Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Revista de Osteoporosis y Metabolismo Mineral
versão On-line ISSN 2173-2345versão impressa ISSN 1889-836X
Rev Osteoporos Metab Miner vol.15 no.2 Madrid Abr./Jun. 2023 Epub 25-Set-2023
https://dx.doi.org/10.20960/revosteoporosmetabminer.00017
ORIGINALS
Follow-up and compliance to anti-osteoporotic treatment from nursing in a fracture liaison service
1Unidad FLS de Prevención de Fracturas. Hospital Provincial Nuestra Señora de Gracia. Zaragoza
Introduction:
compliance to anti-osteoporotic treatment is essential for the effectiveness of medications in clinical practice and is a priority objective for fracture liaison services (FLS).
Objectives:
to describe the follow-up and compliance to treatment of patients assisted by our FLS and identify the reasons for follow-up discontinuation.
Material and methods:
this is a descriptive, retrospective, and cross-sectional study of patients aged > 50 years with osteoporotic fractures treated in an FLS from 2016 through 2020. A descriptive statistical analysis of the variables collected was conducted using the SPSS software.
Results:
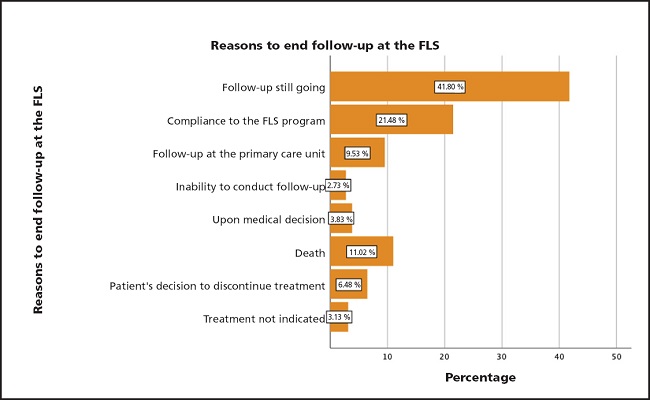
the sample included 1280 patients; 86.2 % were women and 13.8 % were men, 26.7 % of whom had received prior anti-osteoporotic treatment. After inclusion in the FLS, there was an increase of 59.6 % in patients who were started on anti-osteoporotic treatment and a 42.6 % increase in supplementation. A total of 4 different follow-up visits were conducted (at 5.4 months, 14.5 months, 24.3 months, and 33.8 months) with good compliance to treatment at around 72.1 %, 80.6 %, 83.1 %, and 83.7 %, respectively, and compliance to supplements at around 90.1 %, 90 %, 88.2 %, and 87.1 %, respectively. The reasons for follow-up discontinuation were completion of the follow-up program (21.48 %), death (11.02 %), transfer of follow-up to primary care (9.53 %), patient's decision (6.48 %), medical decision (3.83 %), treatment not indicated (3.13 %), and inability to continue follow-up (2.73 %).
Conclusions:
the inclusion of these patients in an FLS shows a high percentage of good compliance and improves the percentage of patients with osteoporotic fractures who are started on treatment. The most common reason for follow-up discontinuation was continuation of care by primary care physicians.
Keywords: Fracture liaison service; Fragility fracture; Medication compliance; Osteoporosis treatment; Case manager
INTRODUCTION
The World Health Organization (WHO) defines osteoporosis (OP) as a chronic disease characterized by low bone mass and deterioration of the microarchitecture of the bone tissue, leading to increased bone weakness and an increased risk of fractures (1,2).
The prevalence of osteoporosis is increasing due to the progressive aging of the population, and it is estimated to cause 9 million fractures worldwide annually, making up a serious public health problem with significant medical, social, and economic impact (1-5). It is known as a silent disease because it often progresses asymptomatically, and its first clinical or sentinel sign is often a fragility fracture (1-4,6,7).
Fragility fracture (FF) is defined as a fracture that occurs without trauma or with low-energy trauma, such as a fall from a height corresponding to standing height or less (1,8). It is estimated that approximately one in three women and one in five men over the age of 50 will experience, at least, one fragility fracture in their lifetime (1,6,8).
The most predictive factor for a FF is the presence of a previous fracture as it increases the risk of subsequent fractures or re-fractures within the next two years (9,10). This increased risk is known as imminent risk of fracture and can trigger what experts call a cascade of fractures (6,8-11).
Despite the wide range of anti-osteoporotic treatments (AOT), available there is a treatment gap, defined as the percentage of eligible individuals who do not receive osteoporosis medication (12,13). According to various studies published, it is estimated that between 63 % and 80 % of the individuals with fragility fractures do not receive any form of treatment, indicative that osteoporosis is possibly both underdiagnosed and undertreated (6,8,13-16).
In addition to the treatment gap, a serious problem is therapeutic compliance, which is clearly observed with the use of oral bisphosphonates, the most commonly prescribed pharmacological drugs these days (6,7,10,17-19).
Treatment compliance refers to adherence and is of great importance for the effectiveness of drugs in clinical practice (2,18,20,21). Factors affecting compliance are diverse, complex, and multidimensional being some associated with treatment itself and its administration schedule, and others with the patients' cognitive status and knowledge (2,14,18,20,21).
Therefore, in response to the urgent need for improving this situation, the International Osteoporosis Foundation (IOF) recommended the implementation, whenever possible, of Fracture Liaison Services (FLS) as a global strategy for secondary fracture prevention.
However, according to the IOF, FLS are available in < 10 % of hospitals in Spain (1,11,22).
The FLS model has become increasingly common, and there are various types of FLSs based on the care model used: types A, B, C, and D. Type A represents a coordinated approach to secondary fracture prevention with a central coordinator who identifies, investigates, and initiates treatment, and a follow-up program for patients included in the FLS (6,13,23,24). This approach begins with the identification of patients > 50 years of age with a recent FF followed by the evaluation of clinical risk factors for future fractures, possible causes of secondary osteoporosis, initiation of treatment, and appropriate long-term follow-up to improve compliance to anti-osteoporotic therapy (3,11,12,25).
Several studies have demonstrated the effectiveness and efficacy of FLS in various aspects of FF management including patient identification and increased treatment initiation rates (38 % vs 17.2 %), and improved compliance after sustaining a fracture (57 % vs 34.1 %), thus reducing the risk of new fractures (3,6,8,11,24,26).
The objective of this study is to describe the follow-up and compliance to anti-osteoporotic treatment and supplements in our FLS, and identify the reasons for follow-up discontinuation. Additionally, the study aims to determine the percentage of patients who initiate treatment.
MATERIAL AND METHODS
This study was approved by the Aragón Ethical Committee for Scientific Research (CEICA) of the Government of Aragon, Spain that issued a favorable opinion back in September 28, 2016, and all patients included received an information sheet and signed a written informed consent form.
A descriptive, retrospective, and cross-sectional study was conducted on patients treated at the Fracture Liaison Service (FLS) of Hospital Provincial Nuestra Señora de Gracia in Zaragoza, Aragón (Spain) since the establishment of this unit since November 1, 2016 up until December 31, 2020.
Our FLS is a type A model, operational since November 2016, that consists of a specialized medical coordinator in Traumatology, a specialist in Geriatrics and Gerontology, a case manager nurse, and a nursing care and administrative tasks technician.
The inclusion criteria in our FLS are: patients ≥ 50 years of age from Health Sector I, from Zaragoza and with any of the following diagnostic categories according to ICD-9-CM (International Classification of Diseases): vertebral fracture (805 and 806), pelvic fracture (808), proximal humerus fracture (812), distal radius and ulna fracture (813), and femoral neck fracture (820, 821). All patients are identified through the emergency department care registry and invited to a weekly consultation where they are offered voluntary inclusion in the unit.
Our follow-up protocol includes phone or in-person follow-ups for, at least, 2 years after the initiation of treatment (at 6 months, 1 year, and 2 years after treatment initiation). Various factors such as the patients' disease progression, therapeutic changes, and detection of fractures at follow-up impact the duration of personalized follow-up. For this study, all the follow-ups conducted on the selected sample were reviewed on 4 different occasions during the 3 years following their inclusion, and sometimes for longer periods, thus verifying therapeutic compliance to AOT and/or supplements administered.
This follow-up was mainly conducted by the case manager nurse, either in person or over the phone. To evaluate compliance to AOT and supplements during different follow-ups, a questionnaire was used that classified compliance as good if medication was used > 80 % of the time, fair if used between 50 % and 80 %, and poor if used < 50 % of the time. Additionally, the tolerance or intolerance to both AOT and supplements was recorded.
An important aspect of the follow-up was patient education and awareness provided by the case manager nurse through detailed written information in the clinical report at the initiation of treatment and during in-person follow-ups, as well as verbally during phone follow-ups. The importance of treatment regarding the risk of sustaining a new fracture and its implications for the patients' quality of life and independence was stressed out as well.
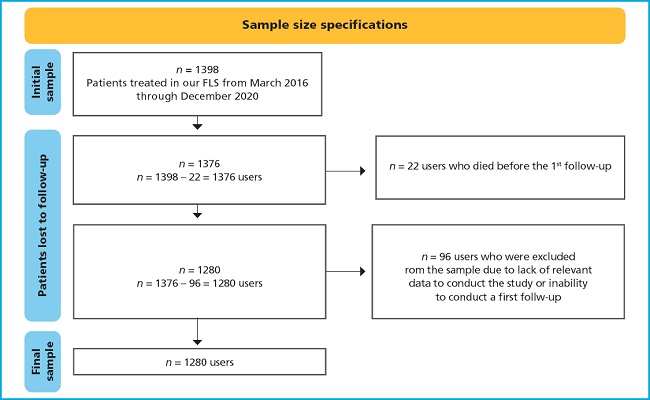
From an initial sample of 1398 patients included during the study period, the final sample of the study included a total of 1280 patients with detailed explanations of the exclusions made in figure 1.
A database was created in the SPSS program for demographic, clinical, initiation, follow-up, and compliance variables associated with anti-osteoporotic treatment and/or supplements, as well as the causes for follow-up discontinuation and risk of fracture. These variables were used for a descriptive analysis.
The variables analyzed in our study include demographic variables (gender, age, and mortality), general clinical variables (height, weight, body mass index), relevant past medical history (treatment with glucocorticoids over the past 6 months and organic diseases that may decrease bone mineral density or other risk factors associated with falling). For fracture risk assessment with the FRAX® tool, the guidelines published by Azagra et al. (27) were followed, which adjusted the FRAX® for a Barcelona population, describing thresholds that stratify the risk of major fracture as < 5 % for low risk, ≥ 5 % and < 7.5 % for intermediate risk, and ≥ 7.5 % for high risk of fracture (23,27). The number of falls within the year prior to the index fracture, the location of index fractures, and the presence of previous fractures were documented.
Regarding the variable of supplements prescribed in the FLS, the milligrams of calcium used in the diet were estimated using a calcium intake calculator.
Compliance and tolerance variables to AOT and supplements were collected in the 4 follow-ups conducted. Finally, the variable of causes of follow-up discontinuation was analyzed including compliance of the FLS program, follow-up by primary care physician (referral of follow-up to the patient's primary care physician for various reasons like patient preference, initiation of supplements only, etc.), inability to conduct the follow-ups (inability to contact the patient during the follow-ups scheduled), medical decision (when discontinuation was indicated by a clinician assisting the patient, whether the FLS coordinator or a different healthcare professional assisting the patient for other reasons), mortality, treatment discontinuation by patient decision, and treatment not indicated.
Quantitative variables were analyzed as mean ± standard deviation, while the qualitative ones were analyzed as absolute frequency and percentage. A univariate descriptive statistical analysis was performed using the “SPSS Statistics” version 22 for Mac, with statistical significance set at p values < 0.05.
RESULTS
Out of the 1280 patients selected for our study, 1103 (86.2 %, 95 %CI, 84.16–88.02) were women and 177 (13.8 %, 95 %CI, 11.98-15.84) were men, with a mean age of 82.1 ± 9.9 years (Kolmogorov-Smirnov test for normality; p < 0.05.). The mean age in men was 84.3 ± 8.3 years, and 81.7 ± 10.2 years in women.
Table I shows a descriptive analysis of the clinical variables studied.
Table I. Clinical variables. sites of index fractures #1 and #2, and presence of prior fractures before inclusion in the FLS.
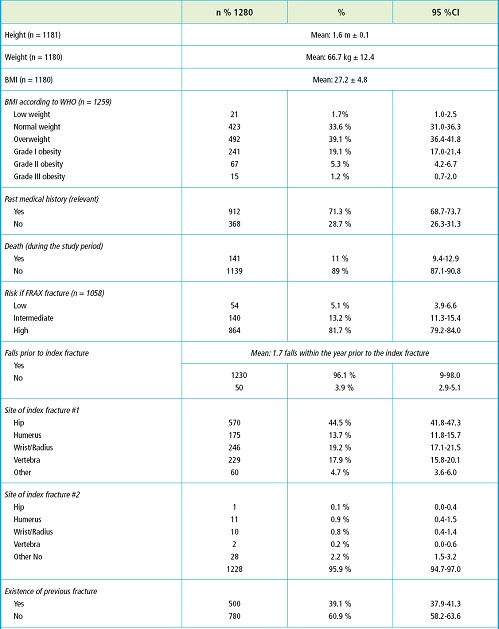
BMI: body mass index; Fx: fracture; FLS: fracture liaison service; WHO: World Health Organization.
All patients in our sample had at least one index fracture, which was a prerequisite to be included in the FLS. Additionally, 6.3 % had two index fractures, and 1.9 % three index fractures during recruitment. Furthermore, 39.1 % had previously sustained some type of prior fracture before the index fracture. Among patients with a past medical history of fracture prior to the index fracture, 30.5 % had sustained a major fracture (5.3 %, hip; 5.2 %, humerus; 7.7 %, wrist; 12.1 % vertebra) while the remaining 8.5 % had sustained fractures in different locations. Regarding previous falls including the fall that led to their referral to our FLS, the mean number of falls in the year prior to inclusion was 1.7.
Regarding treatment, only 26.7 % of the patients had received AOT and 34.8 % supplements prior to inclusion. After evaluation in the FLS, 83.3 % received AOT, and 77.4 % supplements. The most prescribed drug after inclusion in the FLS was alendronate (44.9 %) followed by denosumab (40.6 %), risedronate (6.8 %), teriparatide (7.6 %), and IV zoledronic acid (0.1 %). Combined calcium and vitamin D supplements were prescribed to 63.1 % of the patients, and vitamin D alone was prescribed to 36.9 % of the patients.
In our study, the mean time elapsed from treatment initiation to the first follow-up was 5.4 ± 4.8 months. The mean time from treatment initiation to the second follow-up was 14.5 ± 7.4 months, to the third follow-up was 24.3 ± 8.9 months, and to the fourth follow-up was 33.8 ± 14.0 months.
Regarding follow-up continuity, out of the 1280 FLS users who received the first follow-up, 933 (72.9 %) had a second follow-up, 551 (43 %) had a third follow-up, and 209 (16.3 %) a fourth follow-up.
Table II shows the type of follow-up conducted at each control, and compliance to TAO and supplements, and tolerance to both in each individual follow-up. A good compliance to TAO was seen during the 1st, 2nd, 3rd, and 4th follow-ups with rates of 72.1 %, 80.6 %, 83.1 %, and 83.7 %, respectively. Regarding supplements, proper compliance was seen in the during the 1st, 2nd, 3rd, and 4th follow-ups with rates of 90.1 %, 90 %, 88.2 %, and 87.1 %, respectively. Regarding tolerance, the figures obtained for TAO exceeded 88 % in all follow-ups except the 1st one (77.4 %); regarding supplements, tolerance was > 94 % in all the follow-ups conducted.
Table II. Compliance and tolerance of AOT and supplements at the follow-ups.
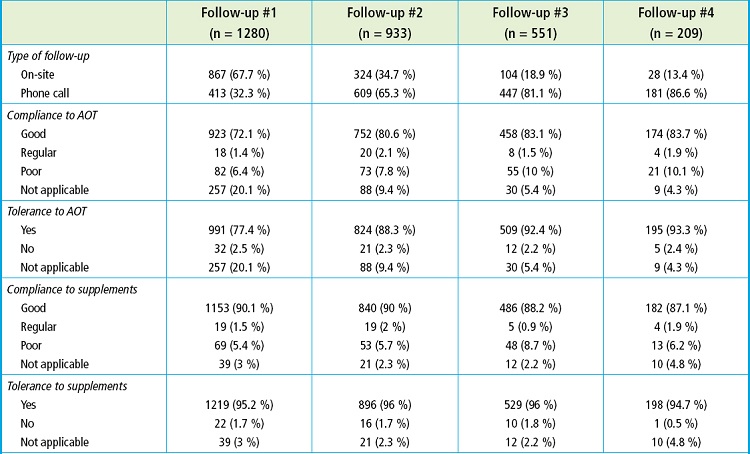
AOT: anti-osteoporotic treatment.
At the time of data collection, 41.8 % of the patients were still included in the follow-up program while 58.2 % had completed the follow-up. Regarding the reasons for ending the follow-up, the most common reason was compliance with the FLS follow-up program (21.48 %) followed by death (11.02 %), follow-up by the patient's primary care physician (9.53 %), patient's decision (6.48 %), medical decision (3.83 %), treatment not indicated (3.13 %), and the impossibility to contact the patient for follow-up reason (2.73 %). The percentage distribution of the reasons for ending the follow-up is shown on figure 2.
DISCUSSION
This study reports the experience gained from implementing an FLS in our hospital to determine the basic profile of patients treated in the unit and shows data on follow-up and compliance to anti-osteoporotic treatment and calcium and vitamin D supplements.
Regarding the presence of previous fractures before the index fracture as the reason why patients are enrolled in our FLS, 39.1 % had sustained a previous fracture (in some cases, up to 3 previous fractures), which is higher compared the findings reported by Ojeda (23), where only 19 % of users had sustained a previous fracture before.
We should mention that the mean BMI of our sample was 27.21 kg/m2 similar to the results obtained by Azagra et al. (27). Furthermore, only 1.7 % of our patients had BMIs < 18.5 kg/m2, which is similar to the figures provided by the study conducted by Naranjo et al28 who found a 1.4 % rate in that BMI range. In our case, 64.7 % of patients were overweight or obese.
A total of 81.7 % of the sample had a high risk of fracture, which is consistent with the profile of patients treated in an FLS who have already sustained, at least, 1 fracture. This stresses the importance of previous fracture when it comes to determining the risk of future fractures and reinforces the importance of initiating anti-osteoporotic treatment as soon as possible. These are conclusions also reached in the studies conducted by Walters et al. (6), De Bruin et al. (12), Borgström et al. (13), and Wu et al. (11).
Therefore, the profile of patient who is often examined in our unit would is that of an approximately 82-year-old woman who has sustained an osteoporotic index fracture, who is overweight, and who has relevant past medical history of osteoporosis with a high risk of fracture according to FRAX and is not on anti-osteoporotic treatment despite nearly 40 % have sustained a previous fracture before the index fracture.
Our study shows a high percentage of hip fractures as index fractures (44.5 %). This could be due, on the one hand, to the presence of an orthogeriatric unit at the hospital where our FLS is located, with which we work collaboratively for secondary fracture prevention. On the other hand, it could be a common finding in most FLSs that capturing hip fractures is easier since these patients require hospital admission. Our study shows a high number of hip fractures as the index fracture. In our case, within the first year of unit activity, the focus of patient recruitment was almost exclusively on hip fractures. Our results differ from former studies that present different FLS models and rates of patient recruitment. For example, in the study conducted by Luc et al. (8), they only had 9 % of the patients with hip index fractures, and in the study conducted by Borrgström et al. (13) they obtained only 19.6 % among their participants.
The mean number of falls sustained by our patients in the year prior to inclusion in the FLS (including the one that caused the index fracture) was 1.7. We believe that this data greatly underestimates the actual number of previous falls since it is collected retrospectively from the patients themselves or their relatives/caregivers who often do not remember falls that did not have the clinical significance of a fracture.
Regarding the type of treatment initiated, a high percentage of patients received alendronate (44.9 %), which is consistent with the national clinical guidelines during that period of time, and with the study conducted by Walters et al. (6). The high percentage of patients who received denosumab (40.6 %) is consistent with the fact that a high percentage of patients are very old, have a high prevalence of hip fractures, are on multiple drugs, and have significant comorbidities. Additionally, in our FLS, IV zoledronic acid was not administered except in some exceptional cases.
On the other hand, studies such as those conducted by Gómez-Navarro et al. (4), Walters et al. (6), and Ojeda (23) highlight the high percentage of patients who were not on any pharmacological treatment prior to being included in the FLS. Our study shows similar figures, specifically, 73.3 % of our patients were not on any prior pharmacological treatment. These data are similar compared to those from other studies that assessed treatment gap like the one conducted by Hiligsmann et al. (14) that estimated that treatment gap in 2019 went from 25 % to 95 % in European countries. In addition, according to the IOF report from 2021, treatment gap in high risk patients was a mean 71 %. However, when adjusting for sex, 71.5 % of women and 84.2 % of men were not on prior treatment, data somehow slightly different from the findings reported by Borgström et al. (13) who saw, back in 2020, that treatment gap in Europe was greater in women (73 %) compared men (63 %). Our study highlights a low percentage of patients receiving prior anti-osteoporotic treatment when the index fracture was sustained (26.7 %). However, reliable information regarding the prescription of such treatment in patients with or without a previous fracture could not be obtained to determine if the difference between the two groups was significant.
The data obtained show a higher number of patients receiving anti-osteoporotic treatment and supplements after being assisted at our FLS. Specifically, there was a 59.6 % increase in the use of anti-osteoporotic treatment and a 42.6 % increase in the use of supplements. This increase in the percentage of patients on treatment after FLS enrollment is also found in the results obtained by Axelsson et al. (29).
Regarding the follow-ups conducted, it was found that they reasonably abided by the initial protocol, although time ranges were too wide compared to the mean.
Regarding treatment compliance and supplements evaluated in each follow-up, we believe that the follow-up program of our FLS was crucial to achieve good compliance to anti-osteoporotic treatment (TAO) and supplements. Data on good compliance obtained throughout the entire follow-up period are satisfactory compared to the treatment gap discussed earlier in patients not included in FLS programs. At the first follow-up, good compliance was seen in 72.1 % of the patients, a percentage that went up in subsequent follow-ups. Within the second follow-up, the rate of good compliance to TAO was 80.6 %, within the third follow-up it was 83.1 %, and within the fourth follow-up, it went up to 83.7 %. This progressive increase in compliance over time was also reported by Walters et al. (6). However, these results differ from those found by Ojeda (23) and Naranjo et al. (28) as these studies did not find significant difference in the percentages of good compliance among follow-ups. We should mention that the study sample shows the number of patients included in the FLS from 2016 through 2020. Therefore, a percentage of patients included in 2019 and 2020 would not have reached 2 years since their inclusion and never had a third or fourth follow-up. The lower compliance rate seen within the 1st follow-up compared to the subsequent ones is striking. We do not know the exact reason for this, but it could be that adverse effects and treatment intolerances typically appear at the beginning of treatment, and until the patients are visited (in-person or by phone) at the 1st follow-up and treatment is adjusted, they may not fully comply to it.
Finally, regarding the causes for ending the follow-up in our FLS, the most common cause was completion of the follow-up program (21.48 % of patients), which in our case is typically 2 years, with some exceptions as previously mentioned. The second cause was mortality at the study period (11 % of the cases). Similar findings have been reported by Kanis et al. (26) who found a 15 % mortality rate among their participants. Only 6.48 % of patients discontinued treatment and, therefore, ended their follow-up by their own decision. We believe that this data probably does not reflect the reality as a whole, and the rate of treatment discontinuation is underestimated since the data obtained are self-reported by the patients and may not accurately represent the actual situation. At the end of the follow-up program, patients transition to being monitored by their primary care physician. The limited duration of follow-up in an FLS underscores the importance of a good relationship and communication with primary care units to maintain treatment compliance beyond the temporal scope of an FLS. Despite the optimistic results regarding compliance in our study, we should mention a free limitations. Firstly, it is a retrospective study, which limits the amount and quality of information available. Additionally, the patient sample is treated as a homogeneous group, which is not consistent with reality as different comorbidities, cognitive status, and social support can influence the patients' compliance capabilities. Secondly, regarding the assessment of treatment compliance, we should mention that information comes from the patients themselves and may differ to some extent from reality. In addition, there was no information available on effective drug withdrawal from pharmacies until the implementation of electronic health records within the final months of the study period, thus making it impossible to draw conclusions on long-term treatment persistence. Finally, there was no control group of patients not included in an FLS for comparison purposes.
On the other hand, one of the strengths of the study is the large number of patients included in the sample and each follow-up (despite the progressive loss of patients) with a structured follow-up program for a minimum period of up to 2 years, which allows obtaining relevant data on the impact of an FLS on treatment initiation and compliance.
In conclusion, this study describes the impact of our FLS on the initiation of anti-osteoporotic treatment and compliance to such treatment over the course of follow-up. The inclusion of these patients in an FLS appears to improve the percentage of patients with a previous osteoporotic fracture who receive preventive treatment significantly. In addition, the active follow-up conducted by the case manager nurse could be a determinant factor to improve treatment compliance in the early years after the fracture, thus reducing the risk of re-fracture.
REFERENCES
1. Pennestrì F, Corbetta S, Favero V, Banfi G. Fragility Fracture Prevention-Implementing a Fracture Liaison Service in a High Volume Orthopedic Hospital. Int J Environ Res Public Health 2019;16(24):4902. DOI: 10.3390/ijerph16244902 [ Links ]
2. Garcia E, Fuentes JE. Adherencia y cumplimiento al tratamiento de la osteoporosis. Farma Journal 2016;1(2):125-32. [ Links ]
3. Noordin S, Allana S, Masri BA. Establishing a hospital based fracture liaison service to prevent secondary insufficiency fractures. Int J Surg 2018;54(Pt B):328-32. DOI: 10.1016/j.ijsu.2017.09.010 [ Links ]
4. Gómez Navarro R, González García P, Martín Hernández C, Castro Sauras A, Valdearcos Enguídanos S. Prevención primaria y secundaria de la fractura de cadera por fragilidad ósea en la población del sector sanitario Teruel. Rev Esp Salud Pública 2017;9. [ Links ]
5. Amphansap T, Stitkitti N, Dumrongwanich P. Evaluation of Police General Hospital's Fracture Liaison Service (PGH's FLS): The first study of a Fracture Liaison Service in Thailand. Osteoporos Sarcopenia 2016;2(4):238-43. DOI: 10.1016/j.afos.2016.09.002. [ Links ]
6. Walters S, Khan T, Ong T, Sahota O. Fracture liaison services: improving outcomes for patients with osteoporosis. Clin Interv Aging 2017;12:117-27. DOI: 10.2147/CIA.S85551 [ Links ]
7. Jaleel A, Saag KG, Danila MI. Improving drug adherence in osteoporosis:an update on more recent studies. Ther Adv Musculoskelet Dis 2018;10(7):141-9. DOI: 10.1177/1759720X18785539 [ Links ]
8. Luc M, Corriveau H, Boire G, Filiatrault J, Beaulieu MC, Gaboury I. Patient-Related Factors Associated with Adherence to Recommendations Made by a Fracture Liaison Service: A Mixed-Method Prospective Study. Int J Environ Res Public Health 2018;15(5):944. DOI: 10.3390/ijerph15050944 [ Links ]
9. Nakayama A, Major G, Holliday E, Attia J, Bogduk N. Evidence of effectiveness of a fracture liaison service to reduce the re-fracture rate. Osteoporos Int 2016;27(3):873-9. DOI: 10.1007/s00198-015-3443-0 [ Links ]
10. Skjødt MK, Khalid S, Ernst M, Rubin KH, Martinez-Laguna D, Delmestri A, et al. Secular trends in the initiation of therapy in secondary fracture prevention in Europe: a multi-national cohort study including data from Denmark, Catalonia, and the United Kingdom. Osteoporos Int 2020;31(8):1535-44. DOI: 10.1007/s00198-020-05358-4 [ Links ]
11. Wu CH, Tu ST, Chang YF, Chang DC, Chien JT, Lin CH, et al. Fracture liaison services improve outcomes of patients with osteoporosis-related fractures: A systematic literature review and meta-analysis. Bone 2018;111:92-100. DOI: 10.1016/j.bone.2018.03.018 [ Links ]
12. De Bruin IJA, Wyers CE, van den Bergh JPW, Geusens PPMM. Fracture liaison services: do they reduce fracture rates? Ther Adv Musculoskelet Dis 2017;9(7):157-64. DOI: 10.1177/1759720X17706464 [ Links ]
13. Borgstrüm F, Karlsson L, Ortsäter G, Norton N, Halbout P, Cooper C, et al. Fragility fractures in Europe: burden, management and opportunities. Arch Osteoporos 2020;15(1):59. DOI: 10.1007/s11657-020-0706-y [ Links ]
14. Hiligsmann M, Cornelissen D, Vrijens B, Abrahamsen B, Al-Daghri N, Biver E, et al. Determinants, consequences and potential solutions to poor adherence to anti-osteoporosis treatment: results of an expert group meeting organized by the European Society for Clinical and Economic Aspects of Osteoporosis, Osteoarthritis and Musculoskeletal Diseases (ESCEO) and the International Osteoporosis Foundation (IOF). Osteoporosis International 2019;30(11):2155-65. DOI: 10.1007/s00198-019-05104-5 [ Links ]
15. Heyman N, Etzion I, Ben Natan M. A coordination project for improvement of osteoporosis medication use among patients who sustained an osteoporotic fracture: The Israeli experience. Osteoporos Sarcopenia 2018;4(4):134-9. DOI: 10.1016/j.afos.2018.11.084 [ Links ]
16. Yeap SS, Nur Fazirah MFR, Nur Aisyah C, Zahari Sham SY, Samsudin IN, C Thambiah S, et al. Trends in post osteoporotic hip fracture care from 2010 to 2014 in a private hospital in Malaysia. Osteoporos Sarcopenia 2017;3(2):112-6. DOI: 10.1016/j.afos.2017.05.001 [ Links ]
17. García-Sempere A, Hurtado I, Sanfélix-Genovés J, Rodríguez-Bernal CL, Gil Orozco R, PeiróS, et al. Primary and secondary non-adherence to osteoporotic medications after hip fracture in Spain. The PREV2FO population-based retrospective cohort study. Sci Rep 2017;7(1):11784. DOI: 10.1038/s41598-017-10899-6 [ Links ]
18. Orimo H, Sato M, Kimura S, Wada K, Chen X, Yoshida S, et al. Understanding the factors associated with initiation and adherence of osteoporosis medication in Japan: An analysis of patient perceptions. Osteoporos Sarcopenia 2017;3(4):174-84. DOI: 10.1016/j.afos.2017.10.002 [ Links ]
19. Fatoye F, Smith P, Gebrye T, Yeowell G. Real-world persistence and adherence with oral bisphosphonates for osteoporosis: a systematic review. BMJ Open 2019;9(4):e027049. DOI: 10.1136/bmjopen-2018-027049 [ Links ]
20. Swart KMA, van Vilsteren M, van Hout W, Draak E, van der Zwaard BC, van der Horst HE, et al. Factors related to intentional non-initiation of bisphosphonate treatment in patients with a high fracture risk in primary care: a qualitative study. BMC Family Practice 2018;19(1):141. DOI: 10.1186/s12875-018-0828-0 [ Links ]
21. Blanch J, Casado E, González J, Valdés C, Ruiz-Baena J, Palomino R, Nogués X. Percepción de los profesionales médicos respecto la adherencia terapéutica de los pacientes con osteoporosis. Rev Osteoporos Metab Miner 2016;8(1):5-23. DOI: 10.4321/S1889-836X2016000100003 [ Links ]
22. Axelsson KF, Johansson H, Lundh D, Möller M, Lorentzon M. Association Between Recurrent Fracture Risk and Implementation of Fracture Liaison Services in Four Swedish Hospitals: A Cohort Study. J Bone Miner Res 2020;35(7):1216-23. DOI: 10.1002/jbmr.3990 [ Links ]
23. Ojeda PS. Programa para la prevención secundaria de la fractura por fragilidad en el Área Norte de Gran Canaria, coordinado por reumatólogos, con la participación de enfermería y en colaboración con atención primaria. [Tesis doctoral]. Gran Canaria:Universidad de Las Palmas de Gran Canaria;2016. Recuperado a partir de: http://hdl.handle.net/10553/19367 [ Links ]
24. Ganda K, Puch M, Chen JS, Speerin R, Bleasel J, Center JR, et al. Models of care for the secondary prevention of osteoporotic fractures: a systematic review and meta-analysis. Osteoporosis Int 2013;24:393-406. DOI: 10.1007/ss00198-012-2090-y [ Links ]
25. Willers C, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M, et al. Osteoporosis in Europe: a compendium of country-specific reports. Arch Osteoporos 2012;17(23):1-129. DOI: 10.1007/s11657-021-00969-8 [ Links ]
26. Kanis JA, Norton N, Harvey NC, Jacobson T, Johansson H, Lorentzon M, et al. SOPE 2021: a new scorecard for osteoporis in Europe. Arch Osteoporos 2021;16(82):1-82. DOI: 10.1007/s11657-020-00871-9 [ Links ]
27. Azagra R, Roca G, Martín-Sánchez JC, Casado E, Encabo G, Zwart M, et al. Umbrales de FRAX®para identificar personas con alto o bajo riesgo de fractura osteoporótica en población femenina española. Med Clin (Barc) 2015;144(1):1-8. [ Links ]
28. Naranjo A, Ojeda-Bruno S, Bilbao-Cantarero A, Quevedo-Abeledo JC, Diaz-González BV, Rodríguez-Lozano C. Two-year adherence to treatment and associated factors in a fracture liaison service in Spain. Osteoporos Int 2015;26:2579-85. DOI: 10.1007/s00198-015-3185-z [ Links ]
29. Axelsson KF, Jacobsson R, Lund D, Lorentzon M. Effectiveness of a minimal resource fracture liaison service. Osteoporos Int 2016;27(11):3165-75. DOI: 10.1007/s00198-016-3643-2 [ Links ]
Received: October 10, 2022; Accepted: May 22, 2023











 texto em
texto em