Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.21 no.67 Murcia Jul. 2022 Epub 19-Set-2022
https://dx.doi.org/10.6018/eglobal.507341
Originals
A training communication program designed for emergency nurses working at ambulance
1aSchool of Nursing, Faculty of Medicine and Health Science. University of Barcelona. Spain
1bEmergency Unit, Hospital Transfronterer de Cerdanya (ATCE), Camí d'Ur n 12, 17520, Puigcerdà, Girona, Spain
2Research Group GIRISAME (International Researchers Group of Mental Health Nursing Care), Madrid, Spain
3aResearch Group GIESS (Group for Research in Nursing, Educaction, and Society), Barcelona, España
3bResearch Group GEIMAC (Consolidated Group 2014-1139: Group for the Study on Nonvariance of Instruments for Measurement and Analysis of Change in the Social and Health Domains), Barcelona, Spain
Communication is the key to understanding the emotional vulnerability of patients in critical condition. A sudden change in health experienced by these individuals due to an accident or illness can lead to serious psycho-emotional outcomes.
Main objective:
To conduct and evaluate an augmentative alternative communication training program (CONCETEM) for pre-hospital nurses and determine its utility and the satisfaction of the nurses.
Methods:
The study has an observational-descriptive design. The sample was 12 pre-hospital nurses selected by inclusion criteria. Post-training evaluation was conducted by the research team to learn whether nurses could perform the communicative intervention.
Results:
100% of the nurses who underwent CONECTEM training were prepared to implement communicative intervention in the ambulance. 60% of the nurses considered that the training was very useful for improving the quality of care for critically ill patients transferred by ambulance. The nurses' satisfaction with the communication training was ‘very good' for 42.4% and ‘good' for 58.3%.
Conclusions:
The results support the importance of Augmentative Alternative Communication training to improve outcomes in critically ill patients and reveal that nurses feel that more training is needed.
Key words: Communication barriers; critical care; ambulance; nurse-patient relationship
INTRODUCTION
Communication with the critically ill patient is complicated by the environmental, social, physical, and structural barriers that encompass it1,2. The inability to speak as a consequence of mechanical ventilation, exhaustion, weakness, fear, or anxiety all contribute to need to interpret the movement, gestures, and behavior of the patient3,4. Poor communication between the nurse and the critically ill patient generate negative emotions, loss of control, misunderstanding, dependency, and alteration of the perception of the patient, with a direct effect on his or her health 5,6.
The training of nurses in communication techniques has always been at a handicap in the improvement of communication with the patient, and by extension his or her well-being. The first studies made of communication between the nurse and the critically ill patient indicated that nurses relied on verbal communication, with short instructions (less than a minute) concerning the technical procedures to be carried out7. Some nurses have used other techniques such as lip-reading and learning by trial and error. Misunderstandings and poor interpretation generated insecurity and frustration in the nurses and worsened their ability to manage pain8, provide emotional support, and meet the needs of the patient9.
The first quasi-experimental study giving evidence of the effectiveness of communication between the nurse and the patient was carried out by Happ et al.10, with an intervention called SPEACS. This study measured the frequency, quality, ease, and success rate of communication during nurse-critically ill patient interaction. The first training of nurses in this area was carried out by specialists in Augmentative Alternative Communication (AAC). The results of the study opened up a new line of research examining the analysis, application, acceptance, and effectiveness of AAC. Models of AAC were then constructed10,11, with nurses receiving training in the different levels of technology associated with AAC: no technology (basic communication skills (BCS)), low technology (blackboards, drawings, international gestures)12, and high technology (electronic devices and programs)13,14. Also assessed were the implementation and impact of AAC training, and the impediments to its implementation in the intensive care unit (ICU)1,15.
In our review of the literature we turned up no studies that contemplated the training of pre-hospital nurses in medicalized ambulances with AAC. The training of pre-hospital nurses (Emergency Medical Systems--SEM) in AAC was therefore put forward for the present study. The adverse conditions represented by the ambulance constitute an additional difficulty in the task of communicating with the critically ill patient16,17, creating a challenge for the healthcare personnel trying to transmit safety and comfort while accompanying the patient and determining the needs and worries of the individual during transport18.
MAIN OBJECTIVES
To assess a training program in basic communication skills (BCS) and augmentative alternative communication (AAC), CONCETEM for pre-hospital nurses and to learn both the usefulness of the training program and the level of satisfaction of those participating in it.
METHODS
Design
This is a prospective, observational, descriptive study. Training was carried out in BCS and AAC (CONECTEM) with selected nurses, with the goal of fulfilling the aims put forth. A post-test model was used.
Population and sample
The population for the study was all of the active nurses in the Medical Emergency System (SEM) database in Puigcerdà (n 22), in the north of the autonomous region of Catalonia, Spain. The non-probabilistic sample was chosen by the principal researcher according to inclusion and exclusion criteria. 1) Inclusion criteria: Being an active nurse on the Puigcerdà SEM team and working more than four duty-shifts per month. 2) Exclusion criteria: Less than two years' pre-hospital experience and having undergone prior training in AAC. The final sample consisted of 12 nurses (n 12).
CONECTEM program and its development
The CONECTEM training program, is aimed principally at nurses treating critically ill patients. It provides tools and resources to nurses to communicate effectively with the aim of improving the quality of the nursing care provided to critically ill patients, limiting the possible psycho-emotional consequences arising from their situation. The program is organized into 4 blocks, as may be seen in Table 1.
Table 1. Conectem training program
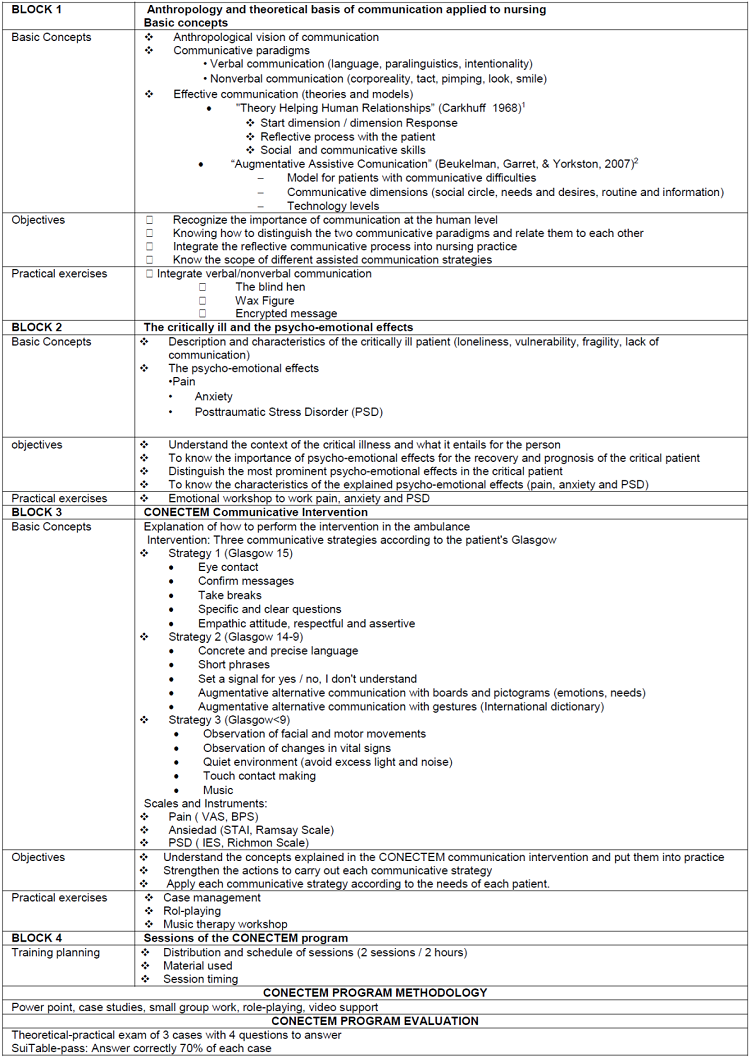
AVS: Analog Visual Scale, BPS: Behavior Pain Scale, STAI: State-Trait Anxiety Scale, IES: Impact Event Scale
1.Beukelman, D, K Garret, y K Yorkston. Augmentative Communication Strategies for Adults with Acute or Chronic Medical Conditions.Baltimore: Paul H Brookes Publishing Co,2007.
2.Carkhuff, R. Helping Human Relations(Vol. 1). New York: Holt, Rineheart and Winston, Inc, 1969.
Instruments
Theoretical-practical test to assess the level of knowledge acquired
The examination consisted of 3 cases with 4 questions each. Two of the questions were closed, and 2 open. In each case answering 3 or all 4 questions correctly indicated that the nurse was prepared.
Questionnaire to determine the usefulness of CONECTEM
A questionnaire was drawn up to measure the following items: the importance of communication prior to the training, new perspectives on communication, broadening of knowledge, incorporation of new techniques, change of attitude towards the patient, improvement in communicative skills, comprehension of psycho-emotional effects, and improvement in care provided. Each variable was assessed with a Likert scale from 1 to 5, with 1 representing ‘none' and 5 ‘a lot'.
Questionnaire on satisfaction with the CONECTEM program
A questionnaire was prepared to measure the following items: materials used, information provided, organization and structure, clarity of explanations and importance of content, participation of the students, relation of theory to practice, satisfactory response to student questions, appropriateness of assessment, and general assessment of the course. Each variable was assessed with a Likert scale from 1 to 5, with 1 representing ‘very deficient' and 5 ‘very good'.
Data collection
In order to carry out the training, three different days were offered to the nurses, to insure that they would be able to attend. The program was made up of 2 sessions of two hours' duration, held in the training room at the Hospital de Cerdanya. At the conclusion of the second session assessment of the training was made by means of the theoretical-practical test. Sociodemographic data and information about the work situation of the nurses was also gathered. Their level of satisfaction with the program was measured with the questionnaire designed to that end, administered by the research team. The usefulness of the training was assessed with an additional questionnaire that was administered at three months' following the program.
Statistical analysis
For the qualitative variables, absolute and relative frequencies in the form of percentages were used, while for the quantitative variables the mean and the standard deviation were used when there was a normal distribution, and the median and the interquartile range when there was not. Data collection was made with a digitized database and analysis was made by means of the statistical package for Windows SPSS v18 (LEAD Technologies, Chicago, Illinois).
Ethical considerations
The project was approved by the Independent Ethics Committee of the Regional University (Spain) INF-2014-17 and by the Board of Directors of the Emergency Medical System (Spain) 20150120_21. The Declaration of Helsinki on ethical principles for medical research involving human subjects guided the study19. Informed consent of the nurses was formalized in order to insure their voluntary participation, the confidentiality of the data collected, and the anonymity of the data. The authors declare there to be no conflicts of interest.
RESULTS
Sociodemographic characteristics of the nurses
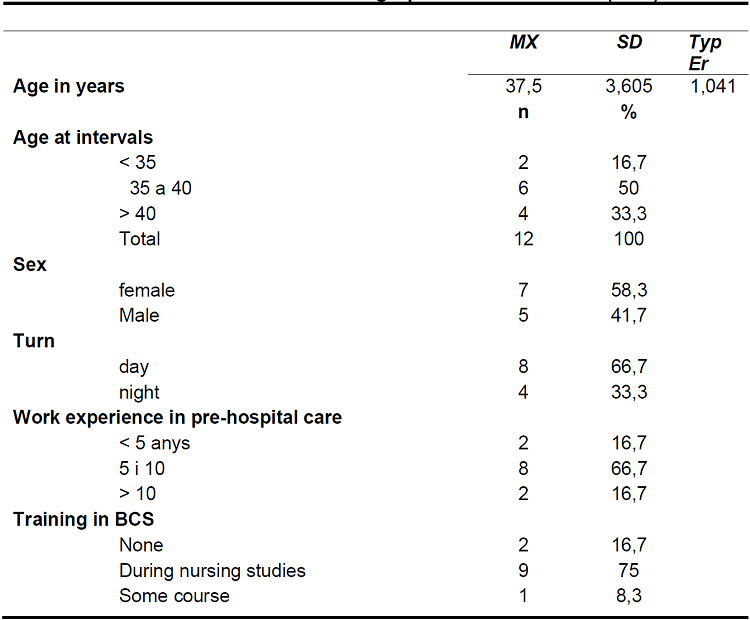
The average age of the participating nurses was 37.5 years. Some 58.3% of the nurses undergoing the communication training were female (n 7). 66.7% were working the day shift. In terms of their work history, 66.7% (n 8) of the nurses had from 5 to 10 years of experience. 75% of them (n 9) had completed a course on basic communication skills during their nursing studies, while 16.7% (n 2) had no prior training in communication (see Table 2).
Aptitude of the pre-hospital nurses in BCS and AAC in the CONECTEM training
All of the nurses participating in the study were prepared to develop their BCS and AAC training in the workplace setting. Most of them responded correctly to the closed questions about the cases: all of them for cases 1 and 3, and 83.3% for case 2. The largest percentage of incorrect responses was in the open reasoning questions: 33.3% for case 1 and 41.7% for case 2. Nevertheless, the prehospital nurses (n 12) who underwent CONECTEM training in BCS and AAC passed the theoretical-practical examination satisfactorily.
Usefulness of CONECTEM training
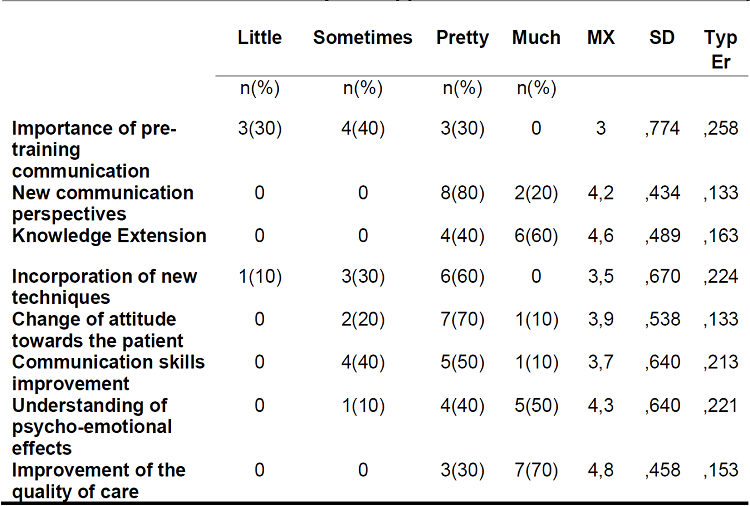
Prior to the training, only 30% of the participating nurses saw communication with the critically ill patient as being important. In contrast, three months after completing the training, 100% of the same nurses felt that the training had opened up new perspectives regarding communication between the nurse and the critically ill patient. Half of the nurses 50% said that the training had helped them greatly in understanding more fully the psycho-emotional effects felt by the critically ill patient, while another 40% felt that it had helped them somewhat. In terms of expanding knowledge about the techniques of communication, 60% said that the training had done so a great deal, while another 40% said that it had done so somewhat. We find the same percentages with respect to the training and improvement in care quality. Some 60% felt that the training had improved the care they provided the critically ill patient greatly, and 40% said that it had done so somewhat. Therefore, we may conclude that the prehospital nurses saw the CONECTEM training program as ranging between somewhat useful and very much so. See Table 3.
Perceived satisfaction with the CONECTEM program
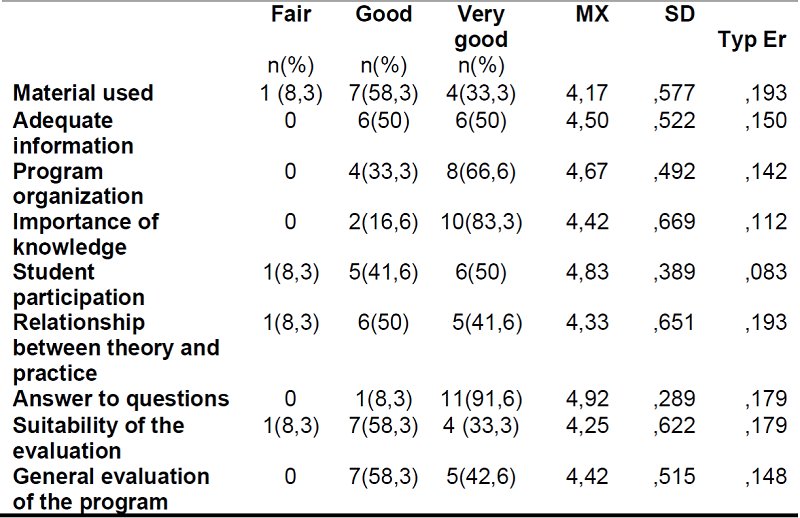
The general assessment of the training was 58.3% good and 42.4% very good. The items seen most favorably were: encouraging student participation, the response of the teacher to questions that arose during the training, and the structure and organization of the course. Of note, all the other variables averaged better than 4/5. Therefore, we may conclude that the satisfaction of the nurses with their program was good. See Table 4.
DISCUSSION
At the outset the nurses participating in the study had a relatively low perception of the importance of communication with the critically ill patient; some 70% (n 7) thought it of little importance or somewhat important. The researchers did not dig deeper to uncover the sources or consequences of this lack of interest, but the reviewed literature indicate that the lack of effective communication between nurse and critically ill patient gives rise to frustration and insecurity in healthcare professionals20 21 22.
Regarding satisfaction with the CONECTEM program, the results indicate that the nurses viewed the methodology used in the program positively, as it encouraged participation by the students. Role-playing and practical case study are two of the most commonly used methods in training programs in communication techniques23,24. The clarification of the concepts and the general evaluation of the program were also very satisfactory (average 4.42/5). It is of note that the training in communication techniques was well received on the part of the nurses. Koszalinski et al.25reported that 41.6% of the nurses in a training program were then able to communicate better with patients, and 100% were inclined to repeat the training experience. Different studies reported that the nurses felt that the training in BCS and AAC was beneficial to them both professionally and personally17 25 26 27.
The results of the present study reveal that the nurses felt that the CONECTEM program was useful (40%) or very useful (60%), in that their improved communication skills meant an improvement in the quality of care provided to critically ill patients. Similar studies in which the nurses participated in in BCT and AAC training also reported that the nurses saw their training as an professional improvement. Koszalinsky et al.28reported that nurses found new techniques learned in their training to be useful, and often used by them. Higginson et al.29concluded in their study that 89% of the nurses participating in the PACE intervention found it to be very useful. Nurses feel greater professional self-confidence when they are able to communicate with their patients. Mehmet et al.23carried out training with emergency service nurses. After the training, their communicative skills (p 0.001), empathy (p 0.001), respect and understanding (p 0.01), and active listening (p 0.03) vis a visthe patient had increased, while their ineffective interactions with patients had decreased by 66%.
In our study the nurses participating in the CONECTEM training believed that the training had opened up new perspectives for them in terms of communicating with critically ill patients, had improved their communicative skills, and had helped them to comprehend the psycho-emotional effects on the critically ill patient (average 4/5). In contrast, the items related with the implementation of the communication techniques had lower scores (average 3/5). Authors who have studied the difficulty in implementing BCS and AAC with the critically ill patient have described barriers encountered by the nurses, including a shortage of time, unfamiliarity with the technology1,15, lack of training, and failure of communication despite having used the techniques that were learned, leading to a certain insecurity in using AAC28.
Limitations
The study has two limitations that must be noted: 1) we did not examine the barriers in the implementation of the training, and their causes. A further study should be carried out to this end; and 2) the representativeness of the sample is limited (n 12), although the other studies reviewed that reported training programs for nurses had from 10 to 22 participants24 29 30.
CONCLUSIONS
The SEM nurses who underwent CONECTEM training based on BCT and AAC were then prepared to apply the new communicative model to their professional lives. All of the nurses felt that the training was useful and that it had improved the care provided to critically ill patients transported in ambulance. The nurses were satisfied with the CONECTEM training, thereby aiding in its future implementation.
Prehospital nurses consider training in BCS and AAC to be useful in helping them communicate more effectively with patients.
Communication programs need to be put in place to improve the quality of care provided to critically ill patients transported in ambulance.
REFERENCIAS
1. Dithole KS, Thupayagale-Tshweneagae G, Akpor OA, Moleki MM. Communication skills intervention: Promoting effective communication between nurses and mechanically ventilated patients. BMC Nurs. 2017;16(1).DOI: 10.1186/s12912-017-0268-5 [ Links ]
2. Norouzinia R, Aghabarari M, Shiri M, Karimi M, Samami E. Communication Barriers Perceived by Nurses and Patients. Glob J Health Sci. 2015;8(6):65-74. DOI: 10.5539/gjhs.v8n6p65 [ Links ]
3. Baumgarten M, Poulsen I. Patients' experiences of being mechanically ventilated in an ICU: A qualitative metasynthesis. Scand J Caring Sci. 2015;29(2). DOI: 10.1111/scs.12177 [ Links ]
4. Guttormson JL, Bremer KL, Jones RM. "Not being able to talk was horrid": A descriptive, correlational study of communication during mechanical ventilation. Intensive Crit Care Nurs. 2015;31(3):179-86. DOI: 10.1016/j.iccn.2014.10.007 [ Links ]
5. Meriläinen M, Kyngäs H, Ala-Kokko T. Patients' interactions in an intensive care unit and their memories of intensive care: A mixed method study. Intensive Crit Care Nurs. 2013;29(2):78-87. DOI:10.1016/j.iccn.2012.05.003 [ Links ]
6. Dithole KS, Sibanda S, Moleki MM, Thupayagale-Tshweneagae G. Nurses' communication with patients who are mechanically ventilated in intensive care: the Botswana experience. Int Nurs Rev. 2016;63(3). DOI:10.1111/inr.12262 [ Links ]
7. Happ MB. Communicating with mechanically ventilated patients: state of the science. AACN Clin Issues. 2001;12(2):247-58. DOI: 10.1097/00044067-200105000-00008 [ Links ]
8. Varndell W, Fry M, Elliott D. A systematic review of observational pain assessment instruments for use with nonverbal intubated critically ill adult patients in the emergency department: an assessment of their suitability and psychometric properties. Vol. 26, Journal of Clinical Nursing. 2017. p. 7-32. DOI: 10.1111/jocn.13594 [ Links ]
9. Radtke JV, Baumann BM, Garrett KL, Happ MB. Listening to the Voiceless Patient: Case Reports in Assisted Communication in the Intensive Care Unit. J Palliat Med [Internet]. 2011;14(6):791-5. Available from: http://www.liebertonline.com/doi/abs/10.1089/jpm.2010.0313 [ Links ]
10. Happ MB, Sereika S, Garrett K, Tate J. Use of the quasi-experimental sequential cohort design in the Study of Patient-Nurse Effectiveness with Assisted Communication Strategies (SPEACS). Contemp Clin Trials. 2008;29(5):801-8. DOI: 10.1016/j.cct.2008.05.010 [ Links ]
11. Patak L, Wilson-Stronks A, Costello J, Kleinpell RM, Henneman EA, Person C, et al. Improving patient-provider communication: A call to action. J Nurs Adm. 2009;39(9):372-6. DOI: 10.1097/NNA.0b013e3181b414ca [ Links ]
12. Happ MB, Baumann BM, Sawicki J, Tate JA, George EL, Barnato AE. SPEACS-2: Intensive care unit "communication rounds" with speech language pathology. Geriatr Nurs (Minneap). 2010;31(3):170-7. DOI: 10.1016/j.gerinurse.2010.03.004 [ Links ]
13. Nilsen ML, Happ MB, Donovan H, Barnato A, Hoffman L, Sereika SM. Adaptation of a communication interaction behavior instrument for use in mechanically ventilated, nonvocal older adults. Nurs Res. 2014;63(1). DOI: 10.1097/NNR.0000000000000012 [ Links ]
14. Handberg C, Voss AK. Implementing augmentative and alternative communication in critical care settings: Perspectives of healthcare professionals. J Clin Nurs. 2018;27(1-2). DOI: 10.1111/jocn.13851 [ Links ]
15. Gropp M, Johnson E, Bornman J, Koul R. Nurses' perspectives about communication with patients in an intensive care setting using a communication board: A pilot study. Heal SA Gesondheid. 2019;24. doi: 10.4102/hsag.v24i0.1162 [ Links ]
16. Togher FJ, Davy Z, Siriwardena AN. Patients' and ambulance service clinicians' experiences of prehospital care for acute myocardial infarction and stroke: A qualitative study. Emerg Med J. 2013;30(11):942-8. DOI: 10.1136/emermed-2012-201507 [ Links ]
17. Ahl C, Nyström M. To handle the unexpected - The meaning of caring in pre-hospital emergency care. Int Emerg Nurs. 2012;20(1):33-41. DOI: 10.1016/j.ienj.2011.03.001 [ Links ]
18. Alm-Pfrunder AB, Falk AC, Vicente V, Lindström V. Prehospital emergency care nurses' strategies while caring for patients with limited Swedish-English proficiency. Vol. 27, Journal of Clinical Nursing. 2018. p. 3699-705. DOI: 10.1111/jocn.14484 [ Links ]
19. WMA. WMA Declaration of Helsinki - Ethical Principles for Medical Research Involving Human Subjects - WMA - The World Medical Association [Internet]. World Medical Association. 2018. Available from: https://www.wma.net/policies-post/wma-declaration-of-helsinki-ethical-principles-for-medical-research-involving-human-subjects/ [ Links ]
20. Momennasab M, Ardakani MS, Rad FD, Dokoohaki R, Dakhesh R, Jaberi A. Quality of nurses' communication with mechanically ventilated patients in a cardiac surgery intensive care unit. Investig y Educ en Enferm. 2019;37(2). DOI: 10.17533/udea.iee.v37n2e02 [ Links ]
21. Finke EH, Light J, Kitko L. A systematic review of the effectiveness of nurse communication with patients with complex communication needs with a focus on the use of augmentative and alternative communication. J Clin Nurs. 2008;17(16):2102-15. DOI: 10.1111/j.1365-2702.2008.02373.x [ Links ]
22. Happ MB, Garrett K, Thomas DDV, Tate J, George E, Houze M, et al. Nurse-patient communication interactions in the intensive care unit. Am J Crit Care. 2011;20(2):1-7. DOI: 10.4037/ajcc2011433 [ Links ]
23. Ak M, Cinar O, Sutcigil L, Congologlu ED, Haciomeroglu B, Canbaz H, et al. Communication skills training for emergency nurses. Int J Med Sci [Internet]. 2011;8(5):397-401. Available from: http://www.pubmedcentral.nih.gov/articlerender.fcgi?artid=3133844&tool=pmcentrez&rendertype=abstract [ Links ]
24. Song MK, Happ MB, Sandelowski M. Development of a tool to assess fidelity to a psycho-educational intervention. J Adv Nurs. 2010;66(3):673-82. DOI: 10.1111/j.1365-2648.2009.05216.x [ Links ]
25. Koszalinski RS, Tappen RM, Melhuish T, Grumme V. Evaluation of a novel communication application from nurses' perspectives. CIN - Comput Informatics Nurs. 2017;35(6):300-6. DOI: 10.1097/CIN.0000000000000322 [ Links ]
26. Happ MB, Sereika SM, Houze MP, Seaman JB, Tate JA, Nilsen ML, et al. Quality of care and resource use among mechanically ventilated patients before and after an intervention to assist nurse-nonvocal patient communication. Hear Lung J Acute Crit Care. 2015;44(5):408-415.e2. DOI: 10.3928/19404921-20140127-02 [ Links ]
27. Kuyler A, Johnson E. Patient and nurse content preferences for a communication board to facilitate dialogue in the intensive care unit. Intensive Crit Care Nurs. 2021 Apr 1;63. DOI: 10.1016/j.iccn.2020.103005 [ Links ]
28. Koszalinski RS, McCarthy JM. Patient communication in the intensive care unit: Background and future possibilities. Vol. 63, Intensive and Critical Care Nursing. 2021. DOI: 10.1016/j.iccn.2020.102955 [ Links ]
29. Higginson IJ, Koffman J, Hopkins P, Prentice W, Burman R, Leonard S, et al. Development and evaluation of the feasibility and effects on staff, patients, and families of a new tool, the Psychosocial Assessment and Communication Evaluation (PACE), to improve communication and palliative care in intensive care and during clinical u. BMC Med. 2013;11(1). DOI: 10.1186/1741-7015-11-213 [ Links ]
30. Nilsen ML, Sereika SM, Hoffman LA, Barnato A, Donovan H, Happ MB. Nurse and Patient Interaction Behaviors' Effects on Nursing Care Quality for Mechanically Ventilated Older Adults in the ICU. Res Gerontol Nurs. 2014. DOI: 10.3928/19404921-20140127-02 [ Links ]
Received: January 26, 2022; Accepted: April 05, 2022











 texto em
texto em