Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.22 no.72 Murcia Out. 2023 Epub 04-Dez-2023
https://dx.doi.org/10.6018/eglobal.558771
Originals
Psychoeducational intervention for weight control in pregnant women
1Departamento de Enfermería y Obstetricia. Universidad de Guanajuato. México
2Facultad de Enfermería. Universidad Autónoma de Nuevo León. México
3Facultad de Psicología. Universidad Autónoma de Nuevo León. México
Introduction:
To control gestational obesity, it is necessary to design and implement interventions to improve the quality of diet and physical activity. The objective of the study was to evaluate the efficacy of a psychoeducational nursing intervention for the control of gestational weight in Mexican pregnant women.
Methods:
quasi-experimental study. The sample consisted of 34 participants; n1=17 y n2=17. The psychoeducational intervention consisted of 12 sessions, which included educational, cognitive behavioral techniques and prenatal yoga, for eight weeks. The control group received routine care and a prospectus additional healthy nutrition. We realized anthropometric measurements before and after the intervention, as well as the retention rate in the intervention and the satisfaction of the participants.
Results:
Pregnant women who participated in the intervention had less gestational weight gain than those in the control group ( D̅1 = 5.17 ± 3.01 vs. ( D̅2 = 8.03 ± 4.06; t = -2.32, gl = 32, p = .026). The intervention was feasible, given that 80% complied with the scheduled sessions and satisfactory acceptability, 76.5% of the participants mentioned that the quality of the program was excellent and 100% mentioned that they received the help they expected.
Conclusion:
The psychoeducational intervention favors gestational weight control in the experimental group compared to the control group. Psychoeducational interventions are recommended for the management of weight gain during pregnancy.
Key words: Body Weight; Pregnancy; Controlled Before-After Studies
INTRODUCTION
Nowadays maternal obesity is considered as a severe public health problem. Nearly 50% of women start their pregnancy with a body weight higher than the recommended, and 50% gain excessive weight in the process (1). In Mexico, obesity rates for fertile age women are higher than in the rest of the world. Exceeding the ideal weight during pregnancy can produce multiple complications, both for the pregnant woman and the baby, even increases the chance of death (3,4).
Different authors explain the interaction of modifiable and non-modifiable risk and protection factors related to the risk in not keeping an ideal weight (5,6,7,8).
To eradicate or control this problem, there have been developed interventions. The most common include educational and behavioral, which focus on improving eating and physical activity habits (9). Those ones, though, have a limited success to control excessive gestational body weight. Psychoeducational interventions, on the other hand, seem to be the most effective, although they have been little used for weight control in pregnant women. These ones focus on the establishment of objectives, problem resolution and motivational interview combined with changes in eating behaviors and physical activity (10).
At this moment, there are no reports of psychoeducational interventions with prenatal yoga, meditation and other complementary techniques to control emotional symptoms and in turn, the body weight. These complementary techniques have been used by themselves or with conventional drugs for the control of emotional problems, like prenatal yoga to decrease depression symptoms, anxiety, and pregnancy stress (11).
To apply the intervention, the base was the assumptions of the Health Promotion Model (HPM). This model has been used to turn non-healthy behaviors into healthy behaviors, both for explicative and predictive studies. Specifically, this model has been useful for the designment and implementation of behavioral, educational, and psychoeducational interventions for weight control, healthy eating habits, physical activity, and other topics (13,14).
Therefore, the objective of this research was to evaluate the efficiency of a psychoeducational intervention for gestational body weight in pregnant Mexican women. The second objective was to identify the feasibility and acceptability of a psychoeducational intervention.
MATERIALS AND METHODS
The study design was quasi-experimental, pretest and posttest measurements with two groups. The selected population were pregnant women who received prenatal attention in Nuevo Leon Metropolitan Area. The sampling was considered non-probabilistic because the chosen participants attended to three Child Development Centers. The data collection started on February 2017, and finalized on December 2017. The data analysis ended on May 2018.
Criteria selection
Inclusion criteria: Women older than 18 years of age on their first trimester of pregnancy and with a medical opinion. This opinion shared information about the mother’s health status and states the participant does not have physical or mental health problems that do not make her able to participate.
Exclusion criteria: Pregnant women with threatened abortion, twin pregnancy, participants in other intervention on obesity prevention in pregnancy in the last month.
Elimination criteria: women with less than 70% of attendance in the intervention program.
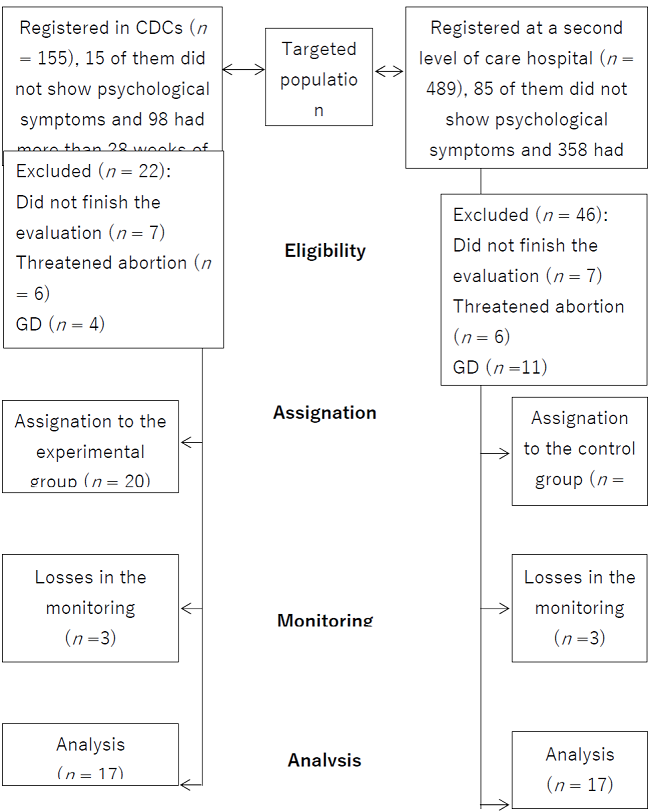
The Figure 1 shows the distribution of the participants selection for the intervention and control group considering quasi-experimental criteria.
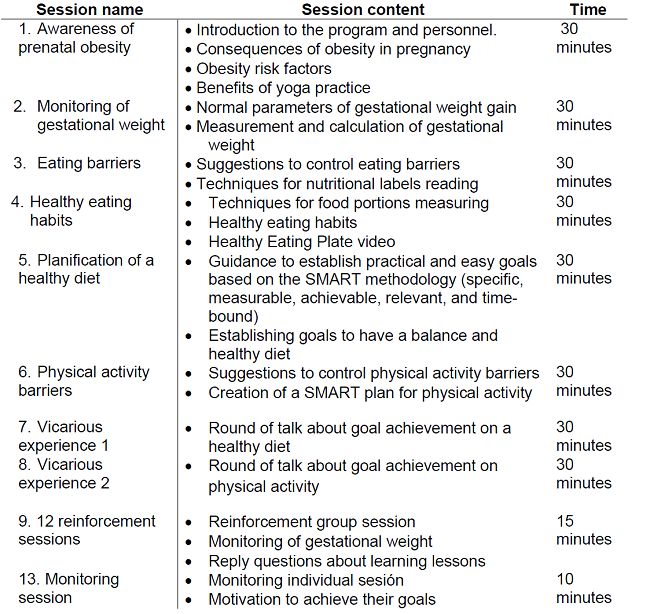
The experimental group received 13 sessions divided into 8 for learning, 4 for reinforcement and 1 for monitoring. These were given twice a week, in groups of 6 to 8 members for 2 months. In Table 1 it is possible to find the name and activities per session. To ensure credibility, guides for the enabler and the participant were designed (15),16). The control group received routine care and an educational session about nutrition.
The study was realized in compliance with the General Health Law in matter of Health Research. Approved by the Ethics and Research Committee of the UANL Nursing School, registration number FAEN-M-1251.
Data was captured and analyzed through the Statistical Package for the Social Sciences (SPSS) version 20 for Windows. 34 participants were analyzed (n1 = 17; n2 = 17). Descriptive and inferential statistics were obtained. The calculation for the normality starting off the valuation data was made through the Kolmogorov-Smirnov Goodness-of-Fit test, corrected by Lilliefors. The results were interpreted as major when the level of statistical significance was .05 or less.
The attendance and satisfaction of the participants was considered to assess the feasibility of the intervention. The satisfaction of the intervention was measured with the Client Satisfaction Questionnaire (CSQ-8) (17).
Anthropometrical measurements (weight and height) were made. Total gestational weigh gain (GWG) was obtained by calculating the difference between the pregestational weight and the current weight. The GWG was classified as low, normal, and high, considering the pregestational body mass index, the gained weight, and the recommended weight according to the gestation week, based on the Institute of Medicine (18).
RESULTS
Both the experimental group (n1) and the control group (n2) had 17 participants. In both groups most of the sociodemographic characteristics were similar.
Table 2. Clinical and sociodemographic baseline characteristics among the participation groups.
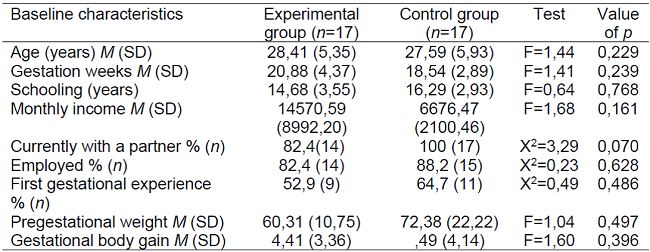
Note:M=mean; SD= standard deviation; X2= Ch square test; F= Analysis of Variance Test (ANOVA).
In relation to the feasibility, the percentage of women who stayed in the program was acceptable, 85% (19). On the attendance, 70% of the participants complied with all the scheduled sessions.
According to the satisfaction of the intervention, 76.5% declared the quality of the program was excellent, and 100% mentioned they felt satisfied with the support they received. Overall, they felt satisfied with achieving change, especially on dietary intake.
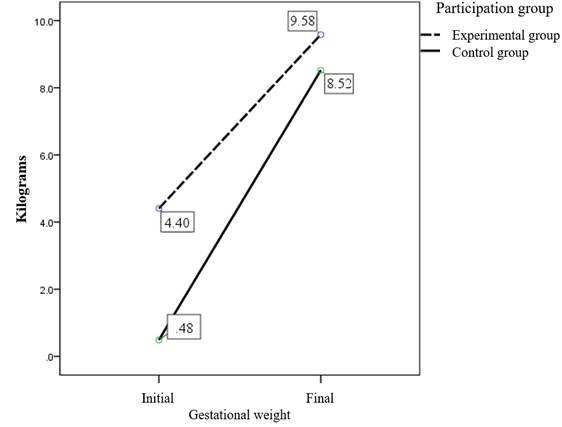
To show the efficacy of the intervention, it was possible to find a significant mean difference in gestational weight gain. The pregnant women from the experimental group showed less increase of gestational weight after the intervention than the control group ( D̅1 = 5,17 ± 3,01 vs. ( D̅2 = 8.03 ± 4,06; t = -2,32, gl = 32, p = ,026), respectively (Figure 2).
DISCUSSION
This study found that applying a psychoeducational intervention based on Pender's Health Promotion Model has an important influence on weight control in those women who received the intervention, compared to those who did not. These results are consistent with other studies where weight control and personalized diets, exercising, psychological evaluation and information about healthy lifestyles were also included(19),(20). Yet, it remains different to other studies with smartphones among their tools (21,22). The provided data about parameters supposed to increase in pregnancy and the risks in the mother and the baby that excessive body weight can lead to could have raised awareness and motivation in the participants to try to get their weight into the ideal parameters. Additionally, pregnancy months are a learning stage; a moment in life when women can be more willing than ever to learn everything about pregnancy and try to improve their health for their baby to be born in good health as well.
According to the feasibility and satisfaction of the intervention, the intervention had an acceptable feasibility, consistent facts with other authors (19,23). This paper had an accepTable intervention and complied with the participants' expectations. The design for the guides for the enabler and the participant might have made the implementation of the sessions easier.
Studies about feasibility of an intervention are a determinant factor to evaluate efficacy. Therefore, it is important to consider the external validity of the interventions with high chance of efficacy and previous feasibility to try their effect with a study design with a greater methodological rigor (24,25). Then, it would be important to think about the internal and external validity of this intervention and include intervention strategies based on the HPM, particularly on the development of behavioral activities related to the barriers and self-efficacy, as well as adding prenatal yoga.
One of the limitations took place when recruiting pregnant women in the first trimester, which was more difficult than expected. Many women go to their prenatal care appointment in their last trimester or when there is a health risk for them or their babies, and some of them declared their time was limited. An important barrier for attendance was the lack of self-control on their work times or their partners’. In the last sessions, the weather was also an uncontrollable factor, as two rainy days were the cause for unattendances and participants being late.
CONCLUSIONS
It is possible to replicate the intervention in the same context, as it was feasible to realize a 12-session intervention, with a complementary therapy (prenatal yoga), as well as cognitive behavioral strategies. It also represents an alternative to treat obesity in pregnancy and promote healthy eating and physical activity. The findings show this intervention is easy to apply and potentially useful to raise awareness in pregnant women about their own health. Furthermore, there is a less gestational weight gain that received psychoeducational intervention.
Including early education, a healthy diet and physical activity, and prenatal yoga, as well as strategies to control healthy eating barriers and physical activity in pregnancy can help women in a personal way to improve their ability to increase weight in the recommended parameters during this period.
REFERENCIAS
1. Goldstein RF, Abell SK, Ranasinha S, Misso ML, Boyle JA, Harrison CL, et al. Gestational weight gain across continents and ethnicity: systematic review and meta-analysis of maternal and infant outcomes in more than one million women. BMC Med. 2018;16(1):153. Disponible en: https://doi.org/10.1186/s12916-018-1128-1 [ Links ]
2. Barquera S, Hernández-Barrera L, Trejo B, Shamah T, Campos-Nonato I, Rivera-Dommarco J. Obesidad en México, prevalencia y tendencias en adultos. Ensanut 2018-19. Salud pública Méx. 2020; 62(6): 682-692. Disponible en: https://doi.org/10.21149/11630 [ Links ]
3. Fakhraei R, Denize K, Simon A, Sharif A, Zhu-Pawlowsky J, Dingwall-Harvey ALJ, et al. Predictors of Adverse Pregnancy Outcomes in Pregnant Women Living with Obesity: A Systematic Review. Int J Environ Res Public Health. 2022;19(4):2063. Disponible en: https://doi.org/10.3390/ijerph19042063 [ Links ]
4. Langley-Evans SC, Jo Pearce J, SE. Overweight, obesity and excessive weight gain in pregnancy as risk factors for adverse pregnancy outcomes: A narrative review. J Hum Nutr Diet. 2022;35(2):250-264. https://doi.org/10.1111/jhn.12999. [ Links ]
5. Zhou M, Peng X, Yi H, Tang S, You H. Determinants of excessive gestational weight gain: a systematic review and meta-analysis. Arch Public Health. 2022;80(1):129. https://doi.org/10.1186/s13690-022-00864-9. [ Links ]
6. Farias DR, Carrilho TRB, Freitas-Costa NC, Batalha MA, Gonzalez M, Kac G. Maternal mental health and gestational weight gain in a Brazilian Cohort. Sci Rep. 2021;11(1):10787. https://doi.org/10.1038/s41598-021-90179-6 [ Links ]
7. Zhou M, Peng X, Yi H, Tang S, You H. Determinants of excessive gestational weight gain: a systematic review and meta-analysis. Arch Public Health. 2022;80(1):129. https://doi.org/10.1186/s13690-022-00864-9 [ Links ]
8. Guzmán-Ortiz E, Cárdenas-Villarreal VM, Guevara-Valtier MC, Botello-Moreno Y. Estado nutricio saludable en la mujer durante la gestación: teoría de rango medio. Enfermería universitaria. 2018;15(3):305-16. Disponible en: https://doi.org/10.22201/eneo.23958421e.2018.3.67082 [ Links ]
9. Amyx M, Zeitlin J, Hermann M, Castetbon K, Blondel B, Le Ray C. Maternal characteristics associated with gestational weight gain in France: a population-based, nationally representative study. BMJ Open. 2021;11(7):e049497. Disponible en: https://doi.org/10.1136/bmjopen-2021-049497. [ Links ]
10. Cantor A, Jungbauer RM, McDonagh MS, Blazina I, Marshall NE, Weeks C, et al. Counseling and Behavioral Interventions for Healthy Weight and Weight Gain in Pregnancy: A Systematic Review for the U.S. Preventive Services Task Force. JAMA. 2021;325(20):2094-2109. https://doi.org/10.1001/jama.2021.4230. [ Links ]
11. Guzmán-Ortiz E, Flores-Peña Y, Felix-Ortiz RE, Cárdenas-Villarreal VM. Intervenciones psicoeducativas para reducir factores psicosociales y controlar el peso en mujeres embarazadas. Journal health NPEPS. 2018;3(1):253-67. Disponible en: http://dx.doi.org/10.30681/252610102807 [ Links ]
12. Ng QX, Venkatanarayanan N, Loke W, Yeo WS, Lim DY, Chan HW, et al. A meta-analysis of the effectiveness of yoga-based interventions for maternal depression during pregnancy. Complement Ther Clin Pract. 2019;34:8-12. Disponible en: https://doi.org/10.1016/j.ctcp.2018.10.016 [ Links ]
13. Murdaugh CL, Pender NJ, Parsons MA. Health promotion in nursing practice. Pearson. Boston, Massachusetts. Estados Unidos de América, 2019. [ Links ]
14. Vahedian Shahroodi M, Tavakoly Sany SB, Hosseini Khaboshan Z, Esmaeily H, Jafari A, Tajfard M. Effect of a theory-based educational intervention for enhancing nutrition and physical activity among Iranian women: a randomised control trial. Public Health Nutr. 2021;24(18):6046-6057. Disponible en: https://doi.org/10.1017/S1368980021002664. [ Links ]
15. Gitlin, Laura N., and Sara J. Czaja. Behavioral intervention research: Designing, evaluating, and implementing. Springer publishing company, 2015. [ Links ]
16. Sidani, Souraya, and Carrie Jo Braden. Design, evaluation, and translation of nursing interventions. John Wiley & Sons, 2011. [ Links ]
17. Sabooteh S, Feizi A, Shekarchizadeh P, Shahnazi H, Mostafavi F. Designing and evaluation of E-health educational intervention on students' physical activity: an application of Pender's health promotion model. BMC Public Health. 2021;21(1):657. Disponible en: https://doi.org/10.1186/s12889-021-10641-y [ Links ]
18. Institute of Medicine, National Research Council, Committee to Reexamine Institute of Medicine Pregnancy Weight Guidelines. Weight Gain During Pregnancy: Reexamining the Guidelines. Rasmussen KM, Yaktine AL, editors. Washington (DC): National Academies Press (US); 2009. PMID: 20669500. Disponible en: https://doi.org/10.17226/12584 [ Links ]
19. Vincent D, Pasvogel A, Barrera L. A feasibility study of a culturally tailored diabetes intervention for Mexican Americans. Biol Res Nurs. 2007;9(2):130-41. Disponible en: https://doi.org/10.1177/1099800407304980 [ Links ]
20. Xu MY, Guo YJ, Zhang LJ, Lu QB. Effect of individualized weight management intervention on excessive gestational weight gain and perinatal outcomes: a randomized controlled trial. PeerJ. 2022;10:e13067. Disponible en: https://doi.org/10.7717/peerj.13067 [ Links ]
21. Liu J, Wilcox S, Wingard E, Turner-McGrievy G, Hutto B, Burgis J. A Behavioral Lifestyle Intervention to Limit Gestational Weight Gain in Pregnant Women with Overweight and Obesity. Obesity (Silver Spring). 2021;29(4):672-680. Disponible: https://doi.org/10.1002/oby.23119 [ Links ]
22. Yew TW, Chi C, Chan SY, van Dam RM, Whitton C, Lim CS, et al. A Randomized Controlled Trial to Evaluate the Effects of a Smartphone Application-Based Lifestyle Coaching Program on Gestational Weight Gain, Glycemic Control, and Maternal and Neonatal Outcomes in Women With Gestational Diabetes Mellitus: The SMART-GDM Study. Diabetes Care. 2021;44(2):456-463. Disponible en: https://doi.org/10.2337/dc20-1216 [ Links ]
23. Sandborg J, Söderström E, Henriksson P, Bendtsen M, Henström M, Leppänen MH, et al. Effectiveness of a Smartphone App to Promote Healthy Weight Gain, Diet, and Physical Activity During Pregnancy (HealthyMoms): Randomized Controlled Trial. JMIR Mhealth Uhealth. 2021;9(3):e26091. Disponible en: https://doi.org/10.2196/26091 [ Links ]
24. Gesell SB, Katula JA, Strickland C, Vitolins MZ. Feasibility and Initial Efficacy Evaluation of a Community-Based Cognitive-Behavioral Lifestyle Intervention to Prevent Excessive Weight Gain During Pregnancy in Latina Women. Matern Child Health J. 2015;19(8):1842-52. Disponible es:https://doi.org/10.1007/s10995-015-1698-x [ Links ]
25. Bowen DJ, Kreuter M, Spring B, Cofta-Woerpel L, Linnan L, Weiner D, et al. How we design feasibility studies. Am J Prev Med. 2009;36(5):452-7. Disponible en: https://doi.org/10.1016/j.amepre.2009.02.002 [ Links ]
Received: February 27, 2023; Accepted: June 23, 2023











 texto em
texto em