Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Medicina Oral, Patología Oral y Cirugía Bucal (Internet)
versão On-line ISSN 1698-6946
Med. oral patol. oral cir.bucal (Internet) vol.11 no.4 Jul. 2006
Multiple oral fibropapillomatosis as an initial manifestation of Cowden Syndrome. Case report
Fibropapilomatosis oral múltiple como manifestación inicial de Síndrome de Cowden. Caso clínico
Luis Miguel Capitán Cañadas1, José Luis Salinas
Sánchez2, Sergio Luis Martínez Castillo2,
Ildefonso
Leopoldo Labrot Moleón1, David Durán Moreno1, Darío
Sánchez López2, Eduardo Valencia Laseca3
1Internal Medicine Resident
2Adjunct Doctor
3Service Director. Maxillofacial and Oral Surgery Service.
Virgen de las Nieves University Hospital, Granada
ABSTRACT
Cowden syndrome is a rare hereditary disease included within
hamartoma-type gastrointestinal polyposis. It is characterised by associated
mucocutaneous anomalies and by the extraordinary tendency to develop malignant
neoplasia, mainly in the breast and thyroid. Early diagnosis of the syndrome and
adequate tumoral screening in patients with mucocutaneous papillomatosis make it
possible to make an earlier diagnosis of associated pathologies which have great
morbidity when detected late. We present the case of a patient diagnosed with
Cowden syndrome after consultation for labial papillomatous lesions of long
evolution who was subsequently treated for breast and kidney cancer in initial
stages.
The correct diagnosis of a banal pathology of oral mucosa
made it possible for us to take early action against the neoplastic pathology
associated with this disease.
Key words: Cowden syndrome, multiple hamartomas, oral, papilloma.
RESUMEN
El síndrome de Cowden es una infrecuente enfermedad
hereditaria englobada dentro de las poliposis gastrointestinales de tipo
hamartomatoso. Se caracteriza por asociar anomalías cutaneomucosas y por la
extraordinaria tendencia a desarrollar neoplasias malignas, principalmente de
mama y tiroides. La importancia de un diagnóstico precoz del síndrome y de un
adecuado screening tumoral en pacientes con lesiones papilomatosas
cutaneomucosas, nos va a permitir adelantarnos en el diagnóstico de patologías
con enorme morbimortalidad asociada en caso de una detección tardía. Presentamos
el caso de una paciente diagnosticada de síndrome de Cowden tras consultar por
lesiones papilomatosas labiales de largo tiempo de evolución y tratada
posteriormente de cáncer de mama y riñón en estadios iniciales.
El correcto diagnóstico de una patología banal de mucosa
oral, nos ha permitido actuar de manera muy precoz frente a la patología
neoplásica asociada a dicha enfermedad.
Palabras clave: Síndrome de Cowden, hamartomas múltiples, oral, papiloma.
Introduction
First described by Lloyd and Dennis in 1963 (1), Cowden syndrome or multiple hamartoma syndrome is a rare hereditary genodermatosis of dominant autosomic transmission with variable expressiveness (2), included within the large family of hereditary gastrointestinal polyposis (3). These polyposis are characterised by the type of dominant polyp: hamartomatous or adenomatous, the former defined by an overgrowth of epithelial and stromal cellular elements of normotypical features (2). Hamartomatous polyposis represent a small but not insignificant number of hereditary polyposis with a predisposition to degenerate into gastrointestinal cancer (4).
The prevalence of Cowden syndrome is 1:200,000 (3) making it what is considered to be a rare disease (CIE-9-MC:759.6 code) (5). Cowden syndrome shows multiple hamartomas of endodermic, ectodermic or mesodermic origin (3). Despite being treated as a disease within the gastrointestinal area, its extraintestinal clinical manifestations are manifest and on numerous occasions determine the patients prognosis (3).
- Gastrointestinal manifestations
Manifestations of Cowden syndrome in the gastrointestinal tract are practically indistinguishable from family juvenile polyposis syndrome (6). They are characterised by the presence of multiple hamartomatous polyps along the gastrointestinal tract, principally located in the colon and rectum (4, 7), generally asymptomatic (8), a fact that contributes to the underdiagnosis of the disease (4). Histologically they are characterised by presenting a high number of normotypical glands of mucoid content, inflammation and edema of the lamina propria and lymphoplasmocitary infiltration (9). We may also find ganglioneuromas and lipomatous and inflammatory polyps and ganglioneuromas (3). In the esophagus it is possible to find glycogenic acanthosis without associated clinical repercussions (10).
- Extraintestinal manifestacions
Unlike with other polyposis, systemic manifestations of Cowden syndrome are abundant and sufficiently distinctive, which can determine their clinical diagnosis (3). Mucocutaneous lesions are the most notable manifestations of Cowden syndrome; in fact approximately 80% of patients diagnosed with the syndrome of multiple hamartomas has or will develop some manifestation of this type in the future (11).
These are usually lesions that evolve over a long period of time and which, generally speaking, manifest themselves in the initial stages, before the other neoplastic processes associated with the disease develop, which shows the importance of detecting these benign lesions early and beginning adequate tumoral screening for early diagnosis (12). The most notable types of these lesions are facial trichilemmomas, acral keratosis, subcutaneous lipomas, palmoplantar keratosis, oral and labial papillomas with a characteristic cobbled look (13). The appearance of vitiligo, neuromas, xanthomas and café-au-lait spots is less commonly associated with Cowden syndrome (14).
Although these are the most noted clinical manifestations, these lesions can be accompanied by otorhinolaryngological (15), ophthalmological (16), gynecological (17), renal (18) and craniomaxillofacial (3) manifestations. Because of its special importance, it is imperative to underscore the high risk associated with developing neoplastic pathologies, mainly of the breast and thyroid (3), without overlooking the possibility of developing other types of neoplasia (ovarian, uterus, kidney and meninx) (17).
Diagnosis
Diagnosis is mainly based on clinical criteria. At this time the diagnostic method of major and minor clinical criteria proposed by Salem and Steck (11) as subsequently revised and modified by the International Cowden Consortium in 2000 (19) is the accepted one (Table 1. Pathognomonic Lesions and Major and Minor Criteria). Cowden syndrome is diagnosed when the patient shows one of the following criteria:
1. Presence of pathognomonic lesions, always when under one of the following conditions:
- Six or more facial papules, of which three or more must be trichilemmomas.
- Facial papules and papillomatosis in oral mucosa.
- Papillomatosis in oral mucous and acral keratosis.
- Six or more palmoplantar keratosis lesions2. Presence of two major criteria, one of which must be macrocephalia or Lhermitte-Duclos disease
3. Presence of one major criterion and three minor criteria
4. Presence of four minor criteria
Cowden syndrome can be diagnosed for a direct relative of an affected patient if he or she meets one of the following conditions (3):
1. Mucocutaneous pathognomonic lesions
2. Any major criterion with or without associated minor criteria.
3. Presence of two minor criteria.
Clinical case
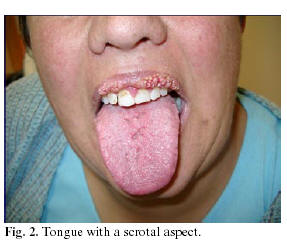
Female patient, 42 years old, with no personal antecedents of interest, referred by her general practitioner to the Maxillofacial and Oral Surgery office of the Virgen de las Nieves University Hospital in Granada, Spain, with multiple lesions of a papillomatous aspect on her upper lip (Figures 1a and 1b), approximately fifteen years in evolution, according to the patient. The intraoral examination of the patient showed the presence of a tongue with a scrotal aspect (Figure 2). Under local anaesthesia and in two surgical visits, a complete exeresis of the lesions was undertaken. The anatomopathological study of the lesions typified them as fibropapillomas.
Because of the cobbled characteristic of the mucous lesions, joined with the systemic examination of cutaneous trichilemmomas in acral regions (Figure 3), the long evolution of the lesions and the presence of direct family antecedents (mother died of thyroid neoplasia at 49 years of age with the presence of the same type of lesions in the labial mucosa, sister with breast pathology of unknown origin and daughter operated on for a thyroid papillary carcinoma), the decision was made to send the patient to the Gynecological Service to screen for breast neoplastic pathology, given the strong suspicion, between the different diagnoses proposed, that we were looking at Cowden syndrome.
At the Gynecological Service in our hospital, the patient was diagnosed with bilateral breast fibrocystic pathology and infiltrating ductal carcinoma (GII) of the left breast, which required a tumorectomy and a homolateral axillary dissection and complementary treatment with post-operative chemoradiotherapy. Given the clinical diagnosis of genodermatosis of multiple hamartomas (the patient had a pathognomonic lesion, one major criterion and three minor criteria), a complete process of systemic tumoral screening was undertaken. The patient was evaluated at the Digestive Service, where the presence of asymptomatic polyps in the rectal and colon mucosa was detected in the clinical monitoring. She was subsequently sent to the Endocrinological Service to evaluate the progressive size of her thyroids associated with clinical hyperthyroidism. After discarding malignancy in a cytohistological study, the patient was operated on by the Endocrine Surgery Service, which performed a total thyroidectomy The conclusive anatomopathological result diagnosed the lesion as a multinodular colloid goitre.
Five months after the thyroid surgery and after a routine abdominopelvic ultrasound, a mass was detected on the right kidney, which after a CT scan, showed radiological characteristics of malignancy.
At the Urology Service, it was decided to perform a radical right nephrectomy plus a lymphadenectomy on the superior vena cava. The histological study of the surgical specimen led to the diagnosis of the lesion as renal carcinoma with clear and granular cells of a fundamentally tubular component. Post-surgical complementary treatment was not necessary.
Currently, the patient shows a progressive decrease in visual acuity of unknown origin in a study by the Ophthalmology Service.
All the neoplastic processes that were diagnosed and treated were detected in initial stages. At this time, the patient is in total remission from all the diagnosed and treated tumoral pathologies. Despite having a clear clinical diagnosis almost from the beginning, the patient has been studied at the National Centre for Oncological Research (Department of Human Genetics), which has confirmed definitively that she carries the c1093lnaGGAT mutation on the PTEN gene, which ratifies the genetic diagnosis of Cowden syndrome. The study was extended to the rest of her first-degree family members in order to carry out adequate screening and begin close clinical monitoring when necessary.
Discussion
Multiple hamartoma syndrome or Cowden syndrome appears mainly in Caucasians (95%) and affects women more than men (60%) (12). The symptoms usually appear between the third and fourth decade of life (6). The majority of new patients diagnosed appear as isolated cases without any history of family incidence (3). Carlson et al (9) determined that only 10-15% of the patients have a family member also affected. Possibly due to underdiagnosis of the disease, the true proportion of sporadic cases to related cases has not been determined (20). Approximately 80% of the patients carry the mutation in the tumour-suppressing gene PTEN [phosphatase and tensin homolog] located in chromosome 10q23.3 (21). This gene inhibits tumoral growth, acting as a regulator of the cellular growth activated by tyrosine kinase (10). Up to now, no other genetic mutations associated with the syndrome have been identified (3). Extraintestinal mucocutaneous manifestations constitute the most important clinical characteristic of this syndrome (3). In fact, the four pathognomonic criteria are found related to lesions of this type (19). On numerous occasions, as in the case presented here, it is this type of lesion that clues the specialist in to the existence of much more complex clinical symptoms (3). Slightly over 80% of patients diagnosed with Cowden syndrome have dermatological manifestations (11). Cutaneous lesions appear as papillomatous or lichenoid papules distributed mainly across the maxillofacial territory, neck, back of the hands and forearms (22). In the maxillofacial territory, they are concentrated around the mouth, ears, periorbita and glabellar zone (23). Histopathologically these lesions, identified as trichilemmomas, are hamartomatous in nature, derive from pilose follicles and constitute one of the most important systematic manifestations of the disease (24, 25). Acral keratosis is the second most common dermatological manifestation (3), with the presence of papules that are smooth or rough on the back of the hands and feet. Other less common cutaneous manifestations have been described such as vitiligo, café-au-lait spots and melanosis (14).
It is possible to find papular fibromatosis lesions in oral mucosa. Although the most frequent locations are the lips, tongue, gum, alveolar rim and jugal mucous membrane (26), other affected regions such as the palate, uvula, oropharynx, larynx and nasal mucosa have been described (22).
In patients with mucous membrane-supported prosthesis, it is possible to see the irritative lesion component (27). Under the microscope, they are lesions that are unspecific, with stratified squamous epithelial tissues and numerous fibrous bands (14). It is important to make a correct differential diagnosis of the fibropapillomatosis lesions of oral mucosa, which can be useful in handling the patient (Table 2. Differential Diagnosis of Oral Fibropapillomatosis Lesions). It is possible to observe the presence of scrotal tongue (23), ogival palate (3) and a tendency to contract periodontal disease (28) associated with the syndrome.
The benign cutaneous and mucous lesions described usually manifest themselves early, prior to the development of clinical manifestations of greater severity associated with Cowden syndrome (3), for which reason early recognition of this type of lesion is crucial for the diagnosis of the disease and the beginning of adequate tumoral screening (16).
The main extraintestinal manifestations associated with the syndrome of multiple hamartomas include the possibility of developing thyroid and breast pathology, mainly of a tumoral type (3). Around 67% of patients diagnosed with Cowden syndrome show thyroid pathology, which is the most common systemic manifestation associated with the syndrome (29). The main thyroid symptoms described are colloid goitres, follicular adenoma, papillary and follicular carcinoma, oncocytoma and thyroglossal duct cysts (3). The patient may present hypo-, hyper- or euthyroidism, without a clear tendency to any one of these clinical forms (29). Up to 3% of patients may develop thyroiditis and up to 12% carcinoma of the thyroid (30).
Slightly more than 50% of the patients affected by Cowden develop mammary pathology (16). The associated benign mammary pathology can include forms such as fibrocystic mastopathy, fibroadenomas and areolar malformations (3). The malignant forms include breast cancer (31), which is possibly the most worrisome manifestation of Cowden syndrome and can affect up to 36% of the patients (11), which means that close monitoring of the patient, period clinical examinations, mammograms and appropriate family screening are imperative.
Gynecological symptoms may include irregular menstruation, ovarian cysts and ovarian, cervical, endometrial and renal tumoral pathology (17).
Despite the fact that this is a disease that is originally digestive and contrary to what occurs with other hamartomatous polypomatosis, an increased risk of developing intestinal neoplasia is not documented (9, 16). However, and until we have more information in this respect, it is necessary to adequately screen for gastrointestinal tumours.
In approximately one third of patients with Cowden syndrome, skeletal alterations can occur, including craniomegaly, pectus excavatum, vertebral anomalies and ogival palate (32). Finally, there is a series of syndromes that can develop in the context of Cowden syndrome, such as ocular alterations like hypertelorism, corneal opacity and glaucoma (16), anomalies in the nervous system which can include neuromas of cutaneous nerve endings, neurofibromas, Lhermitte-Duclos disease and a progressive loss of hearing (15), cardiorespiratory pathologies including arterial hypertension, interauricular septal defects, mitral valve prolapse, insufficiency of the aortic and mitral valve and pulmonary hamartomas. (16). Another miscellany of tumours described (17, 18) in the context of Cowden syndrome include lipomas, liposarcomas, meninx tumours, non-Hodgkin lymphomas and Merkel cells carcinoma.
Conclusion
Beginning from the differential diagnosis of non-specific oral lesions of long-term evolution, clinical symptoms that also associated thyroid goitre and malignant neoplasia of the breast and kidney were also diagnosed.
Cowden syndrome is an infrequent cause of skin and oral mucosa fibropapillomatosis lesions. The development of these lesions usually precedes the almost systematic establishment of tumoral pathology, mainly in the breast and thyroid. Adequate early diagnosis of these lesions facilitates the monitoring, diagnosis and treatment of the patients in the initial stages, as well as prescribing systematic family screening.
![]() Correspondence:
Correspondence:
Dr. Luis Miguel Capitán Cañadas
Servicio de Cirugía Oral y Maxilofacial
Hospital Universitario Virgen de las Nieves. CRT.
Carretera de Jaén s/n. Granada. España.
E-mail: luismxf@hotmail.com
Received: 29-12-2005
Accepted: 29-03-2006
References
1. Lloyd K, Dennis M. Cowdens disease: a possible new symptom complex with multiple system involvement. Ann Int Med 1963;58:136-42. [ Links ]
2. Boardman LA. Hereditable colon cancer syndromes: Recognition and preventive management. Gastroenterol Clin N Am 2002;31:1107-31. [ Links ]
3. Schreibman IR, Baker M, Amos C, McGarrity TJ. The hamartomatous polyposis syndromes: A clinical and molecular review. Am J Gastroenterol 2005;100:476-90. [ Links ]
4. Longy M, Lacombe D. Cowdens disease: report of a family and review. Ann Genet 1996;39:35-42. [ Links ]
5. Ramírez Díaz-Bernardo, J. Introducción. En: Izquierdo Martínez M, Avellaneda Fernández A, eds. Enfermedades raras, un enfoque práctico. Madrid: Instituto de Salud Carlos III, Instituto de Investigación de Enfermedades Raras; 2004. p. 13-5. [ Links ]
6. Burt RW. Polyposis syndromes. Clin Perspectives Gastroenterol 2002:51-9. [ Links ]
7. Starink, Van der Venn JP, Arwert F, de Waal LP, de Lange GG, Gille JJ, et al. The Cowden syndrome: a clinical and genetic study in 21 patients. Clin Genet 1986;29:222-33. [ Links ]
8. Marra G, Armelao F, Vecchio FM, Percesepe A, Anti M. Cowdens disease with extensive gastrointestinal polyposis. J Clin Gastroenterol 1994;18:42-7. [ Links ]
9. Carlson GJ, Nivatvongs S, Snover Dc. Colorectal polyps in Cowdens disease (multiple hamartoma syndrome). Am J Surg Path 1984;8:763-70. [ Links ]
10. Mc Garrity TJ, Wagner Baker MJ, Ruggiero FM, Thiboutot DM, Hampel H, Zhou XP, et al. GI polyposis and glycogenic acanthosis of the esophagus associated with PTEN mutation positive Cowden syndrome in the absence of cutaneous manifestations. Am J Gastroenterol 2003; 98:1429-34. [ Links ]
11. Salem OS, Steck WD. Cowdens disease (multiple hamartoma and neoplasia syndrome): a case report and review of the English literature. J Am Acad Dermatol 1983; 8:686-96. [ Links ]
12. Botma M, Russel DI, Kell RA. Cowdens disease: a rare cause of oral papilomatosis. J Laringol Otol 2002; 116:221-3. [ Links ]
13. Hand JL, Rogers, RS. Oral manifestations of genodermatoses. Dermatol Clin 2003;21:183-94. [ Links ]
14. Thyresson HN, Doyle JA. Cowdens disease (multiple hamartoma syndrome) Mayo Clin Proc 1981;56:179-84. [ Links ]
15. Malone JP, Levin RJ, Fedok FG. Otolaryngologic manifestations of Cowden syndrome. Otolaryngol Head Neck Surg 2000;123:644-6. [ Links ]
16. Starink TM. Cowdens disease; analysis of fourteen new cases. J Am Acad Dermatol 1984;11:1127-41. [ Links ]
17. Lee HR, Moon YS, Yeom CH, Kim KW, Churi JY, Kim HK, et al. Cowdens disease. J Korean Med Surg 1997;12:570-5. [ Links ]
18. Attard TM, Lynch HT. Diagnosis and management issues in pediatric patients with gastrointestinal polyps. Pract Gastroenterol April 2003:57-72. [ Links ] 19. Eng C. Will the real Cowden syndrome please stand up: revised diagnostic criteria. J Med Genet 2000;37:828-30. [ Links ] 20. Schrager CA, Schneider D, Gruener AC, Tsou HC, Peacocke M. Clinical and pathological features of breast disease in Cowdens syndrome: An underrecognized syndrome with an increased risk of breast cancer. Hum Pathol 1998;29:47-53. [ Links ] 21. Marsh DJ, Coulon V, Lunetta KL, Roca-Serra P, Dahia PL, Zheng Z, et al. Mutation spectrum and genotype-phenotype analyses in Cowden disease and Bannayan-Zonana syndrome, two hamartoma syndromes with germline PTEN mutation. Hum Mol Genet 1998;7:507-15. [ Links ] 22. Hildenbrand C, Burgdorf WH, Lautenschlager. Cowden syndrome-Diagnostic skin signs. Dermatology 2001; 202:362-6. [ Links ] 23. Weary PE, Gorlin RJ, Gentry WC, Corner JE, Greer KE. Multiple hamartoma syndrome (Cowden disease). Arch Dermatol 1972;106:682-90. [ Links ] 24. Gorlin RJ, Cohen MM, Levin LS. Hamartoneoplastic syndromes: Cowden´s syndrome (multiple hamartoma syndrome). En: Syndromes of the Head and Neck. New York: Oxford University Press ed; 1990. p. 357-61. [ Links ] 25. Blanco V, Keochgerián V. Cowdens syndrome. Case report, with reference to an affected family. Med Oral Patol Oral Cir Bucal 2006;11:12-6. [ Links ] 26. Almenar R, Bagán JV, Milián MA, Jiménez Y. Síndrome de Cowden: presentación de un caso clínico con lesiones orales. An Med Int 2001;18:426-8. [ Links ] 27. Morrison JP, Kevin NC. Multiple endocrine neoplasia type IIB (mucosal neuroma syndrome, Wagenmann-Frobose syndrome). J Med Genet 1996;33:779-82. [ Links ] 28. Greer RO, Popper HA, de Mento FJ. Cowden´s disease (multiple hamartoma syndrome): report of a limited mucocutaneous form. J Periodontol 1976;47:531-4. [ Links ] 29. Hemmings CT. Thyroid pathology in four patients with Cowdens disease. Pathology 2003;35:311-4. [ Links ] 30. Eng C. Cowden syndrome. J Genet Counsel 1997;6:181. [ Links ] 31. Baù MG, Arisio R, Cristini G, Bertone E, Campogrande M. Screnning-detected breast carcinoma in a patient with Cowden síndrome. The breast 2004;13:239-41. [ Links ] 32. Saccardi A, Bacci S, Romagnoli P, Ravina A, Ficarra G. Cowden´s syndrome: a case report with clinical histopathological and immunological studies. Minerva Stomatol 1994;43:423-8. [ Links ]











 texto em
texto em