INTRODUCTION
Pesticides (available as organophosphate, organochlorine, aluminium phosphide) poisoning accounts for one-third of the total suicide rate across the globe [1]. Aluminum phosphide (ALP) is available in the form of tablets and powder most commonly in the name of Celphos (56% ALP and 44% Carbamate). ALP is a solid fumigant that liberates lethal phosphine gas in contact with atmospheric air and hydrochloric acid in the stomach. Within minutes of ingestion, toxic features of poisoning may be seen like severe vomiting, resistant hypotension, metabolic acidosis, myocardial suppression, and acute respiratory distress syndrome (ARDS). No specific antidote is available until date so aggressive supportive management is the key to survival in cases of ALP poisoning. A retrospective study of 125 patients in Ethiopia showed high prevalence in females (57.6%) with nausea and vomiting being the common presenting symptom followed by hypotension [2]. A similar study in Iran suggested the mortality rate of ALP poisoning in Iranian population of 27% with good survival rate in younger age patients [3].
We present a case of 24-year-old female with ingestion of 4.5g of ALP managed successfully by our team.
CASE REPORT
A 24-year-old female presented with deliberate ingestion of one and a half tablets of ALP (56%), 3g each mixed with fruit juice 30 minutes before presentation at the emergency department (ED) of our hospital. Her family members denied any history of psychiatric illness or use of any medications. She complained of mild abdominal pain localized around the peri-umbilical region. She had 2 episodes of vomiting prior to the presentation at the hospital that contained recently eaten food particles mixed with water. At ED, she was conscious with a Glasgow Coma Scale (GCS) of 15/15. Her vitals were within the normal limits except her heart rate, which was 120 beats/min. Her oxygen saturation in room air was 94%. Immediate decontamination and gastric lavage with coconut oil were done. Routine investigations were sent which were within the normal limits. The patient was kept nil per oral to prevent any further phosphine gas release. Magnesium sulphate was initiated with a 3g bolus followed by 6g infusion over 12 hours for 5 days. The patient was then admitted to the ICU for further monitoring and treatment with magnesium sulfate infusion and maintenance intravenous fluids.
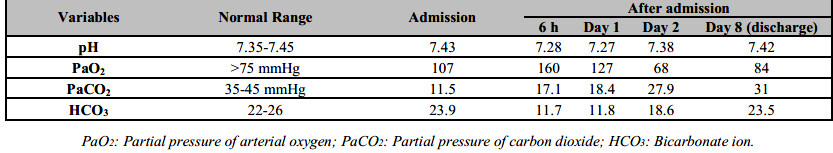
Six hours after the admission to Intensive Care Unit (ICU), the patient developed hypotension (BP=70/50 mmHg). She was resuscitated with one litre of normal saline and the blood pressure after one hour was 80/60 mmHg. Nor-adrenaline drip was started at 0.05mcg/kg/min and increased upto 0.1mcg/kg/min until the blood pressure returned to a normal range. Arterial blood gas (ABG) analysis showed metabolic acidosis (pH: 7.28, PaCO2: 17.1, HCO3: 11.7) for which sodium bicarbonate infusion was given over the next 48 hours until the acidosis was corrected. The ABG was repeated at every 24 hour until the acidosis was normalized (Arterial Blood Gas report from admission to discharge shown in Table 1).
On day 2 of admission to ICU, her serum potassium raised to 6.5 mmol/L. 12 lead ECG was done immediately which showed normal sinus rhythm. She was then treated for hyperkalemia with 10% Calcium gluconate infusion. Her potassium levels and ECG were monitored every 6 hourly and the potassium level normalized after 24 hours.
On day 3 of admission, she developed shortness of breath and oxygen saturation started falling. She was hooked with an oxygen mask at oxygen at 8L/min. Immediate chest X-ray showed left lower zone consolidation (Figure 1A) for which antibiotic and steroid were added. Piperacillin/Tazobactem at 4.5g every 8hourly was continued for 7 days. 200mg of intavenous hydrocortisone was given stat and then 100mg every 8 hourly was continued for 7days. She required oxygen for the next 36 hours and we were able to gradually taper off the oxygen requirement. She was completely stable on day 4 of admission to the ICU and magnesium sulfate infusion was continued for 5 days.

Figure 1. From left to right: Chest X-ray showing left lower zone consolidation (1A), resolved consolidation after treatment (1B).
She was shifted to the medical ward on 6th day. Oral feeding with sips and liquid diet was started on the same day, which was gradually progressed to solid diet. Psychiatric consultation was done on the same day. She tolerated well to the liquid and solid diets and improved symptomatically. Repeat routine investigations were carried out on the 8th day, which was within normal limit. The Chest X-ray showed resolved consolidation (Figure 1B). The patient was discharged on 8th day and advised for follow-up in 7 days. Her follow-up visits were carried out at regular intervals for 1-month along with psychiatric evaluation on each visit.
DISCUSSION
ALP poisoning is the second most common cause of death due to pesticide poisoning after organophosphate. Nepal being an agricultural country, ALP is widely used as an insecticide and means of self-harm. It is more common in adults. ALP is available as a dark-grey 3g-tablet most commonly in the name of Celphos in Nepal. ALP is fatal with a mortality rate of 37% to 100% [4, 5]. The lethal dose of ALP is 1-1.5g and even a dose of 150-500mg have resulted in mortality [5]. ALP causes toxicity due to phosphine gas (PH3) that is colorless and odorless. On exposure to air, it gives a characteristic smell of garlicky or rotten fish due to substituted phosphine and diphosphines. Since phosphine gas is rapidly absorbed by ingestion, inhalation, and mucosal contacts, immediate decontamination is crucial primary management in cases of ALP poisoning [6].
Ingestion of ALP tablets is the commonest mode resulting in ALP poisoning, the other being inhalation and absorption through the mucosa. After the ingestion of ALP tablets, phosphine gas is liberated in the presence of HCL in stomach. This phosphine gas is rapidly absorbed from the gastrointestinal tract and enters the bloodstream causing direct toxicity to organs like the heart, lung, kidney, and liver. Phosphine gas blocks cytochrome C oxidase in the mitochondria leading to disruption of oxygen transport in the electron transport chain causing cell death. It also releases reactive oxygen species (superoxide and hydrogen peroxide) that causes lipid peroxidation and cell death [7]. Some studies suggested the use of Glutathione, Vit C and E, Carotenes, and melatonin helps in reducing the oxidative stress in cases of ALP poisoning and hence better prognosis [8].
The immediate clinical manifestations include nausea, vomiting, abdominal pain, and loose stools. Cardiac manifestations include refractory hypotension and fatal arrhythmias (supraventricular tachycardia, ventricular tachycardia, ventricular fibrillation, atrial flutter/fibrillation). Respiratory features may include dyspnea, cough, cyanosis, respiratory failure, and ARDS [9]. In our case, the patient developed pneumonia 2 days after admission, which is most probably hospital, acquired pneumonia for which piperacillin/tazobactem was given for 7 days [10]. Other infrequent findings include hepatitis, methemoglobinemia, acute tubular necrosis, and disseminated intravascular coagulation (DIC). The diagnosis is mainly clinical with positive history of ALP tablets ingestion, garlic odor at presentation, and symptoms suggestive of ALP ingestion. However, silver nitrate test on gastric aspirate and gas chromatography with a nitrogen-phosphorus detector can be done for diagnosis in case of doubt [7, 8].
There is no specific antidote available for ALP poisoning. Therefore, the treatment is mainly supportive which includes immediate decontamination, prompt diagnosis, gastric lavage, hemodynamic stabilization, early use of intravenous magnesium sulfate, and intensive monitoring. Gastric lavage with potassium permanganate (1:10000) and coconut oil should be started immediately after the diagnosis of ALP poisoning. Potassium permanganate oxidizes phosphine to a non-toxic phosphate and coconut oil prevents the absorption of phosphine gas by forming a protective layer around gastric mucosa [9]. Sorbitol and proton pump inhibitors has been used with a good effect as shown in few studies. Metabolic acidosis results from accumulation of lactic acid. Mild to moderate acidosis can be treated with intravenous sodium bicarbonate. For severe acidosis and acute renal failure, immediate dialysis may be needed [9, 10, 11]. Myocardial injury leading to hemodynamic instability and refractory is one of the cardinal features of ALP poisoning. Adequate intravenous fluids and vasopressors (Norepinephrine and Dobutamine) should be used to restore the hemodynamic status [10].
The use of intravenous magnesium sulfate has shown to reduce the mortality up to 50% in many studies [11]. Magnesium sulfate acts by stabilizing the cell membrane and hence reducing the incidence of fatal arrhythmias. Another role of magnesium sulfate is to decrease the free radical injury due to its anti-peroxidant effect. Different studies have concluded different doses of intravenous magnesium sulfate. We managed the patient with 3g bolus followed by 6g infusion over the next 12 h for 5 days [2].
Cardiac arrhythmias and hyperglycemia at the time of presentation, severe metabolic acidosis, respiratory failure, shock, lack of vomiting after ingestion, time lapsed after ingestion, and requirement of mechanical ventilation are some poor prognostic factors in case of ALP poisoning [12, 13].
CONCLUSIONS
The recovery of a patient with ALP poisoning is extremely rare especially in developing countries like Nepal. With early presentation to the hospital and aggressive supportive management, recovery is possible. This is a rare case where both mother and child were successfully managed at our hospital. In our case, both mother and child survived because of early presentation, mixing ALP tablets with fruit juice (hence decreasing the potency), early and aggressive supportive management, and early use of intravenous magnesium sulphate. The government should take a keen interest on legalizing the handling of this kind of lethal pesticide whose fatality rate is high.