INTRODUCTION
Hypersensitivity pneumonitis (HP), also called extrinsic allergic alveolitis, is a respiratory syndrome involving the lung parenchyma specifically the alveoli, terminal bronchioles and alveolar interstitium. HP is an immune mediated interstitial lung disease (ILD). A population-based study estimated the annual incidence of interstitial lung diseases as 30:100,000 and HP accounted for less than 2% of these cases [1].The prevalence rates for hypersensitivity pneumonitis is less than 2 per 100,000 persons, and 1-year cumulative incidence rates ranges from 1.28 to 1.94 per 100,000 persons [2, 3]. HP is a rare entity except in certain professions, as an example the prevalence of farmer's lung was found to be 4.2/1000 farmers [4]. In India HP was found to be the most common type of ILD diagnosed in 47.3% of patients in the ILD-India registry [5].
Bagassosis is a rare cause of HP caused by significant exposure to bagasse. Bagasse is the fibrous sugarcane residue after extraction of sugarcane juice. The inhalation of bagasse is the cause of bagassosis. India has a large sugarcane industry. Bagasse with its high fibre content is used in manufacturing products like hard boards, paper mill, building material and bricks. Western Maharashtra is the sugarcane belt of Maharashtra. There is abundance of bagasse in this region. In addition to its use in industry, bagasse is also used as cheap fuel in brick- kilns to bake bricks. Workers are exposed to bagasse dust while handling it. Hypersensitivity pneumonitis results from inhalation of the bagasse dust contaminated by thermophilic actinomycetes, most importantly Thermoactinomycetes vulgaris. The irritant property of bagasse itself and micro-organisms including fungi that grow in it are the likely cause of widespread bronchoconstriction in the peripheral bronchopulmonary tree as seen in other extrinsic allergic alveolitis. We report a case of bagassosis in a brick-kiln worker where bagasse was used as fuel.
CASE REPORT
A twenty-five years old male, brick-kiln worker, reported with the complaints of low-grade fever, dry cough, shortness of breath, loss of appetite and unmeasured weight loss of one-month duration. The fever was continuous, low grade without chills. The cough was non-productive, without any aggravating or relieving factor. Patient also had breathlessness that increased during work and lessen during off-hours. The patient was comparatively symptom free during weekly offs. There was no history suggestive of allergic rhinitis, recurrent respiratory tract infections or asthma in past. The patient's occupational history revealed that he was a labourer in a brick-kiln for five years where bagasse and coal dust was used as the fuel and the workers were exposed to clay, coal and bagasse dust.
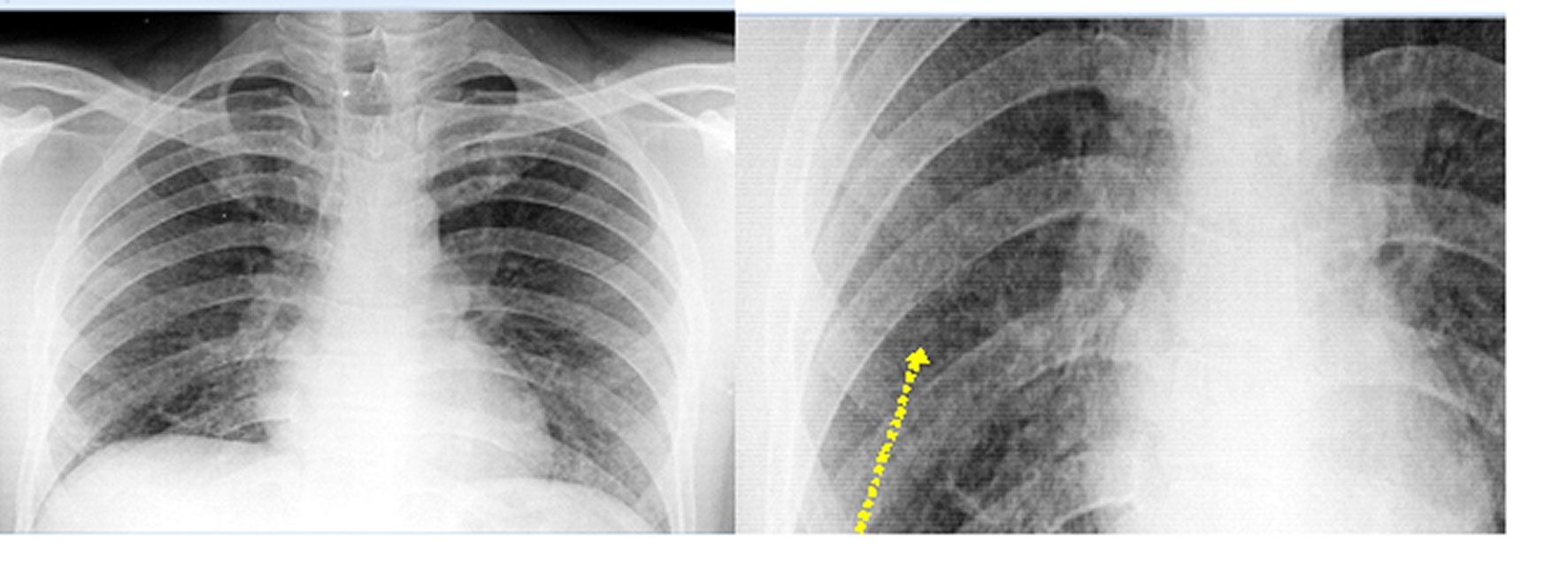
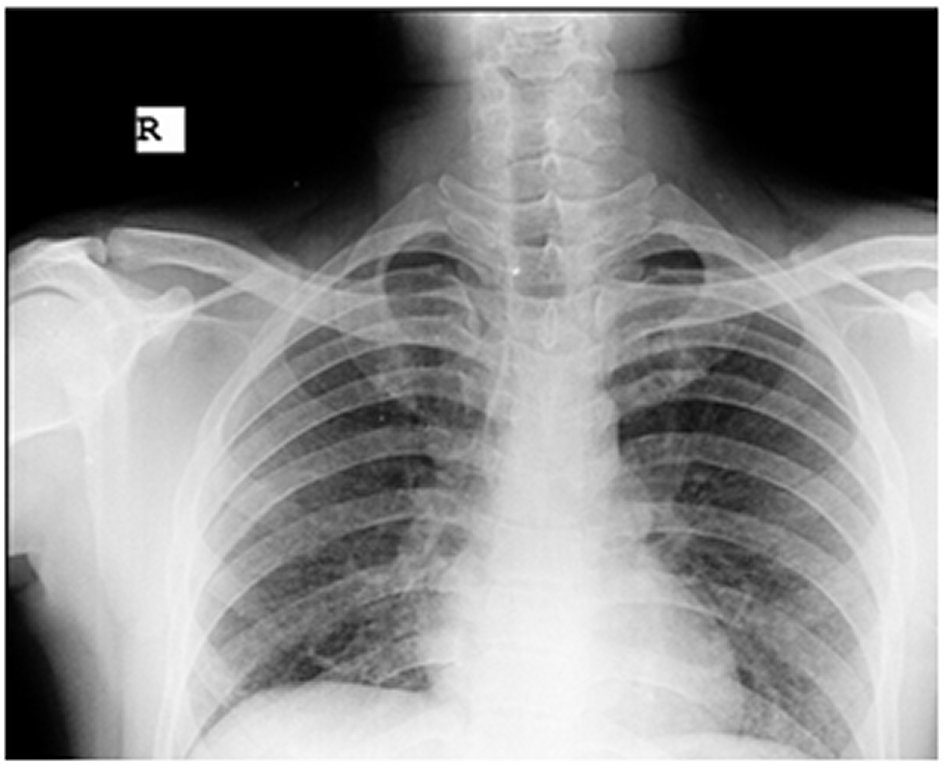
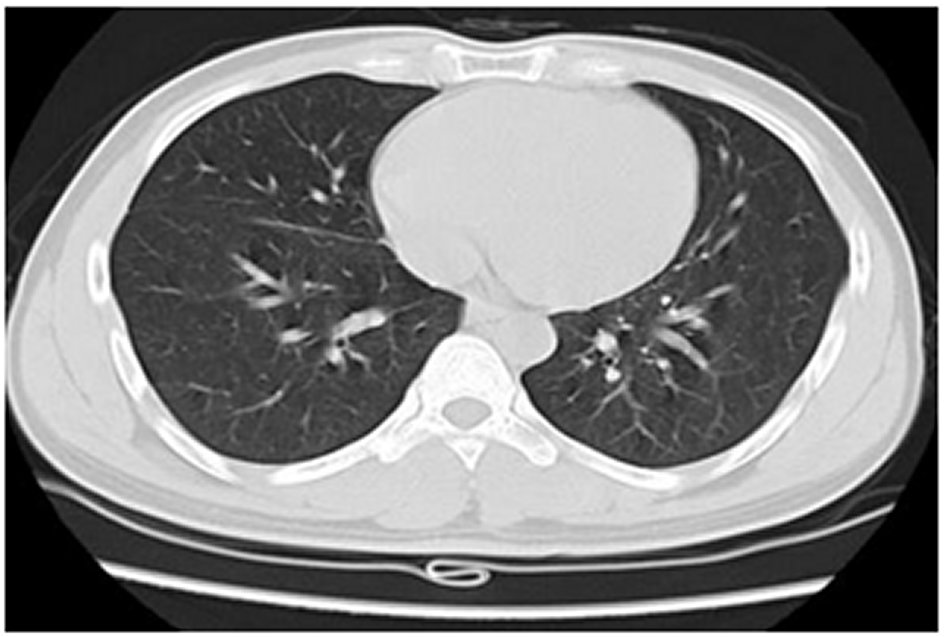
Examination revealed an averagely built and nourished patient. His body mass index (BMI) was 21.3 kg/m2. He was febrile; other vitals parameters were normal. Oxygen saturation was 97% on room air. General examination and examination of upper respiratory tract was unremarkable. On systemic examination, only positive finding was bibasilar fine crackles. Routine investigations including complete blood count, erythrocyte sedimentation rate (ESR) and urinalysis were normal. Absolute eosinophil count was 100/µL. Chest x-ray postero-anterior (PA) view showed bilateral small nodular opacities (Figure 1). Pulmonary tuberculosis was considered as first differential because of its endemicity in India. Other possibilities of pneumoconiosis, hypersensitivity pneumonia and carcinomatous lymphangiectasis were also kept in mind. Tuberculosis was ruled out by negative Mantoux test, sputum for acid fast bacilli (AFB) and cartridge based nucleic acid amplification test (CBNAAT). Sputum examination for fungal hyphae was also negative. High resolution computed tomography (HRCT) thorax showed diffuse micronodules (predominantly in both upper and right middle lobes), ground glass attenuation and air trapping suggestive of hypersensitivity pneumonitis (Figure 2). Spirometry was suggestive of restrictive abnormality, with reduced forced vital capacity (FVC) (70% of the predicted value) and preserved airflow. There was no improvement in FVC with inhaled bronchodilators. He was finally diagnosed as a case of bagassosis in view of the occupational history, clinical and imaging and spirometry findings. He was managed with corticosteroids, tablet prednisone 0.5 mg/kg/day for four weeks followed by weekly reduction of dose by 05 mg per week over next six weeks and then stopped. Patient showed noticeable improvement with treatment (Figures 3 and 4). On medical advice, he also changed his job. He has been followed up for six months post steroid therapy and remains asymptomatic.
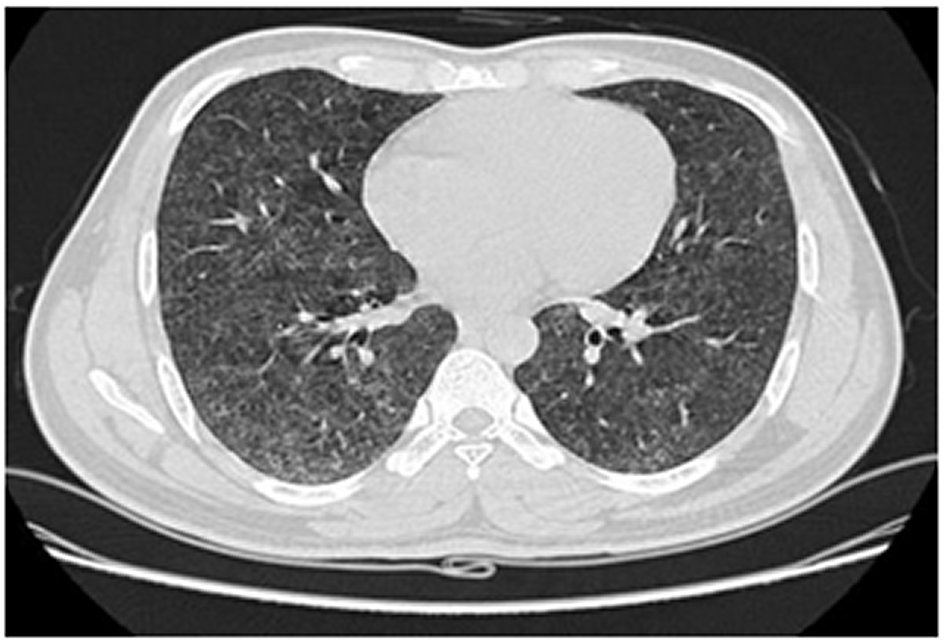
Figure 2. Diffuse ground-glass opacities (GGO) with superimposed intra and interlobular regular nodular septal thickening and a few small areas of air trapping.
DISCUSSION
Bagasse, because of its tough fibrous nature and good insulating properties, is used in the manufacturing of hardboard, acoustic and thermal insulating materials and certain classes of paper and in the production of refractory bricks. First described by Jamison and Hopkin in New Orleans, the incidence, prevalence and age and sex distribution of bagassosis is not known owing to its rather rare occurrence [6]. However, in India, AB Singh and TS Pandit found that 42.5% of sugar refinery workers exposed to bagasse developed respiratory complaints [7]. HP follows a delayed allergic reaction, secondary to repeated and prolonged inhalation of different types of organic dusts of animal or vegetable origin and more rarely chemicals, to which the patient is sensitized and hyper-responsive. A number of substances as avian dust, mould, paint catalyst, sugarcane dust, mushrooms, rat and gerbil urine, tobacco, heating and cooling systems, cork dust, plastic residue, epoxy resin and wheat mould or dust may be responsible for HP such [8]. The workers in environments or settings contaminated by organic dust of various origin, like farmers or animal breeders are most at risk [9]. Repeated exposure to particles sufficiently small in size (diameter < 5 μm) reach the alveoli and trigger an immune response.
A high index of suspicion, a meticulous history covering all relevant environmental and work-related exposure is the keys to the diagnosis of HP. Once history is suggestive of HP, the causal agent need not only to be identified, a temporal association with the alleged substance has to be established. Our patient reported with non-specific respiratory symptoms that could be explained on the basis of respiratory tract infection and/or allergic reaction. His work environment and aggravation of symptoms on work days was a clue to the diagnosis of HP. However, in India, tuberculosis is endemic, it is therefore prudent to consider pulmonary tuberculosis as possibility in all such cases and it's essential to rule it out. In India, tuberculosis may even be co-existing in any patient of chronic lung disease. The diagnosis of bagassosis based on occupational exposure to bagasse in a patient with ILD. The chest x-ray and HRCT merely confirm ILD. The HRCT patterns typical for HP include a centrilobular diffuse micronodular pattern, ground-glass opacification and mosaic attenuation (reflecting coexistent small airways disease) predominantly in upper and middle lobes [10, 11]. Pulmonary function tests show a restrictive picture, including reduced lung volumes, ventilatory capacity and gas transfer. FEV1 and FVC are reduced with normal FEV1/FVC ratio. The spirometry shows the severity of airway restriction and helps in monitoring the response to therapy. Serum specific Immunoglobulins (SsIgGs) against the alleged antigen and/or lymphocytic alveolitis on BAL may help confirm the diagnosis [12]. A lung biopsy should be considered in patients in whom the diagnosis remains uncertain. The physical examination may be completely normal initially. In advanced fibrotic phase, coarse inspiratory rales are usually heard and, in some cases, high-pitched inspiratory wheeze known as “chirping rales” or “inspiratory squeaks” may be present [13].
The first therapeutic intervention should be avoidance of further exposure to the inducing agent. The change of occupation, if possible, is the best way to avoid future exposure. Patients must be warned about the importance of a clean environment and the need to avoid exposure to known HP inducers in future. Currently systemic corticosteroids are the mainstay of pharmacological treatment. Varying doses and duration, starting at 0.5 mg/kg (ideal body weight) for a few days and slow tapering to the lowest possible dose over several months to a year or longer, have been used. The general goal is to maintain the patient at the lowest-possible dose and for shortest duration. The dosage and duration of treatment have not been determined in any study [14]. Alternative drugs have been tried in select cases and include inhaled corticosteroids, bronchodilators, cromolyn sodium, and antihistamines. Low dose macrolide antibiotics have also been tried to reduce inflammation. In patients who cannot tolerate or develop adverse effects of chronic steroid therapy, treatment with azathioprine or mycophenolate mofetil has been tried. Both the drugs were associated with an improvement in gas exchange but there was no significant change in FVC or mortality. The use of immunosuppressive drugs in HP still remains tentative and requires further studies [15].
CONCLUSIONS
Bagassosis is an airborne disease caused by inhalation of the bagasse dust contaminated by thermophilic actinomycetes, most notably Thermoactinomycetes vulgaris. It produces a hypersensitivity reaction characterized by widespread involvement of the distal airways, interstitium and alveoli, resembling that seen in other extrinsic allergic alveolitis. High index of suspicion, meticulous history, thorough clinical examination and systematic diagnostic approach is required for timely diagnosis and management of this potentially reversible, otherwise debilitating condition.