INTRODUCTION
Cicatricial alopecia, also identified as cicatricial or scarring alopecia, is a rare, but significant group of trichologic disorders characterized by irreversible loss of hair follicles resulting in scarring and permanent hair loss [1]. It presents as a loss of follicular ostia in clinical manifestation and destruction of hair follicle in histological investigation [2]. Patients affected by scarring alopecia present with symptoms including; pain, burning, severe itching, quick disease progression, and gradual hair loss [3].
Cicatricial alopecia can be categorized into primary and secondary cicatricial alopecia. In primary cicatricial alopecia, the hair follicle itself is the main target of the disease or its related adventitial dermis with relative sparing of the interfollicular reticular dermis, while in the secondary type, pathological alteration begins from non-follicular dermis, which eventually damages the hair follicle's stem cell-based capacity for repeated regeneration [4, 5]. The main causes of primary cicatricial alopecia are lichen planopilaris, discoid lupus erythematosus, pseudoplade of Brocq, and folliculitis decalvans, whereas trauma, burns, carcinoma, sarcoidosis, and infection are considered as the main causes of secondary cicatricial alopecia [6, 7].
Previous histopathological studies revealed divided the patterns cicatricial alopecia into; lymphocytic, neutrophilic, mixed, and nonspecific types.1 The main classes of primary cicatricial alopecia are neutrophilic group (eg, folliculitis decalvans, dissecting cellulitis), lymphocytic (eg, liche n planopilaris, chronic cutaneous lupus erythematosus, classic pseudopelade of Brocq, central centrifugal cicatricial alopecia), and mixed group (eg, folliculitis keloidalis) [8, 9]. This category is crucial because diverse treatment approaches may be applied depending on the histological type of cicatricial alopecia [10]. Although there is no expectation for regrowth of destructed hair, there is a chance to stop the progression of disease through initial and accurate diagnosis [2]. The major histological type o bserved in some studies was lymphocytic, while other studies reported neutrophilic as the main the type [11]. Cicatricial alopecia can be diagnosed by biopsy generally of new lesions, as stated in previous study [12].
There is a paucity of data on cicatricial alopecia types presented with patients in Libya, hence the current study aimed at evaluating the epidemiological and clinicopathological features of cicatricial alopecia among Libyan population attended outpatient department of dermatology of the Tripoli central hospital in Libya.
METHODS
This study was performed on the archives of 31 patients diagnosed with cicatricial alopecia, referred to outpatient department of dermatology, Tripoli Central Hospital from Jan 2018 to Dec 2019. Patient consent form was obtained from all participated cases and the study approved by the Ethic Committee of department of dermatology, faculty of Medicine, the University of Tripoli, Libya (Ethical approval number. 1201-2019). All patients diagnosed with cicatricial alopecia based on pathology report from a specialist in dermatology were included in this epidemiological study. Patients with secondary causes of cicatricial alopecia that may mimic these disorders were excluded.
All the patients had undergone lesion biopsy and tricoscopic examination. The collected data including type of lesions, gender, age and type of lesion based on skin biopsy and trichoscopic finding were analyzed using SPSS software version 22. The findings are presented in Mean ± Standard deviation. For statistical analysis, the Chi-Square test was used to examine the relationship between different variables. P-value < 0.05 was considered statistically significant.
RESULTS
A total of 31 patients with diagnosis of cicatricial alopecia including 22 females (71%) and 9 males (29%) were participated in this study. The range of age was 15 to 55 years old. Most of the cases were from 36-42 years old. 16.1% of patients suffered from lichen planopilaris (LPP) (4 female and 1 male), 25.8% discoid lupus erythematosus (DLE) (5 female and 3 male), 6% Folliculitis decalvans (4 female and 4 male), 6.45% pseudopelade of Brocq (2 female and no male) and 16.12% Frontal fibrosing alopecia (5 female and no male).
Out of 31 cases, 20 (64.5%) patients with lymphocytic lesions and 11 (35.5%) patients with neutrophilic exudation were noticed. There were 16 females and 4 males with lymphocytic exudation and 6 females and 5 males with neutrophilic exudation, nevertheless there were no statistically significance difference between the type of lesion and gender (P-value > 0.05) (Table 1).
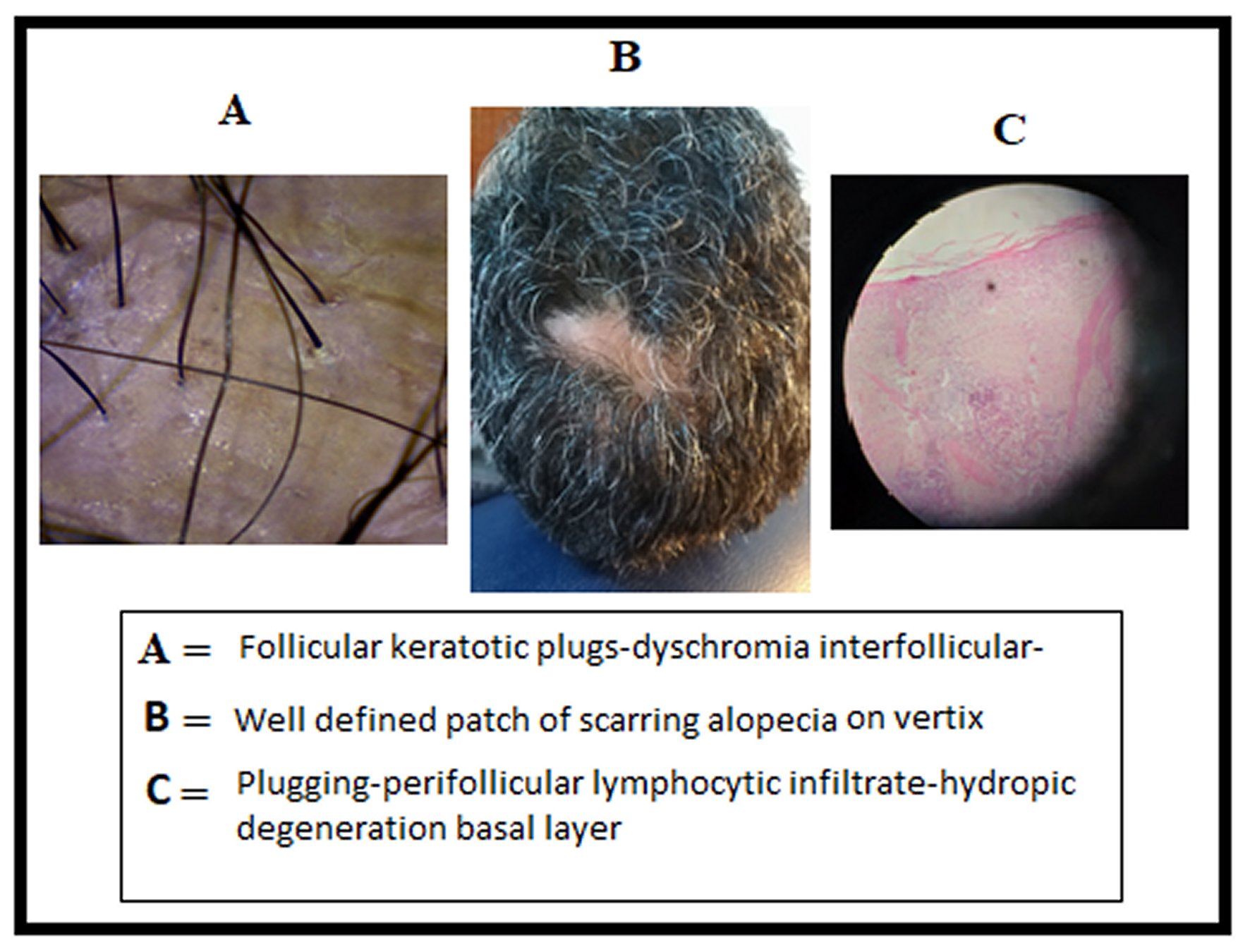
The mean age of patients with lymphocytic lesion was 45.5±1.2 years old whereas for neutrophilic lesion was 38.8±1.5 years old respectively but there were no significant association among mentioned data (P-value > 0.05). Trichoscopic results revealed that most of patients presented with Follicular keratotic plugs hyperkeratosis. Figure 1 summarizes the clinicopathological and trichoscopic features of discoid lupus erythematosus.
DISCUSSION
Cicatricial alopecias are important group of disorders that cause destruction of follicular ostia and may lead to permanent hair loss [13]. These various disorders can arise mainly due to radiation, burn and infections [14]. There is limited data about the global epidemiology of lesions, while early diagnosis and treatment can help in proper control of this condition.
In this current study, we aimed to evaluate 31 cases presented with cicatricial alopecias with the majority of these cases were 22 females (71%). Similarly, females were affected more than males in previously reported results [8, 15]. This might clarify by the fact that females are more probable to ask for medical consultation for skin disorders. On the other hand, a study conducted in Iran reported that 52% patients were males; this may due to the higher amount of neutrophilic cicatricial alopecia that frequently affects male [3]. Certainly, earlier study has revealed that neutrophilic cicatricial alopecia is more frequently seen in middle-aged males, and that lymphocytic cicatricial alopecia is more common among middle-aged females [8]. Our results also represent a wide range of patient age ranged from 15-55 years; nonetheless the disease was more frequent among the middle-aged patients. This outcome is in line with the results reported by earlier studies [16, 17, 18].
The clinicopathological results of our study reported that lymphocytic cicatricial alopecia occurred more commonly than neutrophilic one but rate was not statistically significant (P value > 0.05). The rate exhibited in our study is higher than the rate reported in previous studies, which could have occurred due to racial differences or dissimilarity in data collection [16].
The reported higher rate of patients with lymphocytic lesions in our study was in line with other earlier reports [19]. Lymphocytic types of cicatricial lesions diagnosed through biopsy were lichen-plano pilaris, discoid lupus erythematosus, frontal fibrosing alopecia, and pseudoplade of Brocq. The most common type of lymphocytic lesions was discoid lupus erythematosus (25.8% of all patients). This higher rate of discoid lupus erythematosus in our study was similar to previous results reported by Naeini et al. 2017, which presented a rate of 22.3% of affected patients and mostly were middle-age females [20].
Patients with neutrophilic exudation lesions exhibited tufting hair-follicular and loss of follicular ostia as seen by tricoscopic examination, with rate of 35.4%. However, the percentage of affected patients is higher than other studies [14]. Follicular keratotic plugs, follicular hyperkeratosis, and Peripilar tubular cast in our patients were mostly seen with lymphocytic exudate lesions.
The overall goal for treating the cicatricial alopecias is to diminish the inflammation process by giving immunosuppression or to eliminate microbes through the use of antimicrobial agents [17]. In our study, most of the included patients were treated with some oral medications such as oral corticosteroids and hydroxychloroquine or through the use of local drugs such as triamcinolone acetonide or the betamethasone dipropionate topical cream, with prospective results.
CONCLUSIONS
We have examined, in this study, several cases of histologically confirmed cicatricial alopecia obtained from Libyan patients. Our results reveled that cicatricial alopecia is more frequent in female patients than males. Histologically, the prevalence of lymphocytic lesion of cicatricial alopecia is higher than neutrophilic type. Moreover, cicatricial alopecia was exhibited to be more common among middle-aged patients. Further studies are desirable to elucidate the pathogenesis of cicatricial alopecia. Moreover, early treatment could help in preventing the progression of this disorder.