Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.22 no.69 Murcia Jan. 2023 Epub 20-Mar-2023
https://dx.doi.org/10.6018/eglobal.529411
Reviews
Nursing diagnosis proposal: risk of vaccination refusal
1University School of Nursing of Cartagena. University of Murcia. Murcia. Spain. franmct15@gmail.com
Introduction:
Vaccination is, nowadays, the best tool for the prevention of diseases in public health, avoiding, thanks to it, around 2 to 3 million deaths annually. However, anti-vaccine movements and their growth put public health at risk, being Nursing one of the most important pieces in the fight against these groups and misinformation.
Objective:
To elaborate a diagnosis proposal that registers the susceptibility to the appearance of vaccination refusal.
Methodology:
A bibliographic search was carried out in different databases (LILACS, ScienceDirect, PubMed, Cochrane and Scopus) to support the creation of the diagnosis on the most recent scientific evidence and with the highest level of quality.
Results:
We propose the creation of the diagnosis "Risk of refusal of vaccination", whose definition is "susceptible to refuse immunization against communicable and/or fatal diseases, putting the user's health and public health at risk".
Discussion:
within Taxonomy II, is included in Domain 11, safety/protection, and in class 5, defensive processes.
Conclusions:
In the absence of a Nursing diagnosis related to vaccination, a process in which nurses play an active role, and in the face of the threat posed by anti-vaccine movements, the diagnosis Risk of refusal of vaccination represents an important advance in the body of nursing knowledge.
Key words: Nursing; vaccination; vaccination refusal; anti-vaccination movement
INTRODUCTION
Vaccines are biological compounds that contain a pathogenic agent, killed or attenuated, and whose administration is intended to generate immunity against that microorganism and, therefore, protect the individual from the disease produced by it 1.
Currently, vaccination is considered the best tool for disease prevention in public health, since vaccines are substances that have shown great efficacy, safety and cost-benefit ratio (2,3. Every year vaccines prevent around 2-3 million deaths, and it is expected that this Figure could increase if vaccination coverage at global level were to improve 4.
However, despite the advantages offered by vaccines, the World Health Organization (WHO) contemplated vaccine reluctance as one of the threats to public health in 20194. WHO defines vaccine reluctance as "delay in accepting safe vaccines or refusal of such vaccines despite the availability of vaccination services." 5
The refusal of vaccination, represented by the so-called anti-vaccination movement, has existed since 1796 when the British researcher Edward Jenner created the world's first vaccine to combat smallpox 6. The arguments on which this movement is based are various: religious, doubts about its effectiveness, fear of its adverse effects, vaccination as an alteration of the balance of the human being, or as a form of government control 7.
The advance of these movements in society can lead to a significant increase in cases of diseases against which vaccines exist or to the reappearance of eradicated diseases. In 2017, a 30% increase in reported cases of measles was reported globally due, in part, to the proliferation of the anti-vaccine movement and the spread of false information about vaccines8.
To combat this phenomenon, WHO advocates the use of information and health education campaigns, strategies where Nursing plays a crucial role. 9 In addition, the International Council of Nurses (ICN) considers that nurses are a key player in the fight against misinformation regarding vaccination, exercising as agents and health leaders in the community, being able to increase confidence in vaccines and being the main source of information regarding health10.
OBJECTIVE
The general objective of this work is to elaborate a proposal for a nursing diagnosis that registers the susceptibility to the appearance of vaccination refusal.
As specific objectives we find:
- To identify a diagnostic label, a definition, risk factors and a population at risk according to the recognized problem.
- To determine nursing outcomes appropriate to the diagnostic proposal.
- To establish nursing interventions appropriate to the nursing diagnosis and the proposed nursing outcomes.
METHODOLOGY
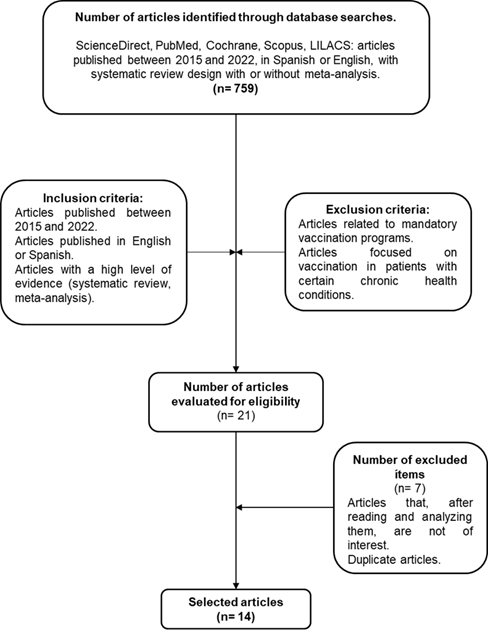
To elaborate this diagnostic proposal, a bibliographic search was carried out in different databases (LILACS, ScienceDirect, PubMed, Cochrane and Scopus), using the DeCS/MeSH: rechazo a la vacunación / vaccination refusal, as well as the following free language terms: vaccination acceptance, vaccination hesitancy. The inclusion criteria established within the search were: articles published between 2015 and 2022, in Spanish or English, and with a high level of evidence (systematic review with or without meta-analysis). On the other hand, the exclusion criteria were: studies conducted on mandatory vaccination programs and articles focused on vaccination in people with chronic diseases.
The search, carried out between May and June 2022, aimed to support the elements that make up the diagnostic proposal (label, definition, risk factors and population at risk) in the most recent scientific evidence.
RESULTS
Following the literature search, a total of 14 articles were used to design the proposal. The results of the search are shown schematically in ILLUSTRATION 1.
NANDA-I defines a risk nursing diagnosis as “clinical judgement concerninig the susceptibility of an individual, family, group, or community for developing an undesirable human response to health conditions/life processes” 11.
Based on this definition, we propose the following diagnosis:
- Label: Risk of vaccination refusal.
- Definition: susceptible to refuse immunization against communicable and/or deadly diseases, putting the user's health and public health at risk.
-
- Risk factors:
Lack of knowledge about vaccines and/or vaccine-prevenTable diseases. The lack of information about vaccines, the receipt of contradictory information from other sources, mostly unofficial or unrelated to the health field, or the receipt of information that is incomprehensible to the user are factors that increase the individual's risk of refusing to vaccinate himself or his children 12,17.
Misinformation or false beliefs about vaccination. Several studies indicate that, as well as lack of knowledge, the presence of misconceptions about vaccines is a risk factor for the occurrence of vaccination refusal 12)(13)(14)(17)(18)(19)(20.
Low perception of the risk of contagion or of the seriousness of the disease. The lack of perception of the risk involved in refusing vaccination, as well as the risk of contracting the diseases that this decision generates, increases the likelihood that the individual will decide not to be vaccinated. It should be noted that, in studies related to the vaccination of children against COVID-19, parents have shown their refusal to be vaccinated because children are often asymptomatic to this disease 12)(13)(15)(17)(18)(19)(20)(21)(22)(23.
Lack of confidence in vaccines. This factor is closely related to lack of information or misinformation, lack of confidence in the health authorities and/or the health system, as well as distrust in relation to the vaccine manufacturing process, especially in the case of recently manufactured vaccines, such as those against COVID-19 13)(19)(21)(23.
Low educational level. Several studies support the relationship between low educational level and refusal of vaccination 13)(15)(16)(17)(18)(19.
Lack of confidence in the healthcare system. This factor encompasses not only confidence in how the system is managed, but also in healthcare professionals and science 13)(14)(16)(17)(18)(20)(23)(24.
Unfavorable socioeconomic status. People living in poorly developed neighborhoods, as well as those whose economic situation is poor, are more likely to refuse vaccination 12)(13)(15)(16)(17)(19.
Fear of the process. The anxiety thatMay be caused by the fact of knowing that the vaccination is performed through a punctureMay be a factor that favors the refusal of the vaccination 12
-
- At-risk populations:
African Ethnicity. People of African descent have less confidence in both vaccines and the health care system. This distrust has its origins centuries ago when black people were exploited for research purposes. Other reasons why people of African descent show more rejection of vaccination are the low level of education in that geographic area, as well as cultural and religious beliefs 13)(15)(16)(18)(22.
Women. Some studies indicate that women are more reluctant to be vaccinated because of rumors about the effects of vaccines on fertility. In addition, in studies of COVID-19 vaccination, women were more reluctant than men because they have a lower tendency to develop serious adverse effects due to SARS-CoV-2 infection than men and a higher likelihood of developing adverse effects from vaccination 12)(13)(16)(20)(22.
Pregnant women. Pregnant women, if they do not receive clear and truthful information about vaccination during pregnancy, are more likely to refuse vaccination 13)(15)(18.
Youth. By not perceiving the risk of not being vaccinated for certain diseases, partly due to the fact that adolescents are not usually a population at risk, as is the case with COVID-19 16)(17)(18)(22
Children whose parents are opposed to vaccination. As they are unable to decide about their health due to their age, children whose parents are negative to vaccination will be at risk of not receiving the relevant immunization 22,25
DISCUSSION
Based on the information extracted from the literature analysis, we can construct the diagnostic label around a multi-axial system, classify it within the NANDA Taxonomy II, as well as relate this diagnostic proposal to nursing outcomes and interventions.
MULTIAXIAL STRUCTURE OF THE DIAGNOSIS
Nursing diagnoses are constituted through a multi-axial system. NANDA-I defines an axis as “a dimension of the human response that is considered in the diagnostic process” 11. The axes used to build the label were:
Axis 1. The focus of the diagnosis. Vaccination refusal. The focus of the diagnosis in this case is "Vaccination refusal", since this is the human response on which action is intended.
Axis 2. Subject of the diagnosis. Individual. However, this diagnosis can also be considered for other subjects, such as a group or a community.
Axis 3. Judgement: Risk of undesirable human response such as refusal to vaccinate.
Axis 7. Status of the diagnosis: Risk. Since it is a diagnosis that registers the susceptibility for the development of a future human response that can cause serious problems, both at the individual and community levels.
CLASSIFICATION IN TAXONOMY II
NANDA-I defines a taxonomy as “a systematic ordering of phenomena/clinical judgments that define the knowledge of the nursing discipline” 11. Within the NANDA Taxonomy II, the diagnosis Risk of Vaccination Refusal would be classified as follows:
-
- Domain 5. Safety/protection.
Class 5. Defensive processes
In addition, within the needs defined by Virginia Henderson, and the functional patterns of Marjory Gordon, this diagnosis would be framed as follows:
- Need 9. Avoid dangers in environment and avoid injuring others.
- Funcional Health Pattern 1. Health perception and management.
NURSING OUTCOMES
A Nursisng-sensitive patient outcome is “an individual, family, or community state, behavior, or perception that is measured along a continuum in response to a nursing intervention(s)”. These are included in the Nursing Outcomes Classification or NOC 24. The proposed Nursing outcomes for the diagnosis Risk of Vaccination Refusal are as follows 25:
[1211] Anxiety level. Severity of manifested apprehension, tension, or uneasiness arising from unidentifiable source.
[1602] Health Promoting Behavior. Personal actions to sustain or increase wellness.
[1603] Health Seeking Behavior. Personal actions to promote optimal wellness, recovery, and rehabilitation.
[1638] Patient’s Engagement. Personal actions to actively participate in health care through shared decision making with health professionals.
[1704] Health Beliefs: Perceived Threat. Personal conviction that a threatening health problem is serious and has potential negative consequences for lifestyle.
[1805] Knowledge: Health behavior. Extent of understanding conveyed about the promotion and protection of health.
[1900] Immunization Behaviour. Personal actions to obtain immunization to prevent a communicable disease.
[1902] Risk Control. Personal actions to understand, prevent, eliminate, or reduce modifiable health threats.
[1924] Risk Control: Infectious Process. Personal actions to understand, prevent, eliminate, or reduce the threat of acquiring an infection.
[2800] Community Immune Status. Resistance of community members to the invasión and spread of an infectious agent that could threaten public health.
[2802] Community Risk Control: Communicable Disease. Community actions to eliminate or reduce the spread of infectious agents that threaten public health.
NURSING INTERVENTIONS
A Nursing intervention is defined as "any treatment, based upon clinical judgement and knowledge, that a nurse performs to enhance patient/client outcomes". 26 Based on this definition, and in order to improve the standards contained in the previously proposed outcomes, we propose the following interventions 25:
[4480] Self-Responsibility Facilitation. Encouraging a patient to assume more responsibility for own behavior.
[5240] Counseling. Use of an interactive helping process focusing on the needs, problems or feelings of the patient and significant others to enhance or support coping, problem solving, and interpersonal relationships.
[5510] Health Education. Developing and providing individual or group instruction and learning experiences to facilitate voluntary adaptation of behavior conducive to health in individuals, families, groups, or communities.
[5520] Learning Facilitation. Promoting the ability to process and comprehend information.
[5820] Anxiety Reduction. Minimizing apprehension, dread, foreboding, uneasiness related to an unidentified source of anticipated danger.
[6530] Immunization Management. Monitoring immunization status and facilitating access to immunizations to prevent communicable disease.
[6610] Risk Identification. Analysis of potential risk factors, determination of health risks, and prioritization of risk reduction strategies for an individual group.
[7330] Culture Brokerage. The deliberate use of culturally competent strategies to bridge or mediate between the patient’s culture and the biomedical health care system.
[7970] Health Policy Monitoring. Surveillance and influence of government and organization regulations, rules, and standards that affect nursing systems and practices to ensure quality care of patients.
[8500] Community Health Development. Assisting members of a community to identify a community’s health concerns, mobilize resources, and implement solutions.
[8820] Communicable Disease Management. Working with a community to decrease and manage the incidence and prevalence of contagious diseases in a specific population.
CONCLUSION
With the presence of a threat to public health such as the anti-vaccine movement and its growth in recent years, the need arises, from Nursing, to collect this phenomenon within the body of knowledge that defines us as a profession, as well as to recognize and systematize those activities that as professionals we can carry out to curb these phenomena.
Moreover, since there is no Nursing diagnosis related to vaccination, a process in which Nursing plays a very important role, it is necessary to have one that records a human response on which nurses can act.
For this reason, we propose the diagnosis Risk of refusal of vaccination, through which we define what this phenomenon means for Nursing, as well as identifying some nursing outcomes and activities that allow us to intervene on patients presenting this diagnosis. In addition, a number of risk groups are recognized as being more susceptible to this phenomenon, such as women, pregnant women, people of African origin, young people, and children whose parents are opposed to vaccination.
REFERENCIAS
1. Forcada Segura JA. Generalidades de las vacunas. Asociación Española de Vacunología [Online]. 2019 [accessed 29 May 2022]. Available at: https://www.vacunas.org/generalidades/ [ Links ]
2. León Gómez VE, Rebollo García L, Rincón Elvira EE, García Murciego MEG. Reticencia vacunal y sus repercusiones: revisión bibliográfica. SANUM [Online]. 2020 [accessed 30 May 2022];4(2):14-27. Available at: https://revistacientificasanum.com/pdf/sanum_v4_n2_a3.pdf [ Links ]
3. Valenzuela MT. Importancia de las vacunas en salud pública: hitos y nuevos desafíos. Revista Médica Clínica Las Condes [Online]. 2020 [accessed 30 May 2022];31(3):233-239. Available at: https://www.elsevier.es/es-revista-revista-medica-clinica-las-condes-202-pdf-S0716864020300407 [ Links ]
4. Organización Mundial de la Salud. Ten threats to global health in 2019. Organización Mundial de la Salud [Online]. 2019 [accessed 30 May 2022]. Available at: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 [ Links ]
5. Jasarevic T. Reticencia a la vacunación: Un desafío creciente para los programas de inmunización. Organización Mundial de la Salud [Online]. 2015 [accessed 28 May 2022] Available at: https://www.who.int/es/news/item/18-08-2015-vaccine-hesitancy-a-growing-challenge-for-immunization-programmes [ Links ]
6. Aparicio Rodrigo M. Antivacunas: un reto para el pediatra. Rev Pediatr Aten Primaria [Online]. 2015 [accessed 30 May 2022];17:107-17. Available at: https://scielo.isciii.es/pdf/pap/v17n66/01_editorial.pdf [ Links ]
7. Fernández P, Jaramillo Carolina. Movimiento anti-vacunas: vacunar o no a nuestros hijos. Revista OACTIVA UC Cuenca [Online]. 2019 [accessed 28 May 2022];4(Especial):47-54. Available at: https://oactiva.ucacue.edu.ec/index.php/oactiva/article/view/406/552 [ Links ]
8. Organización Mundial de la Salud. Un nuevo informe muestra que los casos de sarampión aumentan a nivel mundial debido a una cobertura vacunal insuficiente. Organización Mundial de la Salud [Online]. 2018 [accessed 30 May 2022]. Available at: https://www.who.int/es/news/item/29-11-2018-measles-cases-spike-globally-due-to-gaps-in-vaccination-coverage [ Links ]
9. Organización Mundial de la Salud. COVID-19 and mandatory vaccination: Ethical considerations and caveats. Organización Mundial de la Salud [Online] 2021 [accessed 30 May 2022]. Available at: https://apps.who.int/iris/bitstream/handle/10665/340841/WHO-2019-nCoV-Policy-brief-Mandatory-vaccination-2021.1-eng.pdf?sequence=1&isAllowed=y [ Links ]
10. Consejo Internacional de Enfermeras. Declaración del Consejo Internacional de Enfermeras sobre la vacunación contra la COVID-19. Consejo Internacional de Enfermeras [Online]. 2022 [accessed 30 May 2022]. Available at: https://www.icn.ch/system/files/documents/2022-02/ICN%20Statement%20COVID-19%20Vaccination%20%E2%80%93%20Nurses%20lead%20the%20way_SP_1.0.pdf [ Links ]
11. NANDA International. Nursing DIagnoses. Definitions and Classification 2018-2020. Thieme. 11th edition. 2019 [accessed 11 June 2022]. p. 77, 104, 191. [ Links ]
12. Cadeddu C, Castagna C, Sapienza M, Lanza TE, Messina R, Chiavarini M, et al. Understanding the determinants of vaccine hesitancy and vaccine confidence among adolescents: a systematic review. Hum Vaccin Immunother [Online]. 2021 [Accessed 31 May 2022];17(11):4470-86. Available at: https://pubmed.ncbi.nlm.nih.gov/34473589/ [ Links ]
13. Truong J, Bakshi S, Wasim A, Ahmad M, Majid U. What factors promote vaccine hesitancy or acceptance during pandemics? A systematic review and thematic analysis. Health Promotion International [Online]. 2022 [accessed 31 May 2022];37(1). Available at: https://academic.oup.com/heapro/article/37/1/daab105/6318107 [ Links ]
14. Roy DN, Biswas M, Islam E, Azam MS. Potential factors influencing COVID-19 vaccine acceptance and hesitancy: A systematic review. PLoS ONE [Online]. 2022 [accessed 10 June 2022];17(3). Available at: https://journals.plos.org/plosone/article?id=10.1371/journal.pone.0265496 [ Links ]
15. Adeyanju GC, Engel E, Koch L, Banzinger T, Shahid IBM, Head MG, et al. Determinants of Influenza vaccine hesitancy among pregnant women in Europe: a systematic review. Eur J Med Res [Online]. 2021 [accessed 10 June 2022];26:116. Available at: https://link.springer.com/content/pdf/10.1186/s40001-021-00584-w.pdf [ Links ]
16. Wake AD. The Willingness to receive COVID-19 vaccine and its associated factors: "vaccination refusal could prolong the war of this pandemic" - a systematic review. Risk Manag Healthc Policy [Online]. 2021 [accessed 26 June 2022];14:2609-2623. Available at: https://pubmed.ncbi.nlm.nih.gov/34188572/ [ Links ]
17. Shakeel CS, Mujeeb AA, Mirza MS, Chaudhry B, Khan SJ. Global COVID-19 vaccine acceptance: A systematic review of associated social and behavioral factors. Vaccines [Online]. 2022 [accessed 26 June 2022];10(1):110. Available at: https://www.mdpi.com/2076-393X/10/1/110 [ Links ]
18. Yasmin F, Najeeb H, Moeed A, Naeem U, Asghar MS, Chughtai NU, et al. COVID-19 Vaccine Hesitancy in the United States: A Systematic Review. Front. Public Health [Online]. 2021 [accessed 31 May 2022];9. Available at: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC8650625/pdf/fpubh-09-770985.pdf [ Links ]
19. Wang Y, Liu Y. Multilevel determinants of COVID-19 vaccination hesitancy in the United States: A rapid systematic review. Prev Med Rep [Online]. 2022 [accessed 31 May 2022];25. Available at: https://pubmed.ncbi.nlm.nih.gov/34934611/ [ Links ]
20. Nehal KR, Steendam LM, Campos Ponce M, van der Hoeven M, Smit GSA. Worldwide Vaccination Willingness for COVID-19: A Systematic Review and Meta-Analysis. Vaccines [Online]. 2021 [accessed 31 May 2022];9:1071. Available at: https://www.mdpi.com/2076-393X/9/10/1071 [ Links ]
21. Nolte F, Pacchiotti A, Castellano V, Lamy P, Gentile Á. Reticencia a la vacunación: abordaje de su complejidad. Rev Hosp Niños [Online]. 2016 [accessed 31 May 2022];60(268):16-22. Available at: https://pesquisa.bvsalud.org/portal/resource/pt/biblio-1103478 [ Links ]
22. Galanis P, Vraka I, Siskou O, Konstantakopoulou O, Katsiroumpa A, Kaitelidou D. Willingness, refusal and influential factors of parents to vaccinate their children against the COVID-19: A systematic review and meta-analysis. Preventive Medicine [Online]. 2022 [accessed 10 June 2022];157(1). Available at: https://www.sciencedirect.com/science/article/pii/S0091743522000421?pes=vor [ Links ]
23. Sheldenkar A, Lim F, Yung CF, Lwim MO. Acceptance and uptake of influenza vaccines in Asia: A systematic review. Vaccine [Online]. 2019 [accessed 26 June 2022];37(35):4896-4905. Available at: https://pubmed.ncbi.nlm.nih.gov/31301918/ [ Links ]
24. Larson HJ, Clarke RM, Jarrett C, Eckersberger E, Levine Z, Schulz WS, et al. Measuring trust in vaccination: A systematic review. Hum Vaccin Immunother [Online]. 2018 [accessed 31 May 2022];14(7):1599-609. Available at: https://pubmed.ncbi.nlm.nih.gov/29617183/ [ Links ]
25. Díaz Seoane M, Berbel Hernández C, Allué Tango M, García Rodriguez C, Sanz López P, Pérez Martín MI, et al. Factors related to parents' decision not to vaccinate their children. Vacunas [Online]. 2020 [accessed 31 May 2022];21(1):4-10. Available at: https://www.sciencedirect.com/science/article/pii/S2445146020300054 [ Links ]
26. Moorhead S, Johnson M, Maas ML, Swanson E. Nursing Outcomes Classification (NOC). ELSEVIER. 5th edition. 2013 [accessed 18 June 2022]. p. 3. [ Links ]
27. NNNConsult. Herramienta online para la consulta y diseño de Planes de Cuidados de Enfermería. ELSEVIER [Online]. 2021 [accessed 18 June 2022]. Available at: https://www.nnnconsult.com/ [ Links ]
28. Butcher HK, Bulechek GM, McCloskey J, Wagner CM. Nursing Intervention Classification (NIC). Elsevier. 7th edition. 2018 [accessed 18 June 2022]. p. 3. [ Links ]
Received: June 27, 2022; Accepted: September 26, 2022











 texto em
texto em