Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.21 no.67 Murcia Jul. 2022 Epub 19-Set-2022
https://dx.doi.org/10.6018/eglobal.503471
Reviews
Health promotion measures in people with diabetes mellitus during covid-19: an integrative review
1Federal University of Paraíba, Paraíba, Brazil
2Federal University of Campina Grande, Academic Nursing Unit, Cuité, Paraíba, Brazil
Objective:
To map scientific evidence on health promotion measures to improve the quality of life of people living with Diabetes Mellitus during the COVID-19 pandemic.
Method:
This is an integrative review, performed in MEDLINE databases via PubMed, CINAHL-Ebsco, Scopus, LILACS and IBECS, using the descriptors "diabetes mellitus", "coronavirus infections", "covid-19", "health promotion” and “quality of life”.The sample counted 17 articles.
Results:
Data were grouped into three dimensions: focusing on the individual; in the community and in government actions or public policies.
Conclusion:
Individual measures were more prevalent in the studies, to the detriment of a limitation of collective and governmental measures.
Keywords: Diabetes Mellitus; Coronavírus Infections; Health Promotion
INTRODUCTION
When configuring itself as a pandemic, theSevere Acute Respiratory Syndrome Coronavirus 2(SARS-CoV-2), represents a global public health emergency, causing collapse in health systems around the world and causing changes in people's lifestyles, especially among the most vulnerable groups and at high risk of mortality from the disease, with Diabetes Mellitus (DM) being a factor that includes subjects in that risk group1,2).
A review of the literature on the subject, pointed out in most of the results of studies, a prevalence of diabetes in patients withCoronavirus Disease(COVID-19), in order to conclude that DM was a prognostic factor for unfavorable outcomes, noting that the prevalence was higher in critically ill patients than in non-serious patients, although the pathophysiological relationship that lead to more serious complications is not clear. among those affected by the disease3.
Therefore, there is evidence that relates to a state of chronic hyperglycemia, others suggest that it is related to inflammatory factors and others point to the use of antidiabetic drugs4.
In this context, differentiated attention between health policies for people with DM is essential, avoiding exposure to COVID-19 as much as possible, in addition to measures that culminate in a reduction in the risk of complications and mortality among those who will contract COVID 19. Despite this need, among the usual challenges for patients with DM in Latin America, the lack of measures, actions, guidelines and specific public policies is pointed out as a present reality even in the face of epidemiological data reflecting a greater risk of mortality from COVID-19 in these patients2.
In this sense, knowing the measures and strategies that aim to promote the health of these subjects during the COVID 19 pandemic, which are being used in different regions of the world, is a relevant and essential factor for rethinking actions with the potential for improvement in living conditions, life and health of this public for the continuous confrontation of the two diseases. Therefore, this study aims to map scientific evidence on health promotion measures to improve the quality of life of people living with DM during the COVID-19 pandemic, with the theoretical perspective of the expanded Health Promotion concept listed in Letter from Ottawa, which brings, in its pillars and potential strategies to address health problems5.
METHODS
This is an integrative review that was developed following the steps: elaboration of the research question; establishment of inclusion and exclusion criteria; search for primary studies; evaluation of included studies; categorization of studies; interpretation of results and synthesis of evidenced results6.
A search was carried out to identify reviews with similar themes, ensuring data exclusivity. The search was guided by the following research question: “What health promotion measures to improve the quality of life of people living with Diabetes Mellitus during the Covid-19 pandemic?”, based on the PICO strategy, whose P refers to the population (people with DM), i intervention/exposure (health promotion practice to improve quality of life) and Co to the outcome/results/context (COVID-19 pandemic).
To operationalize the search, controlled descriptors were selected, after consulting the Descriptors in Health Sciences (DeCS) andMedical Subject Headings(MESH) vocabularies.Table 1presents the descriptors, as well as the strategy adopted in each database.
Table 1. Electronic search strategy. João Pessoa, PB, Brazil, 2021
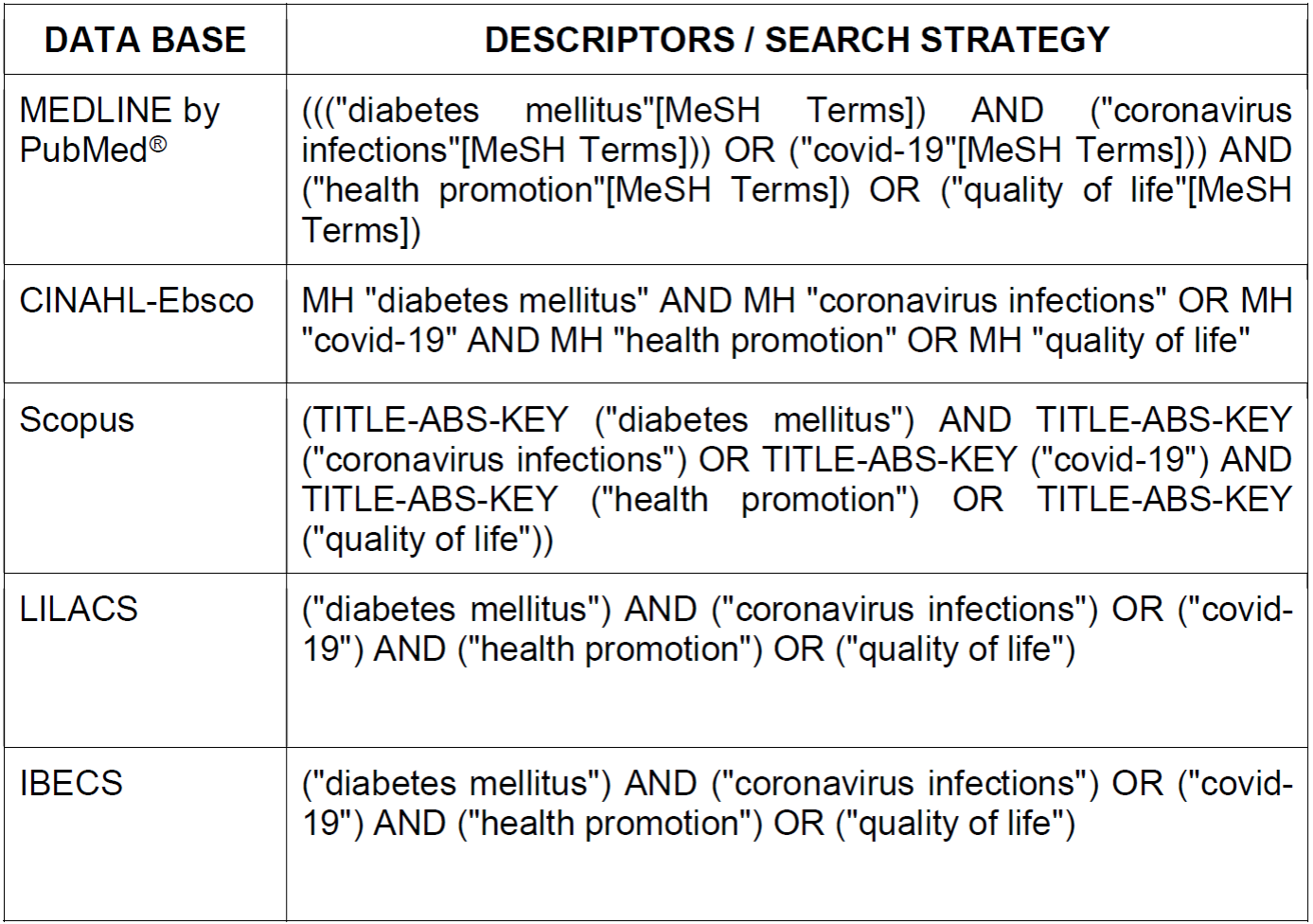
Source: Prepared by the authors, 2021.
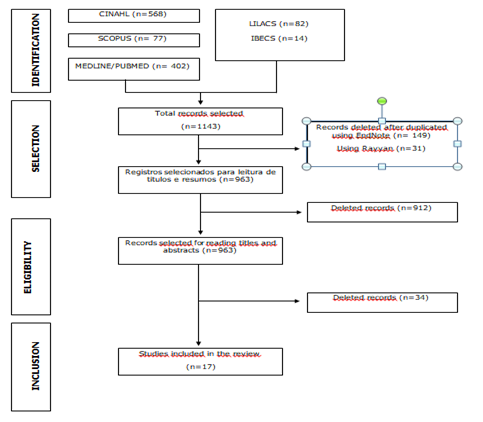
The searches resulted in 1,143 articles. For each database, an export file was generated for theEndNotereference manager, to remove duplications. The selection of the material was made by reading the titles and abstracts, by two independent researchers and blindly, through the free web review programRayyan Qatar Computing Research Institute(Rayyan QCRI), which resulted in 963 articles for the 1st stage of analysis. After this stage, 39 (4.1%) conflicts were identified, therefore, there was a meeting between the two researchers with a third researcher experienced in the area, for their resolution and consensus. Then, in the 2nd stage of analysis, a critical analysis of the articles in their entirety was performed by two independent researchers and blindly, again using theRayyanQCRI. As for the criteria for choosing the articles, experimental, quasi-experimental, observational studies, theoretical reflection, guides and studies published between 2020 and 2021 were included, this time interval was chosen due to the update of evidence on the investigated theme. Experience reports, reports, commentary, integrative and systematic reviews, as well as monographs, dissertations, theses and those articles that did not answer the research question, considering the Covid-19 pandemic context and people with DM and duplicate articles were excluded. The entire process of identification, selection, eligibility and inclusion is shown in Figure 2. It should be noted that the script used for extraction contained information considering the theoretical framework of Dahlgren and Whitehead7, categorizing into individual measures (individuals' lifestyle), collective measures (social and community networks) and governmental measures (living conditions and work).
RESULTS
From the searches carried out in the consulted sources and according to the inclusion and exclusion criteria, a total of 17 articles were included, as shown inFigure 1.
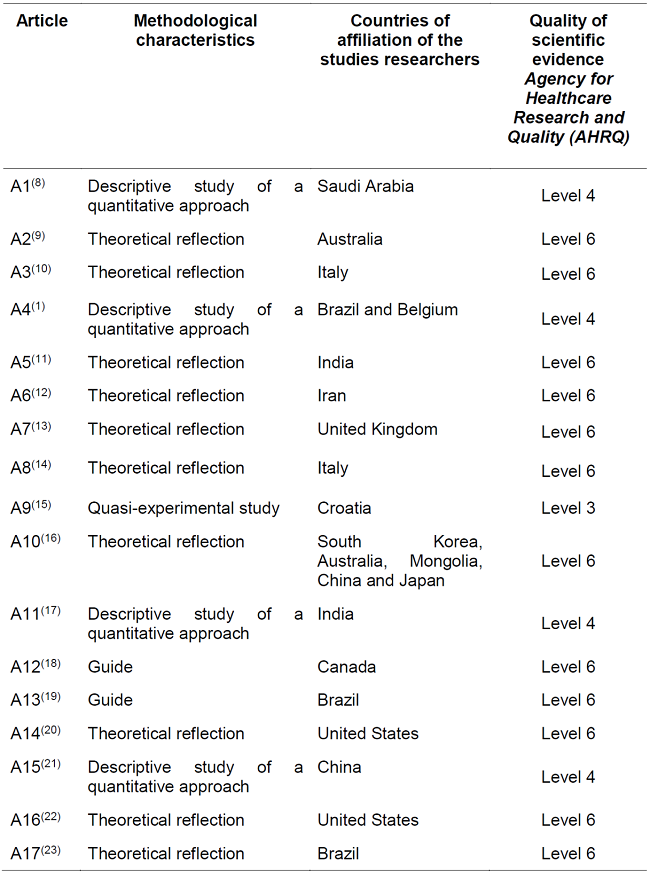
The synthesis of the 17 selected articles is presented inTable 1, which consists of information related to the methodological characteristics and countries of affiliation of the studies researchers.
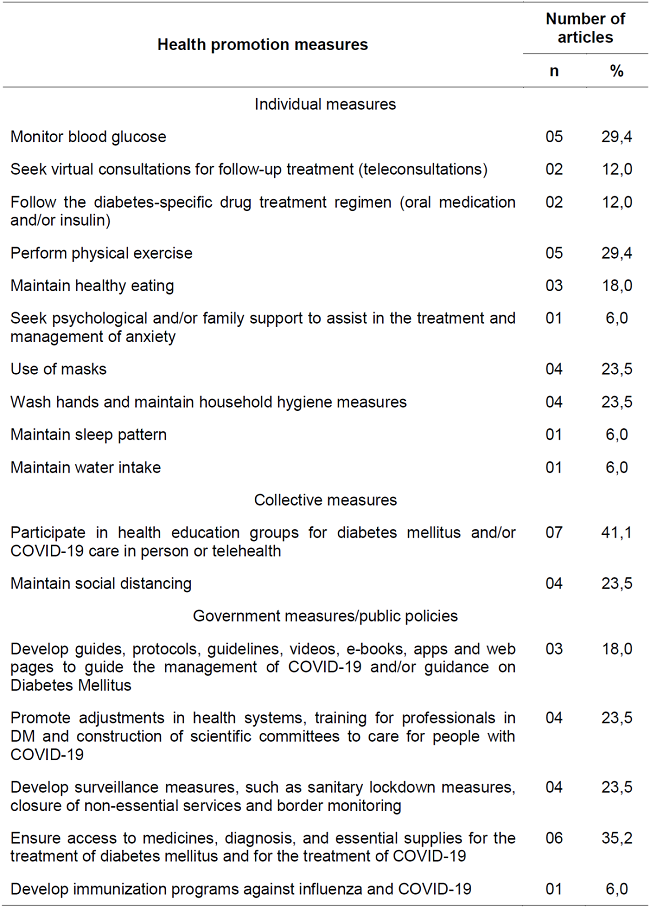
InTable 2, the health promotion measures to improve the quality of life suggested in the articles are presented, being subdivided into: individual measures, collective measures and governmental measures.
DISCUSSION
The studies reveal that individual and collective care measures are being oriented in search of prevention of COVID 19 and injuries in the individual living with DM. With regard to government measures, it is observed that the political response to the pandemic varied according to the institutional design, the autonomy of the political actors involved, and according to the effective belief in the lethal power of the virus23 24.
In this sense, it appears that monitoring glycemic control8 16 19 21 23is essential for people living with DM, since changes in blood glucose, especially hyperglycemia, can cause physiological and immunological disorders25. In addition, hyperglycemia is identified as an aggravating factor of mortality for people with COVID-194,23.
Given the restrictions of social distancing, teleconsultation was a measure used to assist users with DM16,23. This consists of care through the use of technology by the health professional, which allows care without leaving home, for which supplies such as cell phones or computers with the use of the internet are needed26. However, there are potential barriers to be faced, ranging from internet connectivity and user preference for face-to-face meetings with the professional, to availability, technical training and accessibility of subjects to deal with this equipment20.
On the other hand, the popularization of digital tools and the development of guides, protocols and guidelines have been identified as a self-care management strategy for people with DM in the face of the COVID-19 pandemic9-10,23. In view of the reduced access to primary care, diagnostic and hospital services for DM, combined with the fear of exposure to the virus in these places, led to a significant drop in access to usual care9.
Therefore, social distancing is a potential collective measure to prevent infection by Sars-Cov-29 10 14 23. Although recommended by government policies, it seriously affects the treatment of DM, since home confinement limits access to essential services27.
In order to strengthen the distance, actions such as the online prescription of medicines and the delivery of medicines at home by pharmacies are pointed out9. Considering that the drug treatment of people with diabetes consists of the use of antidiabetics and/or insulin, thus, it is recommended to follow the guidelines of health professionals, in order to avoid complications related to DM16,23. In dealing with this problem, there are also recommendations for distributing medications for a prolonged period, in order to avoid going to services23,27.
Regarding the practice of physical exercise, studies point to its relevance in improving glycemic control, pulmonary function, the immune system, accelerating metabolic adaptations, improving cardiorespiratory conditions, decreasing the need for insulin and avoiding secondary complications of DM10 12 18 19 23. Places such as parks, gyms and clubs would be the most suiTable and sought after in non-pandemic situations of COVID-19, but this practice became impossible, requiring other scenarios to carry out these activities27.
In India, recommendations such as climbing stairs, performing domestic activities, gardening and stretching were identified by professionals as activities that can be performed at home and, therefore, easily implemented by people with DM26. Another alternative is the use of online platforms for home exercises, with free classes and specialized instructors10. Regarding healthy eating, studies suggest a balanced diet, composed of proteins, fibers, vitamins, limited saturated fats and hydration18 19 23. A person with DM is more vulnerable to dehydration, so adequate fluid intake must be maintained, being responsible for improving immunity and good kidney function23,28. An unhealthy diet decreases vitamin intake, vitamin D hypovitaminosis is known as a risk factor for insulin resistance, causing endothelial dysfunction and increased platelet aggregation and activation, which predisposes the individual to the development of a hyper-regulable prothrombotic state, which makes them more susceptible to contracting new diseases4.
The use of masks is recommended as an important measure in the prevention of COVID-19, it protects the airways from contact with the virus, being a low-cost measure for the general population12 14 15 23. However, this measure is not enough to provide an adequate level of protection, and other non-pharmacological measures must be adopted, such as hand hygiene12 14 15 23with the use of soap and water to remove dirt or use of 70% alcohol, when it is not possible to use soap and water29.
The literature emphasizes that in the period of the COVID-19 pandemic, people with DM had their sleep pattern impaired, with less than 6 hours of sleep a day, indicating the concern about contracting COVID-19 as a reason, being essential a adequate sleep pattern to keep the body's vital functions sTable22.
Also noteworthy is the participation in health education groups for DM and/or COVID-19 care in person or via telehealth, and health professionals should encourage people living with DM to adhere to virtual means to consultations during the social blockage phase, avoiding exposing the diabetic user, performing only the essentials in person1 8 11 12 15 16 23.
Therefore, the management of DM, as a multifactorial chronic disease, requires access to professionals specialized in the area9 15 16 23. In addition, ensuring that people with the disease can continue to be regularly assisted by their specialized DM health care is essential4.
Considering this, some countries have made adjustments to their health systems1 9 12 23, such as the construction of specialized care centers for COVID-199,23. As well as the remodeling of the healthcare system, with the reconFiguration of wards, separate facilities for those with COVID-19; suspension of non-urgent surgeries and procedures; contact tracing of people exposed to COVID-199. In addition, the development of immunization programs to protect against Covid-19 and influenza23.
In parallel with the aforementioned elements, resources were allocated to preventive, diagnostic and therapeutic regimens for users with DM1 9 12 15)(16(23. And for health professionals, we sought to ensure adequate personal protective equipment2)(9(23.
This study has as a limitation the exclusion of some articles that presented health promotion measures, but not directly related to people with DM.
CONCLUSION
Individual measures were more prevalent in the studies listed in this sample, to the detriment of a limitation of collective and governmental measures. This finding leads us to reflect on the importance of each individual being empowered about the actions they can take in search of their well-being and, consequently, the good of the collectivity. In the case of users with DM, they need to have clarifications and be sensitized about their risk situation in the pandemic, in such a way that they become able to act individually, as well as collectivities and governments must contribute through policies, programs or strategic actions.
REFERENCIAS
1. Barone MTU, Villarroel D, Luca PV, Harnik SB, Lima BLS, Wieselberg RJP et al. COVID-19 impact on people with diabetes in South and Central America (SACA region). Diab Res Clin Pract [Internet]. 2020 Aug [Cited 2021 Apr 01];166. doi: .https://doi.org/10.1016/j.diabres.2020.108301 [ Links ]
2. Arredondo A. The COVID-19 pandemic substantially complicates the usual challenges for patients with diabetes in Latin America. Diab Res Clin Pract [Internet]. 2020 Aug [Cited 2021 May 20];168:108324. doi: https://doi.org/10.1016/j.diabres.2020.108394 [ Links ]
3. Abdi A, Jalilian M, Sarbarzeh PA, Vlaisavljevic Z. Diabetes and COVID-19: A systematic review on the current evidences. Diab Res Clin Pract [Internet]. 2020 Jul 22 [Cited 2021 May 20];166:108347. doi: https://doi.org/10.1016/j.diabres.2020.108347 [ Links ]
4. Cuschieri S, Grech S. COVID-19 and diabetes: The why, the what and the how. JDC (online) [Internet]. 2020 Sep [Cited 2021 Apr 02];34(9):107637. doi: https://doi.org/10.1016/j.jdiacomp.2020.107637 [ Links ]
5. Rabello, LS. Promoção da saúde: a construção social de um conceito em perspectiva comparada. [Internet]. Rio de Janeiro: FIOCRUZ; 2010 [Cited 2021 Apr 02]. p. 228. Available from: http://books.scielo.org/id/z7jxb [ Links ]
6. Mendes KD, Silveira RC, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto Contexto Enferm [Internet]. 2008 [Cited 2021 Apr 02];17(4):758-64. doi: https://doi.org/10.1590/S0104-07072008000400018 [ Links ]
7. Dahlgren G, Whitehead M. Policies and Strategies to promote social equity in health. Stockholm: Institute for Future Studies; 1991. p. 69. [ Links ]
8. Alshareef R, Zahrani AA, Alzahrani A, Ghandoura L. Impact of the COVID-19 lockdown on diabetes patients in Jeddah, Saudi Arabia. Diab Metab Syndr [Internet]. 2020 Sep [Cited 2021 Apr 05];14(5):1583-7. doi: https://doi.org/10.1016/j.dsx.2020.07.05[included in the review] [ Links ]
9. Andrikopoulos S, Johnson G. The Australian response to the COVID-19 pandemic and diabetes - Lessons learned. Diab Res Clin Pract [Internet]. 2020 Jun 02 [Cited 2021 Apr 10];165:108246. doi: https://doi.org/10.1016/j.diabres.2020.108246[included in the review] [ Links ]
10. Balducci S, Coccia EM. Sedentariness and physical activity in type 2 diabetes during the COVID-19 pandemic. Diab Metab Res Rev [Internet]. 2021 Jun 27 [Cited 2021 Apr 10];37(2):14-5. doi: https://doi.org/10.1002/dmrr.3378[include in the review] [ Links ]
11. Chawla M, Jain SM, Kesavadev J, Makkar BM, Viswanathan V, Tiwaskar M et al. Insulinization in T2DM with Basal Analogues During COVID-19 Pandemic: Expert Opinion from an Indian Panel. Diab Ther [Internet]. 2021 Dec 12 [Cited 2021 Apr 16];12(1):133-42. doi: https://doi.org/10.1007/s13300-020-00979-8[include in the review] [ Links ]
12. Dehghan K, Zareipour MA, Zamaniahari S, Azari MT. Tele education in diabetic patients during coronavirus outbreak. Open Access Maced J Med Sci [Internet]. 2020 Dec 25 [Cited 2021 Apr 24];8(T1):610-2. doi: https://doi.org/10.3889/oamjms.2020.5587[include in the review] [ Links ]
13. Fuchs J, Hovorka R. COVID-19 and Diabetes: Could Diabetes Technology Research Help Pave the Way for Remote Healthcare? J Diab Sci Technol [Internet]. 2020 May 30 [Cited 2021 Apr 24];14(4):735-6. doi: https://doi.org/10.1177/1932296820929714[include in the review] [ Links ]
14. Gentile S, Strollo F, Ceriello A. COVID-19 infection in Italian people with diabetes: Lessons learned for our future (an experience to be used). Diab Res Clin Pract [Internet]. 2020 Apr 04 [Cited 2021 Apr 24];162:108137. doi: https://doi.org/10.1016/j.diabres.2020.108137[include in the review] [ Links ]
15. Gvozdanovic Z, Farcic N, Simic H, Buljanovic V, Gvozdanovic L, Katalinic S et al. The impact of education, covid-19 and risk factors on the quality of life in patients with type 2 diabetes. Int J Environ Res Public Health [Internet]. 2021 Feb 27 [Cited 2021 Apr 24];18(5):1-14. doi: https://doi.org/10.3390/ijerph18052332[include in the review] [ Links ]
16. Hwang Y, Khasag A, Weiping J, Jenkins A, Huang C, Yabe D et al. Diabetes and COVID-19: IDF perspective in the Western Pacific region. Diab Res Clin Pract [Internet]. 2020 Jun 24 [Cited 2021 Apr 24];166:108278. doi: https://doi.org/10.1016/j.diabres.2020.108278[include in the review] [ Links ]
17. Jeong IK, Yoon KH, Lee MK. Diabetes and COVID-19: Global and regional perspectives. Diab Res Clin Pract [Internet]. 2020 Jul 02 [Cited 2021 Apr 24];166:108303. doi: https://doi.org/10.1016/j.diabres.2020.108303[include in the review] [ Links ]
18. Kiran T, Moonen G, Bhattacharyya OK, Agarwal P, Bajaj HS, Kim J et al. Managing type 2 diabetes in primary care during COVID-19. Can Fam Physician [Internet]. 2020 Oct [Cited 2021 Apr 24];66(10):745-7. Available from: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7571649/[include in the review] [ Links ]
19. Marçal IR, Fernandes B, Viana AA, Ciolac EG. The Urgent Need for Recommending Physical Activity for the Management of Diabetes During and Beyond COVID-19 Outbreak. Front Endocrinol [Internet]. 2020 Oct 28 [Cited 2021 Apr 24];(11):584642. doi: https://doi.org/10.3389/fendo.2020.584642[include in the review] [ Links ]
20. Monaghan M, Marks B. Personal Experiences With COVID-19 and Diabetes Technology: All for Technology Yet Not Technology for All. J Diab Sci Technol [Internet]. 2020 May 27 [Cited 2021 Apr 24];14(4):762-3. doi: https://doi.org/10.1177/1932296820930005[include in the review] [ Links ]
21. Chunhong S, Haili Z, Jun L, Jian Z, Weihong T. Barriers to self-management of type 2 diabetes during covid-19 medical isolation: A qualitative study. Diab Metab Syndr Obes [Internet]. 2020 Oct 14 [Cited 2021 Apr 24];13:3713-25. doi: https://doi.org/10.2147/DMSO.S268481[include in the review] [ Links ]
22. Sy SL, Munshi MN. Caring for Older Adults With Diabetes During the COVID-19 Pandemic. JAMA Intern Med [Internet]. 2020 Jul 13 [Cited 2021 Apr 24];180:2650-64. doi: https://doi.org/10.1001/jamainternmed.2020.2492. [include in the review] [ Links ]
23. Peixoto TM, Musse JO, Coelho MMP, Silva DC, Nunes IV, Silva ICO. Desafios e estratégias de atenção à saúde de diabéticos no contexto da Covid-19. Rev. Divulg Científica Sena Aires [Internet]. 2020 [Cited 2021 Mai 29];9(3):514-523. doi: https://doi.org/10.36239/revisa.v9.n3.p514a523[include in the review] [ Links ]
24. Schaefer BM, Resende RC, Epitácio SSF, Aleixo MT. Ações governamentais contra o novo coronavírus: evidências dos estados brasileiros. Rev Adm Pub [Internet]. 2020 Sep 24 [Cited 2021 Mai 29];54(5):1429-1445. doi: http://dx.doi.org/10.1590/0034-761220200503 [ Links ]
25. Scott Kruse C, Karem P, Shifflett K, Vegi L, Ravi K, Brooks M. Evaluating barriers to adopting telemedicine worldwide: A systematic review. J Telemed Telecare [Internet]. 2016 Oct 16 [Cited 2021 Mai 29];24(1):4-12. doi: https://doi.org/10.1177/1357633X16674087 [ Links ]
26. Ghosh A, Gupta R, Misra A. Telemedicine for diabetes care in India during COVID19 pandemic and national lockdown period: Guidelines for physicians. Diab Metab Syndr [Internet]. 2020 Apr 04 [Cited 2021 Mai 30];14(4):273-276. doi: https://doi.org/10.1016/j.dsx.2020.04.001 [ Links ]
27. Wicaksana AL, Hertanti NS, Ferdiana A, Pramono RB. Diabetes management and specific considerations for patients with diabetes during coronavirus diseases pandemic: A scoping review. Diab Metabo Syndr [Internet]. 2020 Sep [Cited 2021 Apr 30];14(5):1109-20. doi: https://doi.org/10.1016/j.dsx.2020.06.070 [ Links ]
28. Papadokostaki E, Tentolouris N, Liberopoulos E. COVID-19 and diabetes: What does the clinician need to know? Primary Care Diabetes [Internet]. 2020 [Cited 2021 Apr 24];14(5):558-63. doi: https://doi.org/10.1016/j.pcd.2020.06.010 [ Links ]
29. Silva ÁLDA, Matias LDM, Freitas JMS, Oliveira JCN, Andrade LL. Medidas de prevenção da COVID-19 em pessoas que vivem com diabetes mellitus. REAID [Internet]. 2020 Ago 17 [Cited 2021 Mai 29];93:e020004. doi: https://doi.org/10.31011/reaid-2020-v.93-n.0-art.808 [ Links ]
30. Caballero AE, Ceriello A, Misra A, Aschner P, McDonnell ME, Hassanein M, et al. COVID-19 in people living with diabetes: An international consensus. Journal of Diabetes and its Complications [Internet]. 2020 [Cited 2021 Apr 24];34(9). doi: https://doi.org/10.1016/j.jdiacomp.2020.107671 [ Links ]
Received: December 05, 2021; Accepted: January 04, 2022











 texto em
texto em