Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versão On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.1 Jan./Fev. 2006
ORAL SURGERY
Osteonecrosis of the jaws and bisphosphonates. Report of three cases
Daniel Pastor Zuazaga 1, Joaquín Garatea Crelgo 2, Raúl Martino Gorbea 3,
Amaya Etayo Pérez 3, Cristina Sebastián López 1
(1) Oral and Maxillofacial Surgery Resident
(2) Oral and Maxillofacial Surgeon. Stomatologist
(3) Oral and Maxillofacial Surgeon. Servicio de Cirugía Oral y Maxilofacial. Hospital Virgen del Camino Pamplona (Navarra)
ABSTRACT
Bisphosphonates are recently acquiring increasing relevance in the treatment
of several diseases.
In line with the increased use of these compounds, cases of mandibular
osteonecrosis, and to a lesser extent, maxillary osteonecrosis, are being
reported. This necrosis is difficult to treat in patients who usually have a
previously limited quality of life.
A surgical performance carried out by oral and maxillofacial surgeons,
stomatologists and odontologists might lead to bone exposure.
A treatment based on conservation and as harmless as possible seems to be the
most advisable way of acting with these patients in order to minimize the
incidence and treat the complications, once the lesions have been ascertained.
We report three cases treated in our service of osteonecrosis of the jaws after
exodontics.
This side effect should be remembered before starting any surgical treatment in
these patients.
Key words: Bisphosphonates, osteonecrosis, side effects.
RESUMEN
Los bisfosfonatos están adquiriendo una relevancia terapéutica cada vez mayor,
dada su utilidad en el manejo de diversas patologías.
Con el incremento de su uso, se están documentando casos de necrosis ósea
mandibular, y en menor medida maxilar, de difícil solución y con una
importante afectación de la calidad de vida de los pacientes en tratamiento con
estos fármacos.
El factor que con mayor frecuencia desencadena el proceso es la actuación de
los profesionales: odontólogos, estomatólogos y cirujanos orales y
maxilofaciales.
La previsión, las intervenciones atraumáticas y el tratamiento conservador,
parecen ser los medios más adecuados para minimizar la incidencia o resolver
las complicaciones.
Este artículo presenta tres casos, seguidos por nuestro servicio, de pacientes
con necrosis ósea maxilar tras procedimientos dentales, fundamentalmente
exodoncias.
El conocimiento de este posible efecto secundario de los bisfosfonatos debería
ser tenido en cuenta antes de cualquier intervención en este tipo de pacientes.
Palabras clave: Bisfosfonatos, osteonecrosis, efectos secundarios.
Introduction
Bisphosphonates are recently acquiring increasing relevance with regard to the treatment of several pathologies such as lytic bone metastasis, malignant hypercalcemia, multiple myeloma, osteoporosis and Paget´s disease. (1)
These compounds are pyrophosphate analogues where a carbon atom has replaced the oxygen between the phosphates, changing the lateral chains. They show great affinity with hydroxyapatite crystals and inhibit bone resorption. (2)
The effectiveness and power of bisphosphonates are common knowledge. In general, they show high tolerance, rarely occurring side effects of clinical significance. This last feature is caused by the accumulation of bisphosphonates on bone tissue, where their average life is longer than the time they spend in circulation. These features make bisphosphonates an effective and secure drug.
In line with the increased use of these compounds, cases of mandibular osteonecrosis, and to a lesser extent, maxillary osteonecrosis, are being recorded. These cases are associated with treatments with certain kinds of bisphosphonates: the aminobisphosphonates pamidronate disodium (Aredia®) and zoledronic acid (Zometa®), specially in oncologic patients in advanced stage. R.E. Marxs, S.L. Ruggieros and J.V. Bagáns case reports are some of these studies. (3-6)
It is our intention to report a possible side effect produced by treatments with aminobisphosphonates, recently recorded in monographs, but of great clinical relevance due to the detriment in patients quality of life.
Case 1
67 year-old woman; smoker (6 cigarettes / day). She had been diagnosed as having breast cancer (T2 N0 M0) and treated with surgery combined with chemotherapy and radiotherapy. Due to the metastatic progression of the disease, the treatment with bisphosphonates was initiated (pamidronate 90 mg IV doses 20 monthly cycles). It is after the first 9 cycles of pamidronate that the patient is remitted to our practice by her oncologist, suffering from burning sensation and diffuse gingival pain, regular gingival hemorrhages, and showing a very painful lesion (5mm in diameter) in the lateral edge of her right hemitongue.
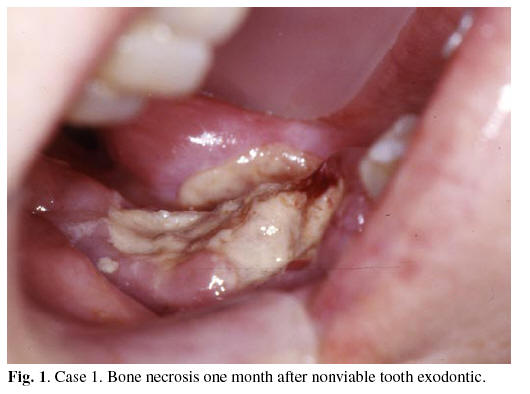
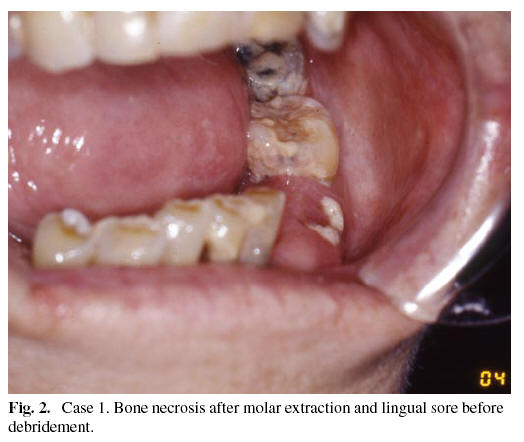
The extraction of the molar which produced the lingual sore and of other four teeth without viability was prescribed. Approximately one month after such exodontics, bone exposure occurred where the extractions had been performed. (Figure 1) Limited curettages of the bone necrosis were made complemented with antibiotic therapy (amoxicilline, clarythromycin) and chlorhexidine gel application. The evolution was favourable in every area, except in the mandibular molar one, where the bone exposure maintained the lingual sore, requiring a more aggressive debridement. Although the exposure didnt disappear completely, control of the patients pain was achieved with the resolution of the lingual lesion.(Figure 2)
Case 2
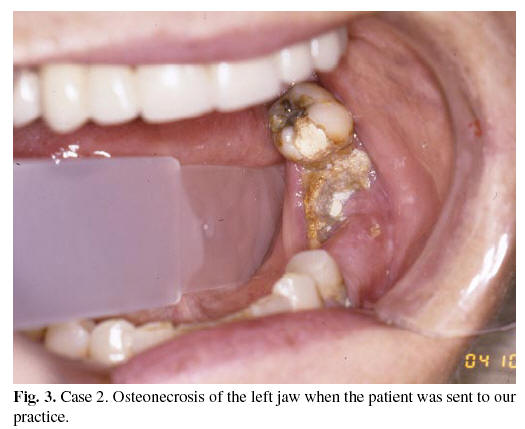
49 year old woman; smoker (30 cigarettes / day). She had been diagnosed as having breast cancer (T1 N0 M0) and treated with surgery, chemotherapy and radiotherapy. Given the metastatic evolution of the disease, she started treatment with zoledronate (4 mg IV doses monthly cycles). She was sent to our practice by her stomatologist, as she showed mandibular nonhealing sockets after dental extractions, periodontal pain and paresthesia of the inferior dental nerve, without metastatic finding. (Figure 3) She had been previously diagnosed and treated as having dental abscess. She had improved with antibiotic treatment, but the process had not been completely solved. Nonsurgical treatment was prescribed, amoxicilline and clorhexidine, and the lesion healed.
Case 3
71 year old man. He had been diagnosed as having multiple myeloma (III-A) and treated with chemotherapy, radiotherapy and medullar autotransplantation. He started treatment with bisphosphonates due to hypercalcemia (pamidronate 90 mg IV doses monthly for three years and zoledronate 4 mg IV doses monthly for one year). He was sent to our practice by his odontologist as he showed nonhealing sockets after mandibular exodontics. The axial computed tomography showed lytic lesions and the patologic studies bone necrosis and reactive osteitis. Surgical treatment was chosen, large debridement and a mucosal flap, complemented with antibiotic therapy and chlorhexidine rinses. Three weeks after surgery bone exposure was seen and conservative treatment precribed, clorhexidine gel, with favourable evolution.
Discussion
Pamidronate and zoledronate are synthetic analogues of endogenous pyrophosphate. Their clinical application involves a direct inhibition of the osteoclastic function.
Pamidronate disodium (Aredia®) and zoledronic acid (Zometa®) belong to the aminobisphosphonate group, nitrogen containing bisphosphonates with greater power and slower metabolization compared to those synthetized earlier. The use of these bisphosphonates is increasing in the treatment of several diseases such as hypercalcemia associated with multiple myeloma or metastatic cancer, osteoporosis and Pagets disease. (1,2)
Some of the mechanisms for antiresorptive action and the subsequent low fragility of bone tissue are:
-Direct antiapoptotic effect on osteoblasts regardeless of the proapoptotic common stimulation, in vitro and in vivo.
-Decreased osteoclast progenitor development and decreased mature osteoclasts recruitment in bone tissue.
-Promotion of apoptosis of mature osteoclasts blocking regulating proteins of mevalonate pathway. (7,8)
-Antiangiogenic properties reducing the circulating endothelial growth factor (EGF). (5)
Bisphosphonates have a direct effect on this dynamic unit which regulates the turn-over between bone formation and resorption, increasing osteoblasts proliferation and decreasing osteoclasts average life, activity and adherence to the mineralized matrix. These effects have been also seen in the maxillofacial area. (9-11)
Through such metabolic changes, aminobisphosphonates reduce bone resorption decreasing skeletal morbidity in oncological patients with bone metastasis. They relieve bone pain, stabilize or even improve lytic bone lesions, decrease the incidence of pathologic fractures, spinal cord compression, hypercalcemia and the need of palliative radiation therapy, noticeably improving patients quality of life. The median time to the first skeletal event is also lengthened and the development of new osteolytic lesions is prevented. As a long-term effect, they also decrease the need of subsequent orthopedic surgery although they dont lengthen survival. (12,13)
With the increasing use of pamidronate and zoledronate new cases of osteonecrosis are being reported, although sometimes there is no causal connection due to a lack of previous literature. (14) The three cases here described showed resistance to both medical and surgical treatments. They were oncological patients afflicted with metastatic breast cancer or multiple myeloma who had been treated with such drugs (Pamidronate 90 mg monthly IV, Zoledronate 4 mg monthly IV).
According to R.E. Marx, the incidence of avascular necrosis of the jaws induced by pamidronate and zoledronate is significant, especially in therapies involving corticosteroids. S.L. Ruggieros and J.V. Bagáns cases reports are some of the studies which support this side effect. There is evidence of exposed necrotic bone, more frequently at the mylohyoid ridge and at the crestal mandible. Radiographic images might present a normal structure without visible lesions, because the bone density remains, inespecific changes or lytic lesions. Risk seems to be increased by long term treatments (longer than a year), and particularly when synchronic tumors, hypoproteinemia, steroids, renal failure or simultaneous chemotherapy treatments occur. (3-5)
At the beginning, the reported cases were diagnosed as different dental procedures such as odontalgia, dental abscess, osteomyelitis, etc... and extraction of the painful dental pieces always resulted in a new bone exposure. This might involve the physician as a possible worsening factor of the process, making it even more complex. (6)
Mandibular-maxillary occurrence of this pathology in the cases treated in our department and the absence of lesions in the rest of the bone tissues supports R.E. Marxs hypothesis, which suggests decisive influence of dental structures. (4) The bone, externally exposed through dental attachments, requires an adequate metabolism and blood supply. The normal turn-over modified by inhibition of osteoclastic resorption and vascular insufficiency could exceed bone vital capacity, resulting in avascular bone necrosis (5). This osteonecrosis is difficult to treat, having no established guidelines for the time being. We have obtained successful results from the treatment of medium size lesions. However, complete resolution has not been achieved in the case of the largest one, where the treatment was merely palliative. Each new extraction, as well as debridements, can cause a greater exposure. Direct closure over bone tissue could fail and sometimes cause worsening, because it is difficult to be sure that the remaining bone is healthy. Surgery was reserved only for the areas which caused painful lesions on the tongue or soft tissue more aggressive alternatives and hyperbaric oxygen cannot be dismissed as a therapeutic option. (3-6,14)
From our own experience we agree with R.E. Marx that the antibiotic treatment (penicillin, erythromycin), together with limited debridements, is the best option to palliate, or even solve , this kind of lesions. (4,5) It is vital to maximize oral hygiene and the use of chlorhexidine containing gel and rinse, as well as the restriction of aggressive actions such as exodontics, unless they are unavoidable. If surgical treatment is required, R.E. Marx recommends a two months interruption of bisphosphonates. (3)
It is unquestionable that other well-known factors also contribute to the appearance of mandibular or maxillary osteonecrosis (radiation therapy, chemotherapy, corticoids, infections, anemia and vasoconstrictor local anesthetics). (15) From them all, radiation therapy remains the most influential, when it is used in the treatment of head and neck tumors. Our department has a population of reference of 560,000 and started giving assistance over 25 years ago; the incidence of malignant tumors in this population approaches the European average. The appearance of three similar cases, the only ones in our service which are not associated with head and neck radiation therapy and in less than six months, leads us to think of the appearance of a new factor.
Although a direct connection with the use of bisphosphonates in this pathology has not been established yet, the treatment with pamidronate and zoledronic acid, associated or not with other therapies, is common to all cases.
Until a further knowledge about the causes for this pathology is achieved, the best option seems to be a maximum control of the cases treated with pamidronate and zoledronate.
Conclusions
-Treatment with pamidronate and zoledronate might be a determining factor in oncological patients suffering from mandible and maxilla bone necrosis.
- A surgical performance carried out by oral and maxillofacial surgeons, stomatologists and odontologists might lead to bone exposure.
-It is a pathology difficult to treat, in patients who usually have a previously limited quality of life.
-A treatment based on conservation and as harmless as possible seems to be the most advisable way of acting with these patients.
-Further research will be essential to clarify the cause, minimize the incidence and register the treatment, once the lesions have been ascertained.
![]() Correspondence
Correspondence
Dr. Daniel Pastor Zuazaga
Servicio de Cirugía Oral y Maxilofacial
Hospital Virgen del Camino Pamplona (Navarra)
C/ Irunlarrea 4
C.P.: 31008
Teléfono: 848 429400 - Fax: 848 429924
E-mail: dapazu@hotmail.com
E-mail: jgaratec@cfnavarra.es
Received: 25-03-2005
Accepted: 11-05-2005
References
1. Hillner BE, Ingle JN, Berenson JR, Janjan NA, Albain KS, Lipton A, et al. American Society of Clinical Oncology Guideline on the role of bisphosphonates in breast cancer. J Clin Oncol 2000;18:1378-91. [ Links ]
2. Plotkin LI, Weinstein RS, Parfitt AM,Roberson PK, Manolagas SC, Bellido T. Prevention of osteocyte and osteoblast apoptosis by bisphosphonates and calcitonin . J Clin Invest 1999;104:1373-4. [ Links ]
3. Marx RE, Stern D, eds. Oral and Maxillofacial Pathology. A rationale for diagnosis and treatment. Quintessence Publishing Co.Illinois; 2003. p. 36-8. [ Links ]
4. Marx RE. Pamidronate (Aredia) and Zoledronate (Zometa) induced avascular necrosis of the jaws: A growing epidemic. J Oral Maxillofac Surg 2003;61:1115-7. [ Links ]
5. Ruggiero SL, Mehrotra B, Rosenberg TJ, Engroff SL. Osteonecrosis of the jaws associated with the use of bisphosphonates: a review of 63 cases. J Oral Maxillofac Surg 2004; 62:527-34. [ Links ]
6. Bagan JV, Murillo J, Jiménez Y, Poveda R, Milian MA, Sanchis JM et al. Avascular jaw osteonecrosis in association with cancer chemotherapy: series of 10 cases. J Oral Pathol Med 2005;34:120-3. [ Links ]
7. Ross JR, Saunders Y, Edmonds PM, Patel S, Broadley KE, Johnston RD. Sistematic review of role of bisphosphonates on skeletal morbidity in metastatic cancer. Br Med J 2003; 327-469. [ Links ]
8. Oades GM, Senaratne SG, Clarke IA, Kirby RS, Colston KW. Nitrogen containing bisphosphonates induce apoptosis and inhibit the mevalonate pathway, impairing ras membrane localization in prostate cancer cells. J Urol 2003;170:246-52. [ Links ]
9. Fleisch H: Bisphosphonates. Mechanisms of action. Endocrine Reviews 1998;19:80-100. [ Links ]
10. Reinholz GG, Getz B, Pederson L, Sanders ES, Subramaniam M, Ingle JN et al. Bisphosphonates directly regulate cell proliferation, differentiation and gene expression in human osteoblasts. Cancer Res 2000;60:6001-7. [ Links ]
11. Altundal H, Guvener O. The effect of alendronate on resorption of the alveolar bone following tooth extraction. Int J Oral Maxillofac Surg 2004;33:286-93. [ Links ]
12. Hortobagyi GN, Theriault RL, Porter L, Blainey D, Lipton A, Sinoff C, et al. Efficacy of Pamidronate in reducing skeletal complications in patients with breast cancer and lytic bone metastases. N Engl J Med 1996;335:1785-92. [ Links ]
13. Gralow JR. Bisphosphonates as adjuvant treatment for breast cancer. Br Med J 2002;325:1051-2. [ Links ]
14. Wang J, Goodger NM, Pogrel MA. Osteonecrosis of the jaws associated with cancer chemotherapy. J Oral Maxillofac Surg 2003;61:1104-7. [ Links ]
15. Tarasoff P, Csermak K. Avascular necrosis of the jaws: risk factors in metastatic cancer patients. J Oral Maxillofac Surg 2003;61:1238-9. [ Links ]











 texto em
texto em