Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.21 no.66 Murcia Abr. 2022 Epub 02-Maio-2022
https://dx.doi.org/10.6018/eglobal.483261
Originals
The effect of pandemic on health and Burnout Syndrome in ICU nursing professionals
1 Facultad de Enfermería. Universidad de Jaén. Jaén. España. bmontes@ujaen.es
Introduction:
ICU nurses have a significant risk of BS due to the stressful conditions of their work. The pandemic has worsened these conditions, so these professionals will probably show Burnout Syndrome scores and affectation of their health.
Objective:
Determine the impact on the different health domains and on the performance of their work in nurses who have worked in the ICU in the midst of the COVID19pandemic.
Method:
A cross-sectional descriptive study was carried out. Sixty-eight nursing professionals who had worked in the ICU during the pandemic participated. Each participant completed a booklet with the following scales: Burnout Scale, SF-36 Quality of Life Questionnaire and Somatic Symptom Scale-Revised (ESS-R).
Results:
It has been found that ICU nurses have BS and obtained high scores in each of its dimensions, as well as psychosomatic symptoms, especially in the Musculoskeletal (ME) and Female Reproductive (RF) subscales. On the other hand, the health levels in the different subscales of the SF-36 were not low, but intermediate. Being a woman, having tested positive for covid19, having a family member or friend who has tested positive for COVID19 and being the main caregiver negatively influenced the appearance of BS, health and somatization.
Conclusion:
As a result of the data obtained of the ICU nurses, it is considered that there are compelling reasons that justify the need to establish protocols for psychological action aimed at ICU nurses.
Keywords: Burnout Syndrome; Nurses; Pandemic; covid19; Health; Psychosomatic symptoms
INTRODUCTION
COVID19 is the disease caused by the new coronavirus known as SARS-CoV-2. According to the World Health Organization, the existence of this new virus was first reported on December 31, 2019, when it was informed of a group of cases of "viral pneumonia" that had been declared in Wuhan (People's Republic of China)1).
On 11th March 2020, the WHO officially declared COVID19 disease a pandemic2). In this way, as stated in BOE No. 67, of 03/14/2020, the Spanish Government took the decision to declare the state of alarm for the health management caused by COVID193).
The pandemic affected those people who have struggled on the front lines from the beginning: nurses. Unfortunately, the conditions in which our professionals have worked have been worsening as the pandemic has progressed4). And this was even more pressing in ICU nursing professionals, whose psychological well-being was greatly affected by the stress at work, the lack of protection against contagion and training5). If in itself, nursing work in ICU is especially stressful, given the demands of their work (high specialization)6, rotating night or twelve-hour shifts7) and coping with the frequent death of patients8, these conditions were aggravated with covid19. Specifically, the lack of ventilators referred to by several Spanish autonomous communities9 and the assumption of the consequences of this exceptional situation, such as the increased probability of suffering from various health problems10). In fact, there is evidence to show how nurses have felt11).
Around half of Spanish health personnel were at high risk of suffering from a mental disorder after the first wave, with the most frequent pathologies being disorders of depression, anxiety, panic, post-traumatic stress and substance abuse9). In just six months, the percentage of nursing professionals suffering from SB had grown exponentially, from 8% to 19%12). Moreover, in those ICU nurses in poor physical health or with SB, the probability of making medical errors increased by 60%13). As a result, the level of satisfaction with their profession had fallen in 35% of nursing staff. In fact, 2 nurses out of 10 do not rule out retiring earlier than planned12).
For this reason, the purpose of this study is to explore the existence of SB, psychosomatic symptoms, and health levels in ICU nursing professionals, as well as possible protective or aggravating factors of SB, psychosomatic symptoms and health levels, as a result of the pandemic.
METHOD
Descriptive cross-sectional study. The inclusion criteria were the following: to have the degree of Nursing and have worked in the intensive care unit during the pandemic. It involved 68 ICU nursing professionals aged between 22 and 62 years (M=36.56, SD=11.43). Of the total participants, 79.4% were women and 20.6% were men. 51.5% had no children, 3.2% had one child, 29.4% 2 children and 5.9% had 3 children. Regarding their marital status, 45.6% are single, 50% are married (35.3%) or with a domestic partner (14.7%) and divorced represent 4.4%. The answer "widower" was included as an option, but no one marked it. 27.9% were primary caregivers of a family member. 22.1% of the participants had tested positive for covid19. 86.8% of respondents had acquaintances, family or friends who had tested positive. In relation to the years, they had been practicing as a nursing professional, almost half of the surveyed population (44.10%), had been working as a nursing professional between 2-5 years, followed by those who have been working as a nurse for more than 10 years (32.40%). Of this time, 33.8% of the sample had been working in this service for less than a year, that is, it is understood that this percentage has been hired exclusively during the pandemic4.
Finally, they were asked two control questions to be sure that the entire sample had had direct contact with these patients: a) whether they had had direct contact with covid patients at work, and b) the estimated time caring for covid patients. To the first question, all participants answered affirmatively, with the average time of care for covid patients being 6.33 hours.
The platform used to do the survey was Google Forms. The study was presented to the participants through a telematic link, mostly by WhatsApp groups of nursing trainees who could disseminate the link to nursing professionals who met the inclusion criteria to participate in the study.
The sample responded voluntarily and anonymously to the different scales. Before starting the questionnaire, the information was attached to the participants, where it was stated that they respected the principles of anonymity and voluntariness and informed consent.
The instruments used in this questionnaire were:
Health Questionnaire SF-36 (Vilagut et al., 2020)14. Consisting of 36 items with different subscales (Physical Function, Physical Role, Body Pain, General Health, Vitality, Social Function, Emotional Role and Mental Health). The response format is Likert type of different points according to the subscale (from 1-2 to 1-6). The final score is calculated by adding the pre-coded value of each response.
Maslach Burnout Inventory Scale (Maslach, 1986)15. Composed of 22 items, whose response format used is Likert type of 7 points, being 0 never and 6 every day. The scale consists of three dimensions: Depersonalization, Emotional Fatigue and Personal Fulfillment. The total score or subtotals is done by calculating the average of the items. In the case of Emotional Fatigue and Depersonalization, the higher the score, the greater the signs of Burnout. On the contrary, in Personal Fulfillment, the lower the score, the greater the indication of Burnout.
Revised Somatic Symptom Scale (ESS-R) (Sandín and Chorot, 1995)16. It consists of 90 items. The last 10 items can only be answered if the respondent is a woman. The response format used is 5-point Likert type (from 1, meaning "never during the last year" to 5, meaning "more than once a month"). The higher the score, the greater the frequency the person has suffered from psychosomatic symptoms. The total score is obtained by adding the values marked in each item globally, as well as that of the subscales (9 for women and 8 for men).
Finally, to obtain a more complete view of how nursing professionals had felt this stage on a personal level and to reinforce the hypotheses, they answered three questions of perception about nursing work in the ICU and the difficulty of working in this service in general and during the pandemic. The possible answers to these three questions were "yes" or "no". Specifically, these questions were: a) "Do you consider ICU work to be more delicate than this of other services?"; (b) "Do you think it's easier to have burnout in ICU than in other services?" ;(c) "Do you consider that the life expectancy in people admitted during the pandemic in the ICU has been lower than on other occasions?"
The hypotheses on which this study is based will be followed by an abbreviation and the number that corresponds to it (H, hereinafter).
First, ICU nurses were expected to score high on the SB (H1) scale, as the percentage of nurses suffering from SB has skyrocketed due to the pandemic12. This hypothesis is also justified by the decrease in job satisfaction and the fact that a sample of nurses working in the ICU specialty is studied. As mentioned in the theoretical framework, job satisfaction has a negative relationship with SB17, while working in certain nursing specialties also influences the appearance of SB, the ICU being one of them17,18.
Second, ICU nurses were expected to have low levels of health on the SF-36 (H2) scale subscales. Since it has been shown that the pandemic has had an effect on the health of nursing professionals, it is foreseeable that this effect will also be seen in the nursing staff of this service because they have more stressful conditions10.
Thirdly, nursing professionals were expected to present psychosomatic symptoms based on SS-R (H3), at least in relation to anxiety and depression, since in Spain the main reasons why a mental health professional has been seen have been these two mental disorders19.
The rest of the hypotheses (from H4 onwards), predicted the relationship of certain sociodemographic variables with the appearance of SB, somatic symptoms and low levels of health, since a relationship has been found between some sociodemographic variables with the appearance of diverse effects in health personnel4.
In this way, it is expected that they will present more SB, psychosomatic symptoms and / or worse health in those nurses who meet the following criteria: being a woman (H4), older (H5), being single (H6), greater number of children (H7), being a primary caregiver of another family member (H8), having tested positive for COVID19 (H9), having family members and / or friends who have tested positive for COVID19 (H10), more time in years working as a nurse (H11), more time in years working as a nurse in the ICU (H12), more time caring for covid patients (H13) and more deaths witnessed per day or work shift (H14).
RESULTS
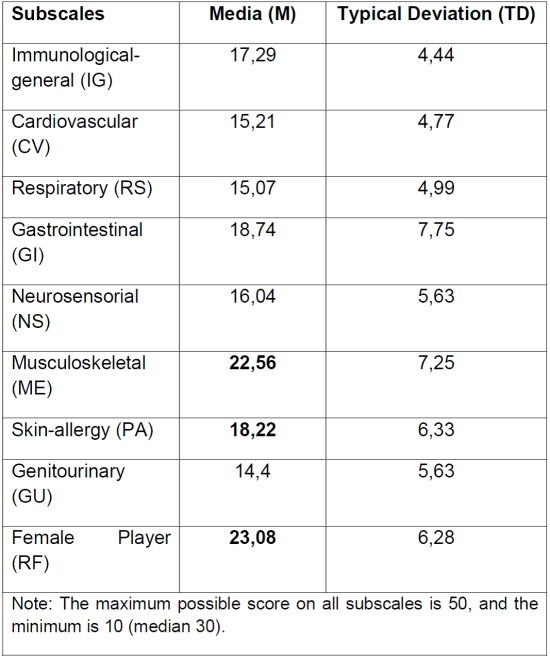
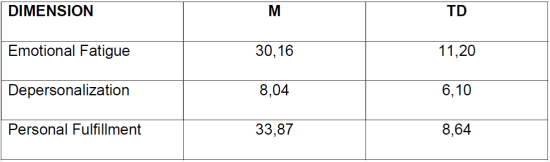
Regarding the scores of the sample in SB and its subscales, the following scores were obtained (Table 1).
Table 1. Means (M) and Typical Deviations (DT) in SB and its subscales: Emotional Fatigue, Depersonalization and Personal Fulfillment.
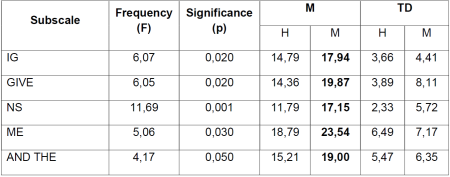
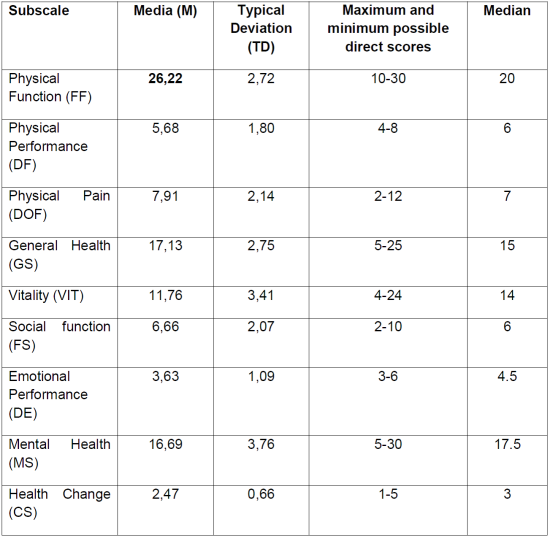
The scores obtained in the subscales of SF-36 (H2) and ESS-R (H3), are described in Table 2 and Table 3.
Table 2. Means (M) and Typical Deviations (TD) and Maximum and Minimum Direct Scores of the SF-36 scale and its dimensions (in bold the scores that distance from the median ±TD).
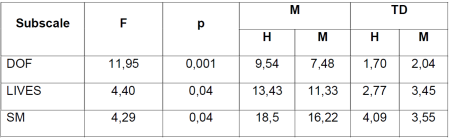
Next, we performed mean difference (ANOVA) analyses of each of the independent variables with the dependent variables. In relation to sex, Table 4 shows the significant differences in several of the SSE-R subscales.
Significant differences were also found in three subscales of the SF-36 questionnaire in relation to sex (Table 5).
Regarding age, significant differences were found in the Respiratory Symptoms (RS) subscale of the ESS-R, F(3, 64)= 3.558; p=0.019. Thus, significant differences were found between 33-42 years and 43-52 years, F(1, 66)= 5,357; p= .020 (M= 13.14, TD= 4.24 vs. M= 5.37; TD= 1.44.
Regarding marital status and the number of children, no significant differences were found. Regarding being a primary caregiver of a relative, significant differences were found in the physical function subscale (FF) of the SF-36, F(1, 66)=6.228; p=0.015, so that ICU nurses who were not primary caregivers of a family member had higher FF scores than those who were (Mno= 26.71; TDno= 2.02 and Myes= 24.95; TDyes= 3.78, respectively.
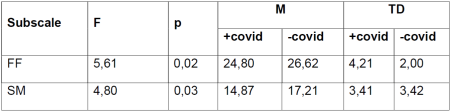
As for whether or not the participant had been positive in covid19, better scores were found in FF and SM (Table 6).
Table 6. ANOVA mean differences in relation to whether or not the nursing professional has been positive in covid19.
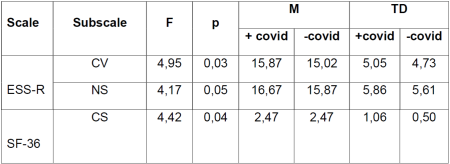
In relation to having a family member and/or friends who had passed covid19, significant differences were found in the following subscales of the ESS-R and SF-36 (Table 7):
Table 7. Differences in ANOVA means in relation to whether or not the nursing professional has family members or friends who have tested positive for covid19.
In relation to the years of service as a nursing professional, significant differences were found in the subscale of Health Change perceived in the last year of the SF-36, F(4, 67)= 3.379; p=0.008, so that the nursing staff who had been less than 2 years showed significant differences, evidencing a greater worsening of their health compared to those who had been more years (2-5 years, p=0.004, M= 3.29, TD= .18; 5-10 years, p=0.005, M= 2.33, TD= .11; more than 10 years, p=0.008, M= 2.36, TD= .10).
Regarding the time in years worked in the ICU, significant differences were found in the Physical Pain subscale of the SF-36, F(4, 67)= 3.375; p= 0.014. Specifically, it was found that nursing personnel who had been working between 5-10 years had greater physical pain, p= .032 (M= 9.87, TD= .53) than those who had been working for 2-5 years (M= 7.27, TD= .41), or less than one year, p = .019 (M= 6.90, TD= .56).
In reference to the estimated time caring for COVID19 patients (H13), significant differences were also found in the Health Change (CS) subscale (F(3, 64)= 4.392; p=0.007). Thus, the nursing staff who had been caring for COVID19 patients between 6 months and one year perceived a greater change in health in the last year with respect to the staff who had been between 3 and 6 months or less than 3 months (p= .015, M= 3.00, TD= .55 vs. M= 2.33, TD= .57 and M= 2.38, TD= .59, respectively).
Finally, significant differences were found in relation to the estimated mean of people who died in ICU per day or shift during the pandemic (H14), in the social function subscale of the SF-36, F(3, 64)= 3.242, p= 0.028. Thus, nursing professionals showed better Social Function the more deaths they had witnessed in their working day, p= .018, M0 =8.20, TD0=1.61, vs. M1= 6.35, TD1=2.04 and M2= 7.07, TD2= 2.02 and M3= 5.85, TD3=1.99, respectively).
Regarding the control questions, 95% of the sample answered that the work in the ICU is more delicate than in other services and 72% that in the ICU it is easier to suffer from SB than in other services. The third question about whether they considered that life expectancy in ICU during the pandemic was lower than on other occasions, 92.6% answered affirmatively.
DISCUSSION
The objective of this study was to describe the impact of ICU nursing professionals in times of pandemic, specifically in the dimensions of Health and Burnout Syndrome. For them, the SF36, ESS-R scales and the Burnout Maslash inventory were used. Taking into account that this affectation could be influenced by some variables, both sociodemographic and exposure and consequences of the pandemic, we took into account and found which of these variables could have worked as protective factors or, on the contrary, as aggravating or risk factors.
In relation to the first hypothesis, the results confirmed this hypothesis. In the Dimension of Emotional Fatigue, the average was well above the cut-off score (30.16 vs >26). In Personal Realization, the average obtained also exceeded the cut-off score (33.87 vs <34). However, in Depersonalization the limit was not exceeded to determine a high degree of depersonalization, but the average is considerably approximated (8.04 vs >9).
ICU nurses perceived a good quality of life7, with the Emotional Performance subscale being the only one with a very low result. This result is consistent with the high scores in Emotional Fatigue. In addition, most of the sample answered that they had had a significant health change since the last year.
Regarding the third hypothesis, it was found that the scores in physical function of the SF-36 were low. However, somatic symptoms were found on almost all scales. Some previous studies explain that the appearance in health professionals of psychosomatic symptoms associated with stress is due to the social idea of the health professional, who is asked for unlimited powers to address problems that are difficult to solve. This produces depersonalization, stress, job dissatisfaction, SB and psychosomatic symptoms in the worker20.
When these somatic symptoms were differentiated by sex, it was found that nurses manifested more immunological-general (GI), gastrointestinal (GI), sensorineural (NS), musculoskeletal (ME) and allergic (PA) somatic symptoms than men. In terms of health, the differences were in the subscales of Physical Pain, Vitality and Mental Health, with women suffering from greater physical pain, less vitality and worse mental health than men. These results are in line with previous studies showing that nurses demonstrate higher anxiety and distress symptoms21.
In relation to the protective or aggravating factors of health and the SB of the nursing staff, it was found that maintaining the family without covid19 positives was a protective factor, while being primary caregivers, having worked in the ICU for more than 5 years, having cared for covid19 patients more than 6 months and witnessing deaths of patients with this disease during their working day were aggravating factors to have or perceive their health worse and / or have more SB.
The physical function of primary caregivers is worse than those who are not primary caregivers as well as for people who had tested positive for covid19 to whom worse mental health was added compared to those who had not been positive.
One of the protective factors against the emotional impact of covid19 is the preservation of the well-being of the family. In this way, nursing professionals with a family member and/or friend who had tested positive for covid19 presented more cardiovascular and sensorineural somatic symptoms, as well as perceiving their current health worse than the previous year. These results were in line with other studies showing the importance of family well-being in the mental health of nursing staff20.
The nursing professionals who perceived worse current health compared to the previous year were those who have worked less than 2 years, compared to those who had been in more years. One possible explanation could be that it takes two years on average to have significant experience in the ICU in the use of nursing techniques and skills to feel more confident in the development of nursing activity22. Thus, professionals who have lived the pandemic in the ICU with less than 2 years of experience would have more stress derived from the situation and therefore greater impact on their health.
According to the years worked in ICU it was also found that the nursing staff showed higher scores of Physical Pain the more years they had been working in this service. This result seems to be in line with studies indicating that the ICU service is one of those related to a higher level of stress23 and, therefore, worsening of pain (specifically, headache and muscle pain)24.
In addition, the perception of health was worse the longer they had been spending, caring for patients with covid19. Specifically, the group of professionals who had been caring for COVID19 patients between 6 months and a year perceived their current health worse than that of the previous year, which took them between 3-6 months and less than 3 months.
Finally, regarding the deaths of patients due to covid19 in their working day, this number significantly affected the social function of ICU nursing staff. The least affected people at the level of Social Function were those who reported 0 deaths per working day and the most affected were those who reported 3 deaths. It is known that the deaths of patients affect nursing staff although the attitudes that professionals adopt in the face of death are diverse; the most common is the approach acceptance (related to religious beliefs, where there is greater confidence and the belief of a happy life after death is present) and neutral acceptance (ambivalence present in the person in the face of the subject of death, expressed in a normal fear of it, but also in its acceptance before its possible arrival)24.
This study is not exempt of limitations. First, the sample of pandemic ICU nurses at the time of the study was small due to the specificity of the sample. Another limitation was that the questions did not appear in a counterbalanced manner to avoid order effects. However, we believe that this has not been a problem in recognizing the importance of the conclusions that have been drawn.
CONCLUSION
After analyzing the results, it is concluded that ICU nurses have SB and high scores in each of the dimensions, as well as present psychosomatic symptoms, especially in the Musculoskeletal (ME) and Reproductive Feminine (RF) sub-wings. On the other hand, health levels in the different subscales, although they have not been low, are referred to as worsening with respect to the last year.
With respect to sociodemographic variables, being a woman, having tested positive for covid19, having a family member or friend who has tested positive for covid19, being a primary caregiver, and the time they have spent caring for covid patients, negatively influence the appearance of SB, health, and somatization.
Thus, given that all the ICU nursing staff in our sample have been in direct contact with covid patients and have spent a lot of time in their care, who present symptoms of SB and worsening of their health, there are compelling reasons that justify the need to establish protocols for psychological action aimed at ICU nursing professionals.
REFERENCIAS
1. Nuevo coronavirus 2019 [Internet]. Who.int. [citado el 30 de mayo de 2021]. Disponible en: https://www.who.int/es/emergencies/diseases/novel-coronavirus-2019?gclid=Cj0KCQjw78yFBhCZARIsAOxgSx2q8CO1atrZDyHv5BiJKvdT2uPOPIrLa95zW7NsMeExEU-SHnx_2hAaAszgEALw_wcB [ Links ]
2. WHO Director-General's opening remarks at the media briefing on COVID19- 11 March 2020 [Internet]. Who.int. [citado el 30 de mayo de 2021]. Disponible en: https://www.who.int/director-general/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 [ Links ]
3. BOE.es - BOE-A-2020-3692 Real Decreto 463/2020, de 14 de marzo, por el que se declara el estado de alarma para la gestión de la situación de crisis sanitaria ocasionada por el COVID19[Internet]. Boe.es. [citado el 30 de mayo de 2021]. Disponible en: https://www.boe.es/eli/es/rd/2020/03/14/463/con [ Links ]
4. Montes- Berges B, Ortúñez Fernández ME. Efectos psicológicos de la pandemia covid 19 en el personal del ámbito sanitario . Enf Global [Internet]. 1 de abril de 2021 [citado 9 de junio de 2021];20(2):254-82. Disponible en: https://revistas.um.es/eglobal/article/view/427161 [ Links ]
5. Carrillo GF. Condiciones de trabajo del personal de Enfermería del Servicio Extremeño de Salud durante la pandemia de COVID en España. NURE investigación: Revista Científica de enfermería 2020(107):5. Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=7616808 [ Links ]
6. Gob.es. [citado el 30 de mayo de 2021]. Disponible en: https://www.mscbs.gob.es/organizacion/sns/planCalidadSNS/docs/UCI.pdf [ Links ]
7. de la Unidad de Cuidados Intensivos del H. U. Valme C de V de LP, Sevilla D. Calidad de vida de los profesionales de la Unidad de Cuidados Intensivos (UCI) del [Internet]. Revistacientificasanum.com. [citado el 30 de mayo de 2021]. Disponible en: https://www.revistacientificasanum.com/pdf/sanum_v4_n3_a1.pdf [ Links ]
8. Rivera DIC, Zambrano LYC, Romero LAL. Actitudes de las enfermeras frente a la muerte de los pacientes en una unidad de cuidados intensivos. Ciencias de la salud 2019;17(3):98-110. Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=7276476 [ Links ]
9. Raurell-Torredà M, Martínez-Estalella G, Frade-Mera M, Rodríguez-Rey LC, de San Pío, E Romero. Reflexiones derivadas de la pandemia COVID-19. Enfermería Intensiva 2020;31(2):90-93. Disponible en: https://www.sciencedirect.com/science/article/pii/S1130239920300389?casa_token=wINMAxr9qNQAAAAA:mITMRGuMSbNE4OH9Pd8DIl52ARQ4X_NWghcqgNvJQhVv4f0LXNEtTSSZTgzldvha0AtNbsMo [ Links ]
10. Pavés Carvajal JR. Occupational hazards and diseases among workers in emergency services: a literature review with special emphasis on Chile. Medwave. 2015;15(7):e6239. Disponible en: https://www.medwave.cl/link.cgi/English/Reviews/GeneralReviews/6261.act?ver=sindiseno?ver=sindiseno [ Links ]
11. Sun N, Wei L, Shi S, Jiao D, Song R, Ma L, et al. A qualitative study on the psychological experience of caregivers of COVID19patients. Am J Infect Control. 2020;48(6):592-8. Disponible en: https://www.sciencedirect.com/science/article/pii/S0196655320302017 [ Links ]
12. Covid19[Internet]. Redaccionmedica.com. [citado el 30 de mayo de 2021]. Disponible en: https://www.redaccionmedica.com/secciones/enfermeria/covid-pandemia-burnout-enfermeras-8270 [ Links ]
13. Las enfermeras con "burnout" cometen hasta un 60% más de errores en UCI [Internet]. Redaccionmedica.com. [citado el 30 de mayo de 2021]. Disponible en: https://www.redaccionmedica.com/secciones/enfermeria/enfermeras-burnout-cometen-mas-errores-uci-5674 [ Links ]
14. Vilagut G, Ferrer M, Rajmil L, Rebollo P, Permanyer-Miralda G, Quintana JM, et al. El Cuestionario de Salud SF-36 español: una década de experiencia y nuevos desarrollos. Gac Sanit. 2005;19(2):135-50. Disponible en: https://www.scielosp.org/article/gs/2005.v19n2/135-150/es/ [ Links ]
15. Researchgate.net. [citado el 30 de mayo de 2021]. Disponible en: https://www.researchgate.net/profile/Christina-Maslach/publication/277816643_The_Maslach_Burnout_Inventory_Manual/links/5574dbd708aeb6d8c01946d7/The-Maslach-Burnout-Inventory-Manual.pdf [ Links ]
16. Sandín B, Chorot P. Escala de Síntomas Somáticos-Revisada (ESS-R). Madrid: Universidad Nacional de Educación a Distancia (UNED)(policopiado) 1995. [ Links ]
17. Vargas C, Cañadas GA, Aguayo R, Fernández R, de la Fuente EI. Which occupational risk factors are associated with burnout in nursing? A meta-analytic study. Int J Clin Health Psychol. 2014;14(1):28-38. Disponible en: https://www.sciencedirect.com/science/article/pii/S1697260014700341 [ Links ]
18. Albaladejo R, Villanueva R, Ortega P, Astasio P, Calle ME, Domínguez V. Síndrome de Burnout en el personal de enfermería de un hospital de Madrid. Revista española de salud pública 2004;78:505-516. Disponible en: https://www.scielosp.org/article/resp/2004.v78n4/505-516/es/ [ Links ]
19. López Montesinos MJ. Consecuencias psicosociales del trabajo en personal de enfermería como indicadores subjetivos de rendimiento desde el enfoque de la gestión de los recursos humanos. Proyecto de investigación: 2010. Disponible en: https://digitum.um.es/digitum/bitstream/10201/10059/1/LopezMontesinos.pdf [ Links ]
20. Ferrán MB, Barrientos-Trigo S. Cuidar al que cuida: El impacto emocional de la epidemia de coronavirus en las enfermeras y otros profesionales de la salud. Enfermería clínica 2021;31:S35-S39. Disponible en: https://www.sciencedirect.com/science/article/pii/S1130862120303028?casa_token=ix_tue3mvpQAAAAA:0X5-s4DNwdftmRDFuV5U5ma0ObRAPCqnTwHQC34GDDjbM2TOX5fhNW_jQlnPj5i5M3IONO0y [ Links ]
21. Roselló M, Andrés SV. Determinación del perfil de enfermería en las unidades de cuidados intensivos cardiológicos según sus competencias. Enfermería en cardiología: revista científica e informativa de la Asociación Española de Enfermería en Cardiología 2012(57):51-58. Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=6294197 [ Links ]
22. Aguado Martín José Ignacio, Bátiz Cano Ainhoa, Quintana Pérez Salomé. El estrés en personal sanitario hospitalario: estado actual. Med. segur. trab. [Internet]. 2013 Jun [citado 2021 Jun 06] ; 59( 231 ): 259-275. Disponible en: http://scielo.isciii.es/scielo.php?script=sci_arttext&pid=S0465-546X2013000200006&lng=es. https://dx.doi.org/10.4321/S0465-546X2013000200006. [ Links ]
23. Blanca-Gutiérrez J.J., Arias-Herrera A. Síndrome de burnout en personal de enfermería: asociación con estresores del entorno hospitalario, Andalucía, España. Enferm. univ [revista en la Internet]. 2018 Mar [citado 2021 Jun 06] ; 15( 1 ): 30-44. Disponible en: http://www.scielo.org.mx/scielo.php?script=sci_arttext&pid=S1665-70632018000100030&lng=es. https://doi.org/10.22201/eneo.23958421e.2018.1.62903 [ Links ]
24. Rivera DIC, Zambrano LYC, Romero LAL. Actitudes de las enfermeras frente a la muerte de los pacientes en una unidad de cuidados intensivos. Ciencias de la salud 2019;17(3):98-110. Disponible en: https://dialnet.unirioja.es/servlet/articulo?codigo=7276476 [ Links ]
Received: June 11, 2021; Accepted: September 14, 2021











 texto em
texto em