Introduction
Use of mobile applications (or apps) in healthcare has experienced an exponential increase in recent years, with over 350,000 apps being available at the present time1. Many of these apps have numerous advantages for improve patient care. They also enable healthcare providers to access clinical information in real time and they provide patients with the possibility to remotely manage their disease, allowing them to play a more active role in looking after their health2,3.
The apps' most popular features include being able to access health information and resources, communicating with healthcare providers, controlling symptoms and keeping track of patient adherence to their medication, among other clinical data4,5. The term patient-reported outcomes (PROs) refers to health outcomes such as quality of life, functional status, health status, satisfaction, etc. that are reported by patients without being interpreted by a healthcare provider6-8. Thus, PROs allow patients to provide subjective information about their disease or their treatment, taking on a more proactive role and contributing to the promotion of patient-centered medicine6.
Use of apps may increase the efficiency of the process involved in recording and monitoring PROs by bringing down hurdles such as consumption of resources, lack of time and the difficulty to implement a real-time continuous registry9-11. For that reason, the recording of data is one of the features of these apps that contributes the highest added value in following up on chronic patients5,12. These data, which may be recorded automatically or introduced by the patients themselves, may be transformed into valuable information for clinicians, who may use them as valuable decision-making tools, improving the quality of care afforded to patients without the latter having to travel to their health center. Chronic conditions such as diabetes, Parkinson's disease, cardiovascular disease and cancer, which require continuous monitoring by healthcare providers, can especially benefit from this kinds of tools11,13,14.
Apps have shown that they can lead to improved health outcomes in patients with the above mentioned conditions. Such improvements may range from greater satisfaction levels to a decrease in the number of complications or even fewer hospital admissions. A case in point is that of the e-Oncosalud app, aimed at patients on treatment with oral antineoplastics, which has been shown to reduce drug-related problems (DRPs), increase adherence to treatment, enhance health-related quality of life and reduce the consumption of resources in these patients15. Nonetheless, the apps that allow recording and monitoring of PROs are in the minority, which means that there is Little evidence on the ability of patient-targeted apps to improve their health outcomes4,5,13,16.
The purpose of this study was to carry out a review of the available evidence on the role of mobile apps in PRO registration and on the impact that using such apps may have on health outcomes.
Methods
A literature search was conducted for studies on apps aimed at recording PROs, which also analyzed the impact of the app itself on patient-related outcomes.
The search was carried out in the course of April 2021 in Medline (through Pubmed) and Embase. The search terms used were “app”, “mobile applications”, “patient reported outcomes”, “outcome assessment, health care” and “quality of Life.” The search was performed for all fields, adapting each of them to the standard database search systems. No date restrictions were applied to maximize the number of publications identified.
To be included, articles had to be published in English or in Spanish, with no time restrictions, and had to dwell on apps used by patients, family members and/or caregivers that measured some kind of PRO, such as adherence, quality of life or other health endpoints. Articles analyzing telemedicine-based interventions other than apps were excluded, as were systematic reviews, editorials, PhD dissertations and opinion pieces.
An analysis was made of the titles and abstracts of the articles obtained. Articles that met the selection criteria were downloaded and subjected to a full-text review. A second author reviewed the articles where doubts arose regarding the selection process. The variables analyzed in each article were as follows: author(s) of the article, publication year, studied population, sample size, health outcomes measured, health outcomes obtained, and whether a pharmacist participated in the study.
Results
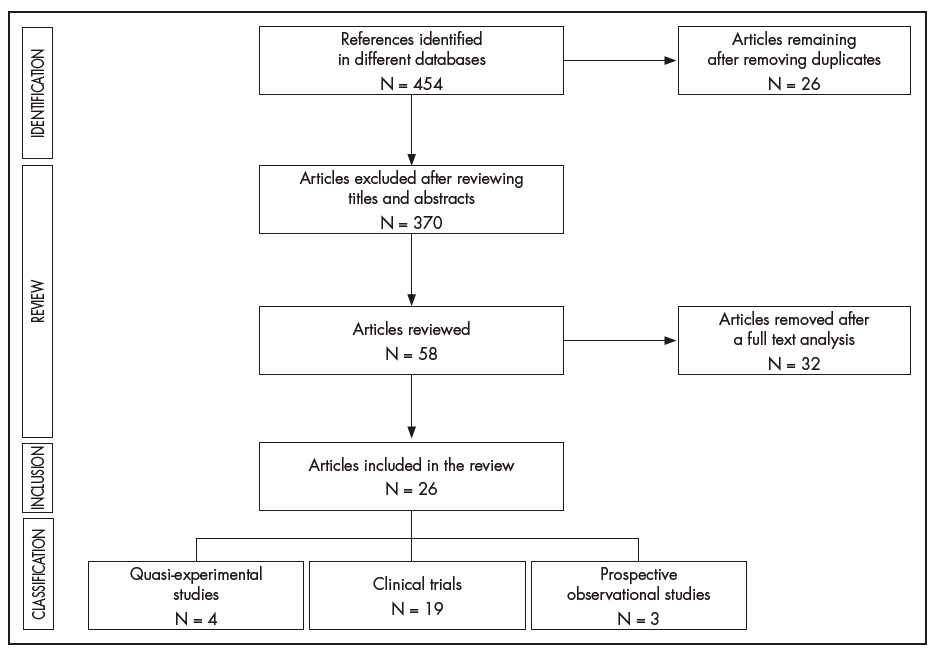
The literature review yielded a total of 454 references. Once duplicates were removed, a total of 370 were excluded for not meeting the established inclusion criteria. At the end of the selection process, the 58 remaining articles that met the inclusion were subjected to a full text review. Finally, 26 of the review articles were included. Figure 1 provides a detail of the selection process.
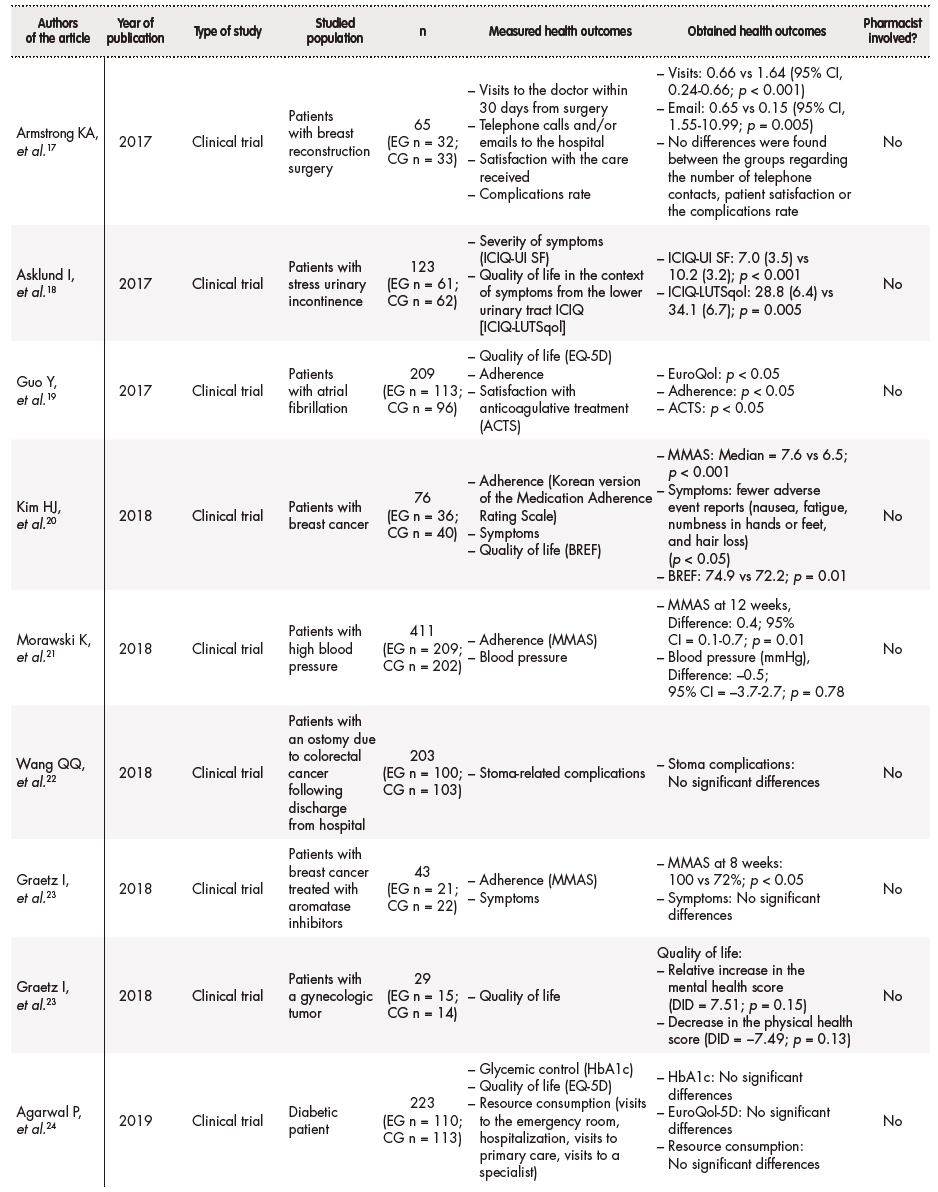
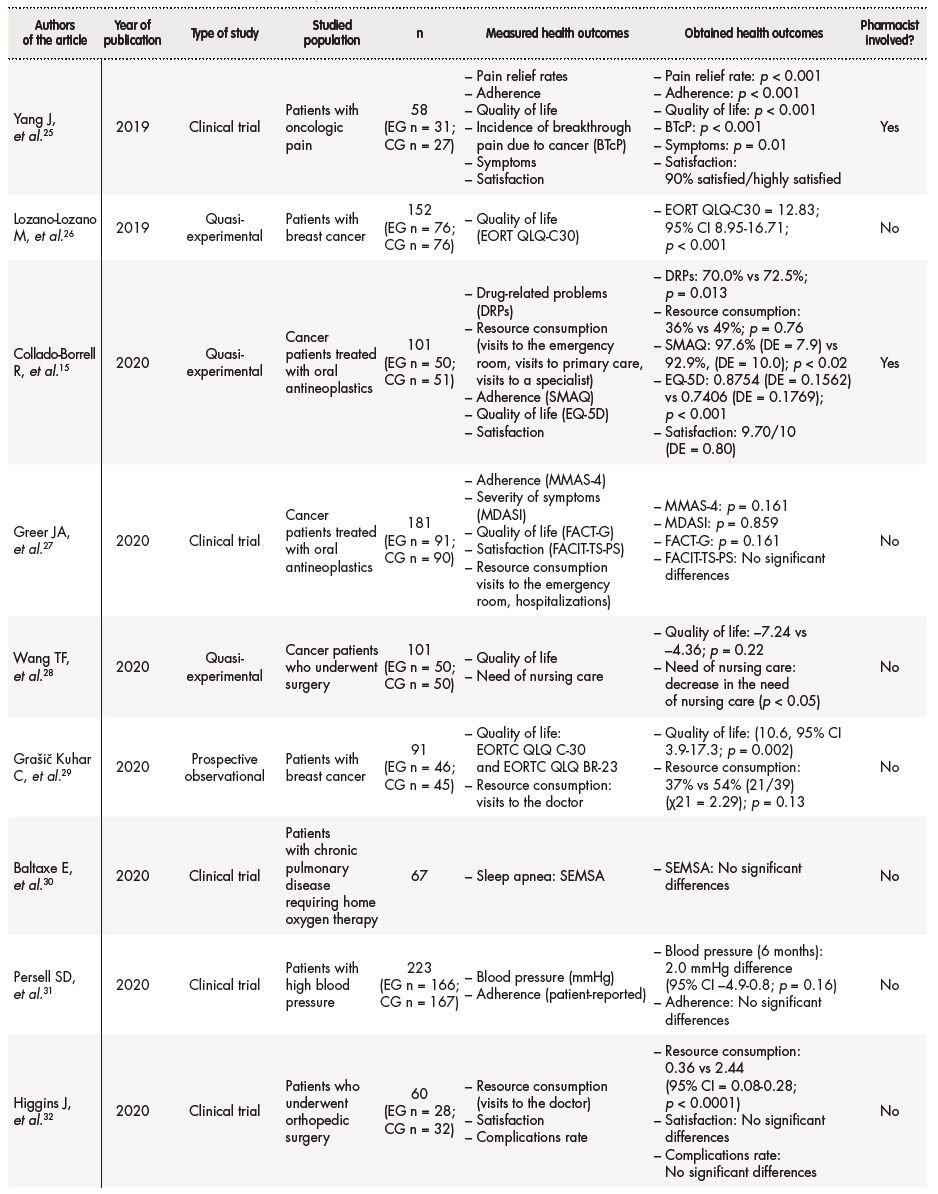
Of the 26 articles reviewed, 19 (73.1%) were clinical trials, 4 (15.4%) were quasi-experimental studies, and 3 (11.5%) were observational studies. Two of the clinical trials were pilot studies. The selected articles were all published between 2017 and 2021, with 50% of them corresponding to 2020. A pharmacy department was involved in 4 studies (15.4%) and 3 of the studies (11.5%) has been carried out in Spain. Table 1 summarizes the characteristics of the studies analyzed17-40.
Table 1 (cont.). Summary of the characteristics of the studies analyzed
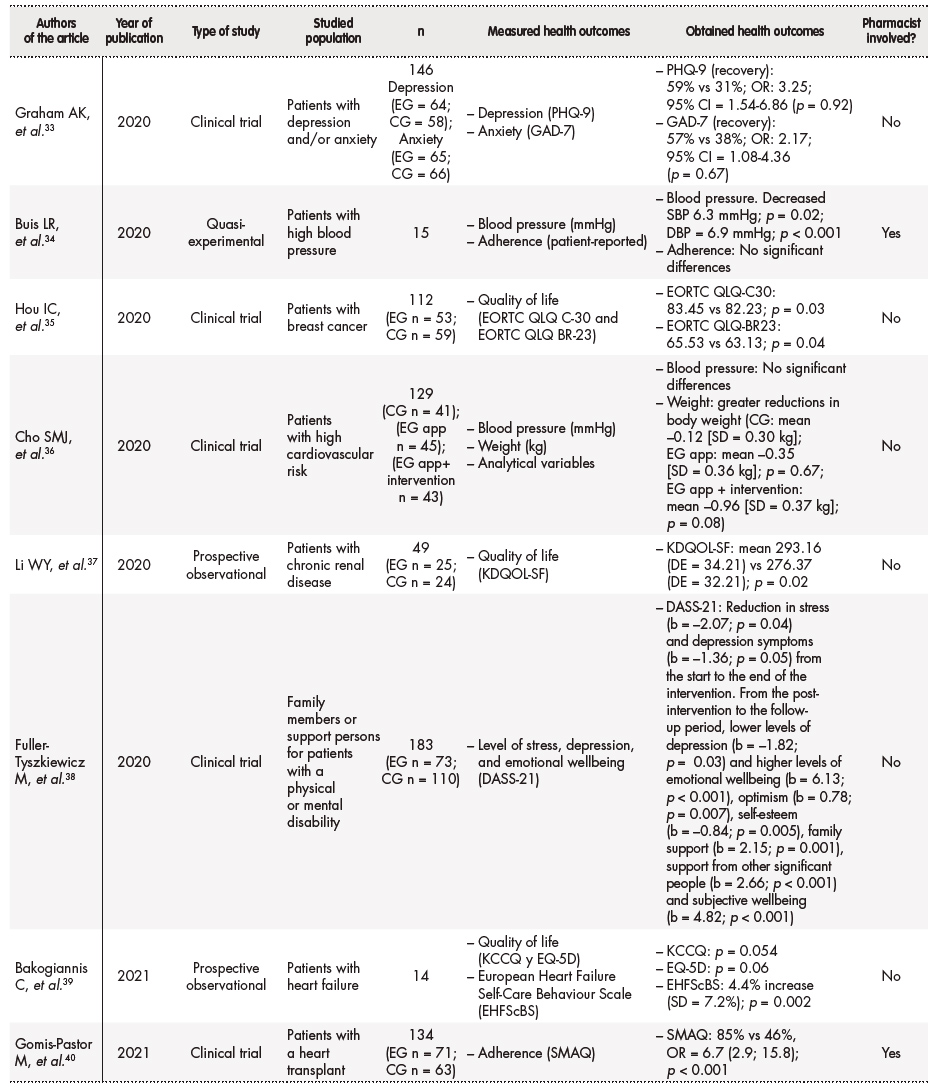
ACTS: Anti-Clot Treatment Scale; DASS-21: Depression Anxiety Stress Scale-21; DBP: diastolic blood pressure; EHFScBS: European Heart Failure Self-care Behaviour Scale; EORTC QLQ: European Organization for Research and Treatment quality of life tool; EQ-5D: European Quality of Life-5 Dimensions; FACIT-TS-PS: Treatment–Treatment Satisfaction– Patient Satisfaction; FACT-G: Functional Assessment of Cancer Therapy–General; GAD-7: Generalized Anxiety Disorder 7-item Scale; CG: control group; EG: experimental group; ICIQ-UI SF: International consultation on incontinence questionnaire – Urinary incontinence short form; KCCQ: Kansas City Cardiomyopathy Questionnaire; KDQOL-SF: Kidney Disease Quality of Life survey; MDASI: MD Anderson Symptom Inventory; MMAS: Morisky Medication Adherence Scale; PHQ-9: 9-Item Patient Health Questionnaire; SBP: systolic blood pressure; SEMSA: Self Efficacy in Sleep Apnea; SMAQ: Simplified Medication Adherence Questionnaire.
The sample size of the studies ranged between 14 and 411 subjects. As regards the types of patients analyzed, most of the articles included cancer patients (11 [42.3%] studies) and patients with cardiovascular conditions [7 (26.9%) studies].
Most studies focused on measuring the impact of the apps analyzed on quality of life (50%), control of clinical parameters (46.2%), adherence (38.5%) and management of symptoms and reduction of complications (26.9%). The remaining studies analyzed the impact of the studied apps on the consumption of resources and on the patients' satisfaction with the level of care received.
Overall efficacy in terms of the percentage of patients where a significant improvement was observed following the use of an app was 73.1%. In spite of that, results were rather heterogeneous across the different interventions analyzed. The PROs where the use of an app was found to have the greatest impact were adherence, health-related quality of life and satisfaction.
Adherence
Adherence was measured by means of validated questionnaires in 8 of the 10 studies where it was analyzed, with the Morisky Medication Adherence Scale (MMAS) and the Simplified Medication Adherence Questionnaire (SMAQ) being the most commonly used ones. Two studies measured this PRO through patient-reported values. Seven (70%) studies observed a statistically significant improvement in adherence when an app was used. In the mAFA pilot study on patients with atrial fibrillation (n = 209), it was found that use of an app significantly improved the patients' understanding, health-related quality of life and adherence to medication (p < 0.05)19. In another study, where subjects had received a heart transplant (n = 134; experimental group [EG] n = 71; control group [CG] n = 63), the strategy based on an app significantly improved adherence to medication as measured by the SMAQ questionnaire (85% vs 46%, OR = 6.7 [2.9; 15.8], p < 0.001)40. Morawskiet al., who studied patients with poorly controlled hypertension (n = 411), found that subjects using an app experienced a small improvement in their adherence to medication at 12 weeks according to the MMAS scale (difference = 0.4; 95% CI [0.1-0.7]; p = 0.1)21.
Health-related quality of life
Of the 13 studies that analyzed health-related quality of life, 8 (61.5%) found a statistically significant improvement in patients using an app. As regards the tools used to measure quality of life, 4 studies used the EuroQol questionnaire and 3 the European Organization for Research and Treatment quality of life tool (EORTC QLQ). The quality-of-life results obtained were independent of the measuring tool used. In a study on 152 patients with breast cancer (EG n = 76; CG n = 76), Lozano-Lozano et al. demonstrated that an app called BENECA was able to improve the subjects' quality of life (EORTC QLQ-C30 = 1.83, 95% CI 8.95-16.71, p < 0.001)26. This study underscored the importance of using an app based on energy balance and showed that it was possible to improve quality of life of breast cancer survivors by means of appropriate monitoring. Grašič Kuhar et al. observed that use of an app by patients with breast cancer on systemic treatment helped them better cope with their symptoms, which lead to an improvement in their quality of life (10.6; 95% CI 3.9-17.3, p = 0.002). Conversely, no change as observed in the use of healthcare resources (37% vs 54% [21/39] [χ21 = 2.29], p = 0.13)29. Another study, which analyzed 112 patients with breast cancer (EG n = 53; CG n = 59), showed that the app used improved quality of life as measured by the EORTC QLQ-C30 and QLQ-BR23 questionnaires (EORTC QLQ-C30: 83.45 vs 82.23, p = 0.03; EORTC QLQ-BR23: 65.53 vs 63.13, p = 0.04)35.
Control of clinical parameters
This PRO was the one for which the greatest number of studies was found where no statistically significant differences were identified in favor of the (58.3% of studies). Agarwal et al. studied 223 diabetic patients (EG n = 110; CG n = 113) and found no differences between the experimental and the control group in terms of glycemic control as measured by HbA1c levels24. Conversely, a quasi-experimental study by Buis et al. on patients with hypertension (n = 15) demonstrated that a pharmacist-supervised app was able to bring down blood pressure in patients with poorly controlled hypertension (blood pressure [mmHg]: reduction in systolic blood pressure [SBP] = 6.3 mmHg; p = 0.02; diastolic blood pressure [DBP] = 6.9 mmHg, p < 0.001)34. Another study on patients with poorly controlled blood pressure (n = 223 [EG n = 166; CG n = 167]) by Persell et al. compared the impact of using an app together with a monitor in the patients' home with the use of just an app for 6 months and observed that the SBP in subjects on the app + monitor group had was similar to that of patients who only used the app (the difference was –2.0 mm Hg [95% CI –4.9-0.8; p = 0.16)]31. A clinical trial on 129 high cardiovascular risk patients distributed into three arms (CG n = 41); (EG app n = 45); (EG app + clinical intervention; n = 43), showed that although simultaneous recording of diet + exercise together with a training program aimed at improving the patients' lifestyles were unable to reduce SBP, they did prove effective in inducing weight loss and reducing body fat (weight: greater weight loss (CG: mean –0.12 [SD = 0.30 kg]; EG app: mean –0.35 [SD = 0.36 kg], p = 0.67; EG app + clinical intervention: mean –0.96 [SD = 0.37 kg]; p = 0.08)26.
Symptomatic control
The ability to control symptoms and/or complications by means of an app was analyzed in 7 studies. Three of these (42.9%) found statistically significant differences in favor of the app. A clinical trial that included 123 patients with stress urinary incontinence observed that, in the experimental group, the app was able to reduce the severity of symptoms as measured on the International consultation on incontinence questionnaire – Urinary incontinence short form (ICIQ-UI SF) questionnaire and induced significant clinical improvements18. However, Wang et al. observed that following up patients with an ostomy due to colorectal cancer after hospital discharge (n = 203 [GI n = 100; GC n = 103]) did not result in a significant improvement in the complications related to the stoma22. Baltaxe et al. were not able to demonstrate that an app can improve patient self-management as measured by the Self Efficacy in Sleep Apnea (SEMSA) questionnaire. However, the wide acceptance enjoyed by this app could be indicative of its potential to improve communication between the parties involved30.
Resource consumption
In the studies analyzed, resource consumption was taken to encompass the different activities and services aimed at meeting patients' care needs (visits to the emergency room, primary care, specialized care, hospitalization) and at ensuring patient-healthcare provider communication (telephone calls, e-mails, etc.). Fifty percent of the studies found statistically significant differences in favor of the apps. The first clinical trial conducted to analyze the impact of an app on resource consumption by patients who had undergone breast reconstruction surgery (n = 65; [EG n = 32; CG n = 33]) found that both visits and email contacts with healthcare providers during the first 30 days after surgery were less frequent in patients using the app (visits: 0.66 vs 1.64 [95% CI, 0.24-0.66; p < 0.001]; email: 0.65 vs 0.15 [95% CI, 1.55-10.99; p = 0.005]). On the other hand, no differences were observed between the groups regarding the number of telephone contacts, patient satisfaction or the complications rate. This data shows that, although patient follow-up through an app does not affect the complications rate, it does improve patient-reported convenience scores17. In a quasi-experimental study on cancer patients undergoing surgery (n = 101 [GI n = 50; GC n = 50]), Wang et al. observed that interventions based on an app significantly reduced the patients' nursing needs, apart from improving their quality of life. The study suggests that apps should be incorporated into the routine care of patients with head and neck cancer to increase the information available to them and to improve their self-management skills28. Similarly, Higgins et al. demonstrated that following up patients through an app may significantly reduce the number of face-to-face visits during the first 6 weeks post-op in patients undergoing anterior cruciate ligament reconstruction surgery, resulting in considerable savings both for the patient and for the system (resource consumption: 0.36 vs 2.44 [95% CI = 0.08-0.28; p < 0.0001])32.
Discussion
This is the first review published to date dedicated to evaluating whether apps that collect PROs are able to improve patients' health outcomes. Oncology is the area that has seen the greatest development of health apps. A total of 42.3% of the articles analyzed investigated the impact of apps on the health of cancer patients, as compared with 26.9% for cardiology patients and 7.7% for surgical or psychiatric patients among others.
A total of 73.1% of the studies reviewed reported that the use of apps resulted in a statistically significant improvement in the evaluated health outcomes. In spite of the limited sample size in some studies, the fact that the majority were randomized clinical trials endows them with a measure of robustness. The most promising findings in the present review were the improvements in health-related quality of life, satisfaction with the care received and adherence to treatment, which was the PRO where apps had the most positive impact.
The review showed that up to 70% of the studies analyzing the potential of apps to improve adherence show a positive effect, adherence rates reaching 100% in some patients15,19-21,23,25,40. Eight of these articles were clinical trials and two quasi-experimental studies. All of them but one measured other PROs apart from adherence, with Gomis-Pastor et al. being the only study whose main goal was to improve adherence through the use of an app. The authors concluded that an app-based strategy can significantly improve adherence as well as the patients' beliefs regarding their medication40. The improved adherence observed in cardiology patients was shown to reduce the number symptoms not only in those patients but also in others23. In fact, 42.9% of studies analyzing the impact of apps on symptom control showed a statistically significant improvement, with similar results across the different studies in terms of symptom management18,20,25. This could mean that apps that collect PROs may play an important role in patient safety, ensuring continuity of care and promoting proper PRO management. According to a clinical trial on patients with breast cancer, which analyzed the impact of an app on the reduction of adverse events and on the improvement of the patients' psychological status, the use of a health app was associated with a lower number of adverse events such as nausea, fatigue, hand foot syndrome and hair loss. Although no statistically significant differences were found in most cases, the incidence of grade 3 fatigue was significantly lower in patients who used the app20.
The collection of PROs and an appropriate management of toxicity have not only been shown to improve patient safety but also to impact their quality of life. For example, Grašič Kuhar et al. observed that use of an app by patients with breast cancer helped them better cope with their symptoms, which resulted in an increased quality of life29. This review showed that quality of life was the most frequently investigated variable, accounting for 50% of all analyzed PROs. This shows the importance given in the literature to quality of life, whose measurement is a way of evaluating the population's health and of analyzing different healthcare interventions41,42. A total of 61.5% of studies showed that quality of life is normally significantly impacted by the use of the app, regardless of the instrument used to measure it15,18,19,25,26,29,35,37. However, Greer et al., which analyzed a sizable patient sample, failed to detect statistically significant differences with respect to the control group. These authors concluded that, although the app could possibly improve health outcomes for all the patients who were prescribed oral antineoplastics, it may be that the intervention is only beneficial for patients with certain risk factors, such as difficulties with adherence or anxiety27. Of the three studies that were only aimed at improving quality of life, Graetz et al. did not report any improvements in the experimental group. It must be noted, nevertheless, that this was a 29-patient strong pilot study23. The other two studies, one of them observational (Lozano-Lozano)26 and the other quasi-experimental (Li et al.)37, did show statistically significant quality of life differences in favor of the app analyzed.
With respect to resource consumption, the majority of studies focused on analyzing the impact of this variable on cancer and surgical patients, half of them showing statistically significant differences in favor of the app analyzed17,28,32. Most of these studies were on surgical patients and showed that follow-up based on an app may reduce the number of hospital visits and the patients' need of nursing care after surgery. It must be noted, however, that none of these studies was designed to analyze the impact of apps on patients' care needs or on the level of patient/healthcare provider communication. Further studies are needed to shed more light on these issues.
Finally, four studies recruited the active participation of a pharmacist in the implementation of the apps and the follow-up of the patients15,25,34,40. All of them revealed statistically significant differences in favor of the apps analyzed. Although the number of pharmacists involved was low, the fact that they were recruited at all is indicative of the important role that pharmacists may play in these technologies. As healthcare providers accustomed to using and validating the new technologies applied to drug administration and patient safety, pharmacists should be regarded as key players in the development of technological initiatives aimed at humanizing care and ensuring the appropriate use of medication.
One of the limitations of this study was the fact that the title- and abstract-based selection of articles was made by a single author. However, to reduce the possibility of bias, a second author was asked to conduct a full text review in cases any doubt emerged in connection with the articles. Furthermore, the possibility exists that an important study for the analysis may have been left out. It must be said, however, that a specific search strategy was designed to identify as many articles as possible.
There is emerging evidence that apps have a positive impact on patients' health outcomes. Use of these tools is making it possible to enhance the management of certain conditions and to achieve outcomes associated with fewer complications, less consumption of resources, improved adherence and better quality of life. These findings should prompt the development of a new self-management model able to promote a healthier lifestyle among patients. Further research is required to determine the applications and limitations of these findings and evaluate the factors that may contribute to improving the outcomes obtained.











 texto em
texto em