INTRODUCTION
Situs inversus totalis (SIT) is a congenital pathology, characterized by the disposition of the thoraco-abdominal organs contrary to the usual, acquiring a “mirror image”. Its prevalence is estimated at 1 in 10,000 live births with no predilection for sex (1). It presents a predominantly autosomal recessive pattern, but an autosomal dominant and X-linked pattern has also been described, although less prevalent (2). It is believed to occur due to a dysregulation of the Sonic Hedgehog (Shh) protein during the third week of embryonic development, which is responsible for the expression of the determining factors of the right-left axis (3).
Most of these patients are unknown unless they have symptoms. SIT can be associated with other congenital pathologies such as pancreatic fibrosis, renal dysplasia, biliary atrophy, and congenital heart disease (4). The coexistence of SIT and Abdominal Aortic Aneurysm (AAA) is extremely rare, and its prevalence is unknown (5,6).
Currently, there is no consensus on which is the optimal therapeutic approach in AAA with SIT, however, good results have been described using the transabdominal, right retroperitoneal and endovascular approaches (6-8).
The objective of this publication is to comment on this peculiar association (SIT + AAA) and its possible implications when surgery on AAA is indicated. By last, patient has agreed to allow the authors to publish their case details and images. He has consented the publication of his case details and images
CASE REPORT
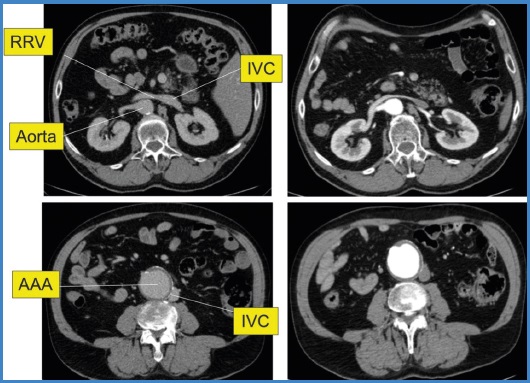
We report a case of a 58-year-old male patient followed-up by our vascular surgery department due to an infrarenal AAA with a transverse diameter of 42 mm, with growth of up to 56 mm (Fig. 1). As a history of interest, the patient has hypertension, diabetes mellitus, atrial fibrillation, Crohn's disease, and SIT.
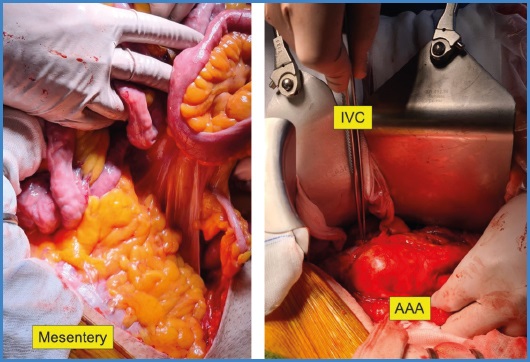
Under general anesthesia, the AAA was excluded, and the aortic continuity was replaced by inserting an aorto-biliac Dacron prosthesis. The surgical procedure was performed through a transabdominal approach from the right side of the patient, with intestinal scrolling towards the left abdomen, unlike usual, due to the anatomical disposition of the root of the mesentery (Fig. 2).
The surgery and the postoperative period occurred without complications and the patient was discharged on the sixth postoperative day. After 30 days, the patient has no incidents in the first review. Currently 3 months have passed since the intervention.
DISCUSSION
SIT is a rare condition that tends to go unnoticed unless patients present symptoms or are discovered during an imaging test or some surgical act (9).
It's presence may increase the surgical risk either due to associated congenital anomalies or due to anatomical changes derived from the reverse arrangement of the thoraco-abdominal organs (3). The association of SIT with AAA is rare and its prevalence is unknown (3).
There are 11 published cases of AAA in patients with SIT in the literature between the first case in 1989 and the present publication (3-13) (Table I).
Table I. AAA associated with situs inversus totalis (SIT). Literature review.
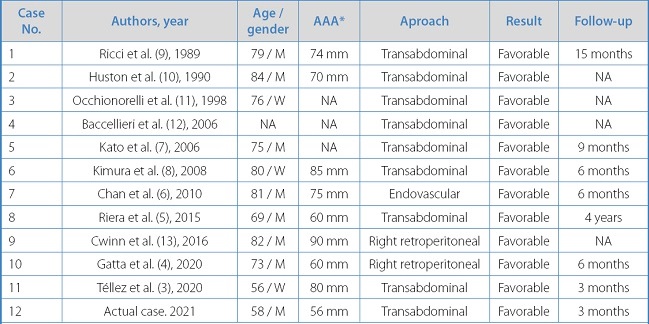
AAA: abdominal aortic aneurysm; SIT: situs inversus totalis; NA: not available;
*Transversal diameter.
The reported cases, like ours, did not present any added difficulty during the surgical act. These have been performed using different types of approaches such as the transabdominal, right retroperitoneal, and endovascular approach (4-6).
The first case reported, in 1989 by Ricci cols. was a 79-year-old male patient who underwent an infrarenal AAA surgery using a transabdominal approach and placement of a Dacron prosthesis. The surgery proceeded without complications and the patient had a postoperative fever that resolved adequately (9).
Kato et al. reported in 2006 a 75-year-old patient with ruptured AAA and SIT who underwent urgent intervention through a transabdominal approach with a bifurcated aortic prosthesis that was performed without incident, the presence of SIT not being a problem for the procedure (7).
On the other hand, Riera et al. in 2015, intervened in a 69-year-old man with an intact AAA and SIT, using a transabdominal approach with a mini-median laparotomy from the right side of the patient with intestinal sliding to the left side and placement of aorto-iliac Dacron prosthesis. The patient recovered without complications and without incidents in the 4-year follow-up (5).
Recently, in 2020, Gatta et al. have performed a right retroperitoneal approach in a 73-year-old patient with a pararenal AAA. Aorto-aortic Dacron graft and exclusion was performed. The patient was discharged on the sixth postoperative day and there were no incidences in CT follow-up after 6 months (4).
In 2010, Chan et al. performed the first published AAA in a patient with SIT using an endovascular approach in an 81-year-old patient. Due to the history of ischemic heart disease and open colectomy, the decision was made to exclude the AAA using an endovascular approach. The procedure was carried out without incident and the patient was discharged on the third postoperative day. After six months, the patient showed no complications on the follow-up computed tomography (6).
Although the transabdominal approach is the most frequently practiced (8 cases), there is no consensus on which is the optimal therapeutic approach in these patients. However, despite the different approach methods used in the literature, asymptomatic SIT does not appear to be a major surgical problem during AAA surgery and does not present additional challenges compared to patients with a normal anatomical disposition.