Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista de Osteoporosis y Metabolismo Mineral
versão On-line ISSN 2173-2345versão impressa ISSN 1889-836X
Rev Osteoporos Metab Miner vol.12 no.4 Madrid Out./Dez. 2020 Epub 05-Abr-2021
https://dx.doi.org/10.4321/s1889-836x2020000400008
SPECIAL ARTICLE
Connexin 43 and cellular senescence: new therapeutic strategies for treating osteoarthritis
1CellCOM Research Group. Biomedical Research Institute of A Coruña. A Coruña (Spain)
2European Research Institute for the Biology of Aging (ERIBA). University Medical Center Groningen (UMCG). University of Groningen (RUG). Groningen (Holland)
3Department of Orthopedic Surgery and Traumatology. University Hospital Complex of Santiago de Compostela. University of Santiago de Compostela (USC). Santiago de Compostela (Spain)
Osteoarthritis (OA) is one of the most prevalent rheumatic diseases at present. It is characterized by the progressive degeneration of articular cartilage accompanied by alterations in other tissues, such as in the subchondral bone, synovial tissue or muscle. Currently one of the most frequent causes of disability in the aging population worldwide, OA is one of the main causes of chronic pain. From the biomechanical point of view, the joint is involved in maintaining mechanical support by stabilizing movement and flexion. The mechanical consequences of joint degeneration include the loss of stability or increased load stress on the joints, associated with changes in the structure and composition of the articular cartilage. Given that the molecular mechanisms by which joint tissue degradation and the loss of its homeostasis occur are not yet known, the current treatments available are based on the use of anti-inflammatories and pain relief drugs.
Articular cartilage is a tissue with unique mechanical properties formed by a dense extracellular matrix (ECM) that covers the surface of the bone in mobile joints, mainly composed of different types of collagen, proteoglycans and glycoproteins. Chondrocytes, the only cell type described in articular cartilage, are the cells responsible for synthesizing ECM components, as well as maintaining tissue homeostasis. Taking into account the distribution of chondrocytes within cartilage, until a few years ago it was believed that chondrocytes were found in isolation in gaps inserted in the ECM without any type of cellular interaction or communication between them. However, recent results have shown that chondrocytes present cytoplasmic projections that are capable of crossing the ECM and connecting distant cells1. In line with these results, it has been shown that chondrocytes express several proteins of the connexin family, involved in cellular communication through gap junctions (GJs). In the case of cartilage, chondrocytes are capable of communicating through connexin channels formed mainly by connexin 43 (Cx43)2. Furthermore, through these cytoplasmic projections and gap junctions, chondrocytes are capable of exchanging different metabolites and small molecules such as ATP or RNA in addition to amino acids and proteins1,3. On the other hand, several studies indicate that the overactivity of Cx43 triggers an inflammatory and degenerative process related to joint degradation in patients with OA2. In our research group we have shown that alterations in Cx43 activity trigger changes in the phenotype of chondrocytes accompanied by an increase in the expression levels of interleukin-1β (IL-1β), cyclooxygenase2 (COX-2) and metalloprotease-3 (MMP-3)4 associated with the progress of the disease. The overexpression of Cx43 in a chondrocyte line increases the CD105 and CD166 markers associated with de-differentiated stem cells, as well as the translocation to the nucleus of the Twist-1 transcription factor, which indicates that they could be undergoing a process of epithelium-mesenchyme transition (TEM)4. Lastly, Cx43 overactivity is associated with increased levels of senescence markers such as p53, p16 and ß-galactosidase, as well as activation of NF-κβ accompanied by a senescent phenotype and increased secretion of inflammatory cytokines, known as the secretory senescence-associated phenotype (SASP)4. These results show that alterations in the expression and activity of Cx43 could be playing an essential role in the development and progression of the disease by modulating the phenotype of the adult chondrocyte. In fact, the decrease in Cx43 activity using different compounds improves the regeneration capacity of different tissues and in different models of age-associated diseases5,6, reinforcing the role of this transmembrane protein in tissue degeneration and senescence.
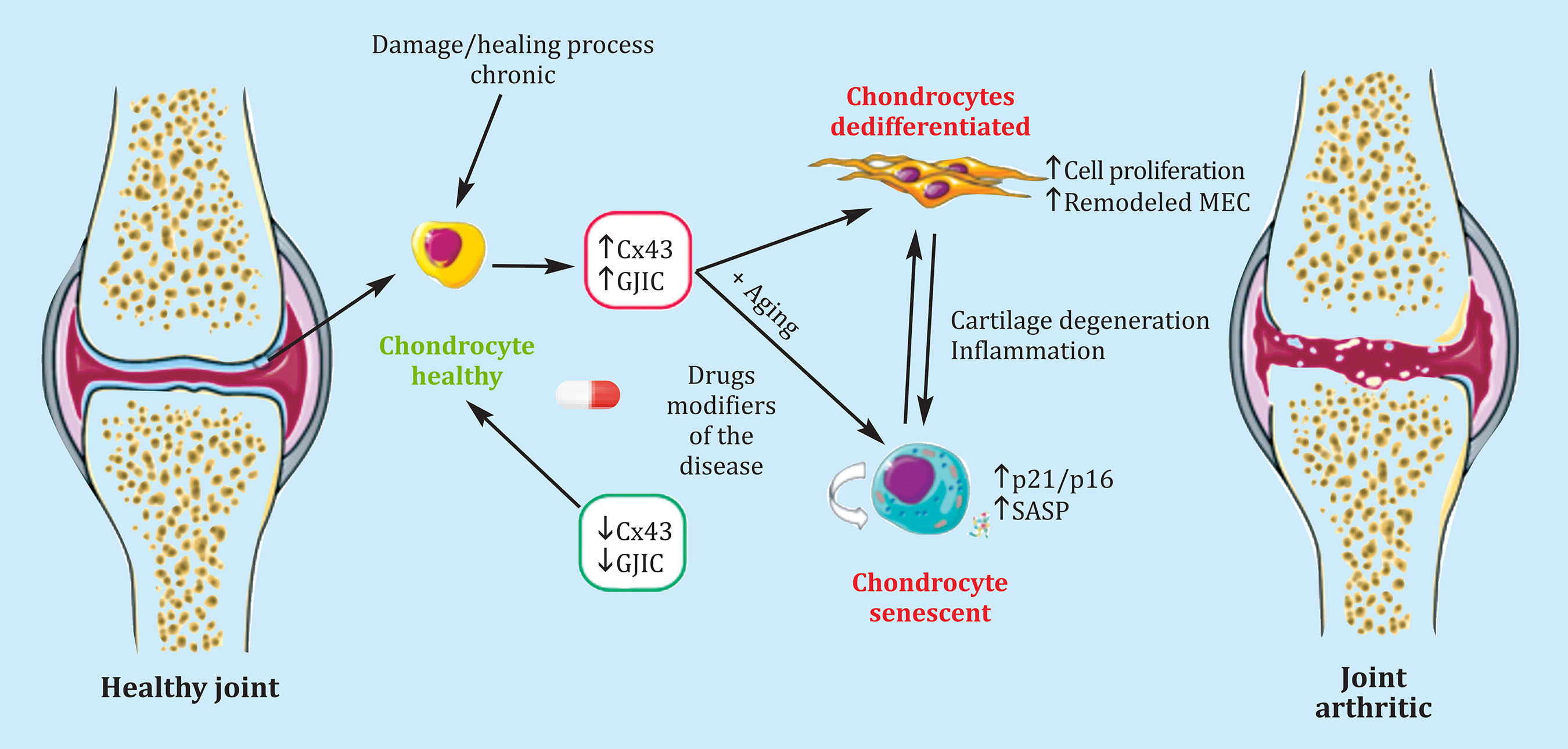
Figure 1. Cx43 is involved in the processes of de-differentiation and senescence in chondrocytes associated with in flammatory and degenerative processes in patients with OA. Decreasing Cx43 levels with osteoarthritis modifying drugs (DMARDs) could reverse this process and favor a regenerative environment that would prevent the progression of the disease
More studies are undoubtedly needed in this regard, but with our results, we could conclude that Cx43 is a therapeutic target of interest to maintain the adult chondrocyte phenotype, and avoid processes of de-differentiation and cellular senescence associated with an inflammatory and degenerative phenotype when it is maintained over time (chronically). In fact, in vitro models have already demonstrated its usefulness in reducing cell senescence markers and favoring chondrocyte re-differentiation, restoring tissue regeneration capacity7-9. In older adults, it should be noted that recently obtained results by our research group indicate that the increase in Cx43 could also be involved in tissue degeneration and accumulation of senescent cells in cases of intervertebral disc degeneration, suggesting that therapies aimed at modifying Cx43 They could be useful in the treatment of degenerative conditions in the intervertebral disc.
In recent years, different OA modifying drugs have been proposed as new therapeutic strategies because of their ability to promote chondrogenesis, thus promoting re-differentiation of chondrocytes and improving tissue regeneration. On the other hand, molecules capable of reducing Cx43 levels, such as oleuropein10, improve ECM formation in 3D models by increasing levels of type II collagen and proteoglycans, and also improve the arthritic chondrocyte phenotype by reducing gene expression levels inflammatory interleukins and metalloproteases10,11.
These and other studies show that high levels of Cx43 in cartilage observed from the first stages of the disease could be related to the activation of degradation processes of articular cartilage by activating the epithelium-mesenchyme transition (cell de-differentiation) and increasing cell senescence synergistically (Figure 1). Undoubtedly, the use of molecules and compounds that decrease the levels or activity of this protein will be of interest for developing new therapeutic strategies for the treatment of degenerative musculoskeletal diseases associated with age, such as osteoarthritis.
Acknowledgments: Our figures have been created using the material available at "Servier Medical Art" (smart.servier.com), and Creative Commons Attribution 3.0. Unported License.
REFERENCES
1 Mayan MD, Gago-Fuentes R, Carpintero-Fernandez P, Fernandez-Puente P, Filgueira-Fernandez P, Goyanes N, et al. Articular chondrocyte network mediated by gap junctions: role in metabolic cartilage homeostasis. Ann Rheum Dis. 2015;74(1):275-84. [ Links ]
2 Mayan MD, Carpintero-Fernandez P, Gago-Fuentes R, Martinez-de-Ilarduya O, Wang HZ, Valiunas V, et al. Human articular chondrocytes express multiple gap junction proteins: differential expression of connexins in normal and osteoarthritic cartilage. Am J Pathol. 2013;182(4):1337-46. [ Links ]
3 Carpintero-Fernandez P, Gago-Fuentes R, Wang HZ, Fonseca E, Caeiro JR, Valiunas V, et al. Intercellular communication via gap junction channels between chondrocytes and bone cells. Biochim Biophys Acta Biomembr. 2018;1860(12):2499-505. [ Links ]
4 Varela-Eirín M, Varela-Vázquez A, Guitián-Caamaño A, Paíno CL, Mato V, Largo R, et al. Targeting of chondrocyte plasticity via connexin43 modulation attenuates cellular senescence and fosters a pro-regenerative environment in osteoarthritis. Cell Death Dis. 2018;9(12):1166. [ Links ]
5 Ghatnekar GS, O'Quinn MP, Jourdan LJ, Gurjarpadhye AA, Draughn RL, Gourdie RG. Connexin43 carboxyl-terminal peptides reduce scar progenitor and promote regenerative healing following skin wounding. Regen Med. 2009;4(2):205-23. [ Links ]
6 Ghatnekar GS, Grek CL, Armstrong DG, Desai SC, Gourdie RG. The effect of a connexin43-based Peptide on the healing of chronic venous leg ulcers: a multicenter, randomized trial. J Invest Dermatol. 2015;135(1):289-98. [ Links ]
7 Mendoza-Naranjo A, Cormie P, Serrano AE, Wang CM, Thrasivoulou C, Sutcliffe JE, et al. Overexpression of the gap junction protein Cx43 as found in diabetic foot ulcers can retard fibroblast migration. Cell Biol Int. 2012; 36(7):661-7. [ Links ]
8 Grogan SP, Miyaki S, Asahara H, D'Lima DD, Lotz MK. Mesenchymal progenitor cell markers in human articular cartilage: normal distribution and changes in osteoarthritis. Arthritis Res Ther. 2009;11(3):R85. [ Links ]
9 Rai MF, Sandell LJ. Regeneration of articular cartilage in healer and non-healer mice. Matrix Biol. 2014;39:50-5. [ Links ]
10 Varela-Eirín M, Carpintero-Fernández P, Sánchez-Temprano A, Varela-Vázquez A, Paíno CL, Casado-Díaz A, et al. Senolytic activity of small molecular polyphenols from olive restores chondrocyte redifferentiation and promotes a pro-regenerative environment in osteoarthritis. Aging (Albany NY). 2020;12(16):15882-905. [ Links ]
11 Varela-Eirín M V-VA, Blanco A, Caeiro JR, Mayán MD. A novel therapeutic target for osteoarthritis:control of cellular plasticity and senescence using connexin43. Revista de Osteoporosis y Metabolismo Mineral. 2019;11(2): 46-54. [ Links ]
Received: December 04, 2020; Accepted: January 10, 2021











 texto em
texto em 


