Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
Enfermería Global
versão On-line ISSN 1695-6141
Enferm. glob. vol.22 no.70 Murcia Abr. 2023 Epub 26-Jun-2023
https://dx.doi.org/10.6018/eglobal.537541
Originals
Perception of patient safety in surgical room and operating ward compared to other wards in a second-level spanish hospital
1Servicio de Cirugía Ortopédica y Traumatología, Hospital de Sagunto. Sagunto. Valencia. España
2Unidad de Cuidados Intensivos, Hospital de Sagunto. Sagunto. Valencia. España
Introduction:
Patient safety is a basic pillar of healthcare. The surgical patient seems to have singularities compared to other hospitalized patients.
Objectives:
Give the HSOPS questionnaire to the health personnel of various departments of our hospital and compare the responses of the areas of the surgical block (central operating room and surgical ward) against other health care areas evaluated, to obtain descriptive information on the safety environment in our hospital, the ability to detect problems and the notification of adverse events.
Methods:
Descriptive cross-sectional observational study. Percentages of positive, intermediate, and negative responses to the questions and dimensions of the questionnaire were assessed.
Results:
194 questionnaire answers were collected (38.5% completion), of which 94 (48.5%) were nurses. “Staffing” and “Management Support for Patient Safety” were weaknesses in both blocks. "Perception of security" and "Teamwork between units" were weaknesses only in the surgical block. The "Expectations of safety actions by the head of service/ supervisor", without being a weakness, were lower in the surgical block. Reporting of adverse events by health personnel is very low.
Conclusions:
We must continue working on evaluating the safety culture and reporting adverse events to improve care for our patients.
Keywords: patient safety; adverse events; medical-surgical Nursery
INTRODUCTION
Patient safety is a basic pillar of healthcare that helps to reduce the risk of damage associated with healthcare practice to an acceptable minimum 1. It is a set of individual and organizational behaviors, based on shared beliefs and values, that seeks to reduce the harm that the patient might suffer in relation to the provision of healthcare 2.
In surgical areas, different interventions are performed by a large number of specialties under the pressure of a surgical procedure, which predisposes to mistakes. The surgical patient seems to have singularities with specific complications of this care such as surgical wound infections, deep vein thrombosis or adverse reactions in relation to anesthesia 3. The care and approach to the safety of the post-surgical patient should be similar to that of other hospitalized patients. The presence of adverse events is related to human, organizational and health system factors, which should be periodically evaluated. The first step towards a better safety culture is the dialogue about adverse events.
In 2008 the World Alliance for Patient Safety, promoted by the WHO, established its second challenge, "Safe Surgery Saves Lives". Its main objective was the safety of surgical interventions and the reduction of patient morbidity and mortality from an interdisciplinary and teamwork perspective. It established that both, patient safety and the success of an intervention, depends on each member of the team 4.
General patient safety perception assessment questionnaires such as the Hospital Survey on Patient Safety Culture (HSOPS) 5, developed by the U.S. Agency for Healthcare Research and Quality (AHRQ), may help to detect deficiencies in health care and to implement improvement actions. For this reason, we decided to carry out our study, to give this questionnaire to the healthcare personnel of various departments of our hospital, and to compare the responses of the areas of the surgical block (central operating room and surgical hospitalization ward) with those of the other areas evaluated, in order to obtain descriptive information on the safety environment in our hospital, the ability to detect problems and the reporting of adverse events.
MATERIAL AND METHODS
A descriptive cross-sectional observational study was carried out to evaluate the results of a survey to assess the patient's perception of security, and a comparison of the responses obtained in the surgical block (central operating room and surgical ward) with the responses from other hospital wards was made. A questionnaire was sent electronically and answered anonymously by nurses, healthcare assistants, porters, hospital cleaners and physicians from several departments (medical, surgical, operating rooms, pediatrics, maternity, oncology and intensive care unit -ICU-) of a second-level Spanish hospital at 2 times when the hospital care pressure for COVID-19 patients was not excessive during the year 2021. A favorable opinion was obtained from the Clinical Research and Trials Committee for the development of this study.
The safety assessment was carried out using the HSOPS questionnaire 5, translated into Spanish 6. It is a semi-structured questionnaire with 42 questions grouped into 12 dimensions, and 5 response options on a Likert-type rating scale: favorable responses to the question statement ("totally agree" or "always"), intermediate ("neither agree nor disagree" or "sometimes") and unfavorable responses to the question statement ("totally disagree" or "never"). The relative frequency of positive responses (number of positive responses divided by the sum of positive, negative and intermediate responses) of each question and each dimension was calculated. A dimension was labeled as a strength if it had at least 75% positive responses to questions asked in the positive direction, or 75% negative responses to questions asked in the negative direction. A question or dimension was considered a weakness if it had at least 50% negative responses to questions asked in the positive sense, or 50% positive responses to questions asked in the negative sense. The frequency of negative responses was also evaluated to elucidate the areas where efforts should be focused to improve the safety culture.
The dimensions were:
- Referred to your area of practice: "Non-punitive response to errors" (Dimension 8: D8), "Organizational learning - continuous improvement" (D4), "Overall perceptions of patient safety" (D2), "Staffing" (D9) and "Teamwork within units" (D5).
- Related to communication: "Communication openness" (D6), "Feedback and communication about error" (D7).
- "Supervisor / manager expectations and actions promoting patient safety" (D3).
- "Frequency of events reported" (D1).
- Aspects in your hospital: "Handoffs and transitions" (D12), "Management support for patient safety" (D10) and "Teamwork across units" (D11).
An overall perception of security culture question was included with a numerical score from 1 to 10. And other questions were added about:
- Professional group;
- Socio-occupational characteristics: in what year did they start working in their current occupation; in what year did they start working in their department;
- Frequency of adverse event reported in the last year;
- And finally 8 questions (53 - 60) about common work practices that indicate safety culture: working with verbal orders, making medical history reports, medication changes, diagnostic information, requesting informed consent and assessing treatment preferences in probably terminal patients.
Reliability, the degree to which the questionnaire consistently measures its object of measurement, without errors, in a population sample, was assessed with Cronbach's alpha coefficient.
An overall security perception score was calculated as the sum of the scores of the different questions: the negative response "never" or "strongly disagree" awarded "0 points" and the positive response "always" or "strongly agree" awarded "4 points". The maximum security perception score would be 4 (maximum score) x 42 questions = 168 points.
The sample size obtained led us to assume that the variables are normally distributed. Continuous numerical variables were described with mean and standard deviation (SD). Categorical variables were described as percentages. T-Student t-test was used to compare a continuous numerical variable versus a dichotomous categorical variable. The JI-Squared test was used to assess the relationship between 2 categorical variables. P value below 0.05 was considered statistically significant.
RESULTS
Overall results
A total of 194 questionnaire answers were collected from health care staff, 148 women (76.29%). Regarding the professional groups of the participants, 94 (48.5%) were nurses, 51 (26.29%) healthcare assistants, 45 (23.19%) physicians, 3 (1.55%) porters and 1 (0.51%) hospital cleaner. Overall, 11.86% came from the Medical Ward, 24.74% from the Surgical Ward, 4.08% from the Operating Room, 15.46% from Pediatrics/Maternity, 6.63% from Oncology and 35.05% from the ICU. Although initially the survey was not carried out in the Emergency Department, 4 workers of this service sent their questionnaire. The overall questionnaire completion rate was 38.5% (190/493), with values ranging from 13.33% in the Operating Room to 73.9% in the ICU.
The mean age was 46.11 years (SD 11.59). They worked in their profession 17.11 +/- 11.96 years, 10.70 +/- 10.30 in our hospital, and 6.78 +/- 6.93 years in their current unit, with asymmetrical distributions (medians of 15, 6 and 3 years, respectively). Only 67 (34.5%) had recently received patient safety training.
The score for quality and safety in patient management was 7.84 +/- 1.53 points (median 8), with 3.09% failing, 12.37% passing, 51.55% notable and 32.99% outstanding. These scores were similar across the different departments. The safety grade scores showed differences between occupational groups (p < 0.001), with scores of notable and outstanding in healthcare assistants, porters and hospital cleaners; and other grades ("passing" and aggregate insufficient) of 18.1% and 28.9% in nurses and physicians. There were no differences in the scores of workers with greater o lesser number of worked years, or worked hours per week. The majority of health workers (96.43%) did not report any adverse event.
Cronbach's ALFA index was 0.92; when each question was individually removed from the overall estimation, all estimates of this statistic were greater than 0.910 .
Question 1 "People support one another in this unit" included in D5 "Teamwork within units", had the highest percentage of positive responses (90.72%). Question 31 "Hospital management seems interested in patient safety only after an adverse event happens", included in D10 "Management support for patients safety", had the lowest percentage of positive responses (21.16%). The dimensions D3 "Supervisor / Manager expectations and actions promoting patient safety" and D5 "Teamwork within units" were Strengths (78.76% and 87.56%). The dimensions D1 "Frequency of events reported", D2 "Overall perception of patient safety", D6 "Communication openness", D7 "Feed-back and communication about error" and D11 "Teamwork across units" had between 50 and 64.7% positive responses. Dimensions D9 "Staffing" and D10 "Management support for safety" were Weaknesses (32.25% and 24.7% positive responses).
The dimensions with the most negative responses were D10 "Management support for patient safety," D9 "Staffing," D8 "Nonpunitive response to errors," and D2 "Overall perceptions of patient safety," all of them accounted for more than 50% of the total negative responses.
The quality score obtained as the sum of the responses to the 42 questions yielded a somewhat lower value than that obtained when quality was asked directly; the mean was 101.95 (SD 21.68) -equivalent to scores of 6.07 (SD 1.29)-. This difference may be due to the fact that the questionnaire is applicable in different hospital settings, and does not include more specific items for each service. There was an acceptable linear correlation between the sum of scores and the overall score for the perception of security (R2 = 0.524).
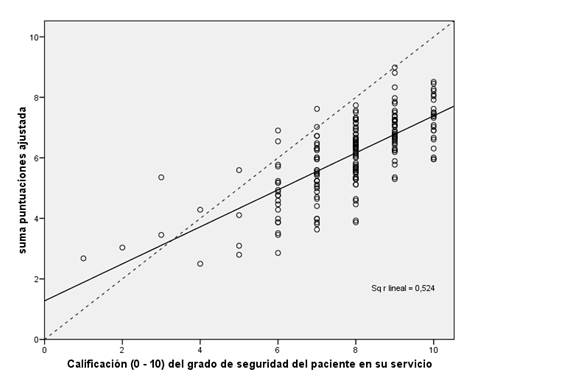
Figure 1: Scatter plot showing the patient safety rating and the sum of scores for the different questions as an estimate of that safety rating. The most of the safety perceptions rated as the sum of question scores is less than the overall perception (points falling below the bisector in the figure).
The last 8 questions had percentages of positive responses above 60%, and even questions 55 "When orders are received verbally about treatments, care or procedures to be performed, the staff receiving them notes them in the clinical document", 56 "Before making a new prescription, the list of medications being taken by the patient is reviewed" and 57 "All medication changes are communicated clearly and promptly to the professionals involved in the patient's care" were Strengths (positive responses > 75%). All questions had less than 20% negative responses.
Results from the sugical block
A total of 56 surveys were collected (48 on the surgical ward and 8 in the operating room), which represented 30.11% of the total number of surveys collected, with a variable completion rate (48% in the surgical ward and 13.33% in the operating room). There was a higher frequency of women (78.6% in surgical block vs 75.4% in the rest, p = ns). The age of the healthcare workers was slightly higher in the surgical block (47.43 ± 11.12 vs 44.98 ± 11.94, p ns). Similarly, the years of profession and years of work in the Sagunto hospital were slightly higher in the surgical block workers than in the rest (20 ± 11.87 vs 15.89 ± 11.84, p = 0.031; and 13.29 ± 11.18 vs 9.59 ± 9.74, p = 0.036). The years of work in the current unit were also somewhat higher in the surgical block (7.91 ±7.79 vs. 6.3 ± 6.50, p = ns). The percentage distributions of the different professional groups were similar in the surgical block and in the rest of the services.
There were no statistically significant differences in age and seniority as a professional, time working in the hospital, or time working in the unit of each between surgical ward and operating room professionals.
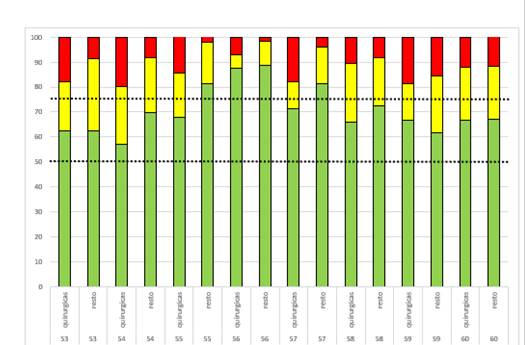
The questions with the highest percentage of negative responses were 15 "Patient safety is never sacrificed to ger more work done" (included in D2 "Overall perception of patient safety") and questions 2 "We have enough staff to handle the workload", 5 "Staff in this unit work longer hours than is best for patient care" and 14 "We work in a “crisis mode” trying to do too much, too quickly" (from D9, "Staffing") (Figure 2). These are all aspects that need to be worked on as a priority within each unit to try to improve the patient safety climate, in a proactive Plan - Do - Check - Act Deming continuous improvement scheme. 7.
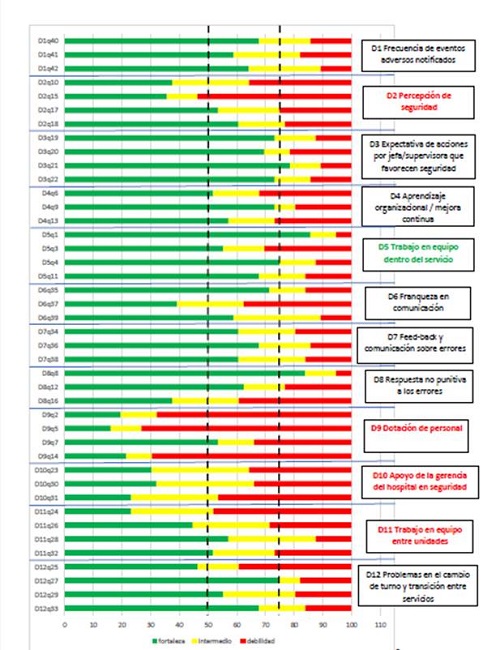
Figure 2: Bar graph showing the positive, intermediate and negative responses to the questions of the different dimensions in the surgical group. Dimensions that are strengths are labeled in green, dimensions with weakness are labeled in red.
Several questions had more than 30% intermediate responses: 39 "Staff are afraid to ask questions about when something does not seem right" (in D6 "Communication openness"), 23 "Hospital management provides a work climate that promotes patient safety", 30 "The actions of hospital management show that patient safety is a top priority" and 31 "Hospital management seems interested in patient safety only after an adverse event happens" (D10 "Management support for patient safety") and 28 "It is often unpleasant to work with staff from other hospital units" (D11 "Teamwork across units ").
The percentages of positive responses in the dimensions of the surgical block and the rest of the units were similar, except in the dimensions related to teamwork (D5 "within units" (p<0.001) and D11 "across units" (p=0.089). The surgical block showed somewhat better scores in “Frequency of events reported” (D1), “Nonpunitive response to errors” (D8), “Management support for patient safety” (D10) and “Handoffs and transitions” (D12), although without significant differences (Table 1).
Table 1: Percentages of positive responses in the different dimensions in the surgical group and in the rest of the services. Dimensions colored in red, Weaknesses. Dimensions colored in green, Strengths. Ns, non-significant difference.
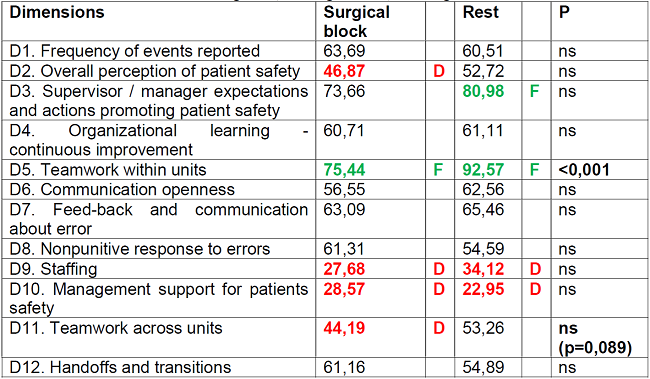
Dimension 5 "Teamwork within units" was a strength in the surgical block and in the rest of the wards, although with a significantly higher value in the rest.
Dimension 3 "Supervisor / manager expectations and actions promoting patient safety” was not a strength in the surgical block (73.66) and was a strength in the rest (80.98).
Dimension 2 "Overall perception of patient safety" was a weakness (46.87) in the surgical block, and was not (52.72%) in the rest. The same was true for dimension 11 "Teamwork across units" (44.19 in the surgical block and 53.26 % in the rest of the units).
Dimensions 9 "Staffing" and 10 "Management support for patient safety" were very marked weaknesses (scores below 35% in the surgical block and in the rest). The perception of "Staffing" was somewhat worse in the surgical block (27.68 vs. 34.12) and the perception of "Management support for patient safety" was worse in the rest (28.57 vs. 22.95) (Figure 3).
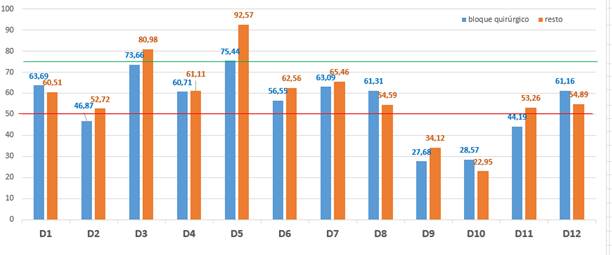
Figure 3: Grouped bar chart of the percentage of positive responses in the different dimensions in the surgical block (blue) and in the rest of the services evaluated (red).
The dimensions with the most negative responses were similar in both scenarios: D9 "Staffing", D10 "Management support for patient safety", D2 "Overall perceptions of patient safety" and D11 " Teamwork across units ".
Comparison of the last 8 questions showed that question 56 was a strength in the surgical block and in the rest of the wards, and 55 and 57 were strengths in the rest. None were weaknesses. No question had more than 30% intermediate responses (Figure 4).
DISCUSSION
The safety of the surgical patient is an issue of vital importance in the field of current medicine, personalized, technified and in pursuit of error. The importance of Nursing, always at the bedside and monitoring the needs of the patient, is enormous. The evaluation of the results of our work draw several significant results.
The group that participated most in our study was Nursery (48.5% of the responses submitted). This is remarkable because, as Alanazi 8 argues, Nursing is a key link in patient safety as it is an important bridge between the patient and other health professionals and plays an important role in promoting safety issues and improving patient outcomes.
The greater length of time previously worked, referring to the surgical block staff, may have influenced the differences in the results found with respect to the other units. The presence of a high turnover with inexperienced staff on temporary contracts may facilitate the presence of errors.
The second dimension "Overall perception of patient safety", with items such as "no more errors happen by chance" or "patient safety is never sacrificed to get more work done", was shown to be a weakness within the surgical block, but not for the rest of surveyed units. We must analyse the internal protocols of the surgical block, looking for points of improvement to optimise the individual perception of safety and internalize the need for patient safety.
A particularly relevant section is the “Frequency of events reported” (D1). Knowing about them allows for the development of resolution and prevention plans and, therefore, is an opportunity to address them prematurely or prevent their occurrence. In our study, 96.4% of respondents reported no adverse events, while in the national study this data is 77.8% 6. In addition, a high percentage of respondents said they feared possible punishment for reporting an adverse event. These data make it impossible to learn from mistakes and make it difficult to improve patient safety because they prevent the creation of adequate prevention plans. Similarly, it should lead us to consider whether there are effective protocols for reporting adverse events and whether healthcare staff are aware of them so that they can use them openly, without fear of being penalised or blamed. Differences between professional groups must be reduced and progressive learning must be facilitated, everybody must understood that error is part of the process, and its communication is the fundamental element for progress. As Pérez Bolaños 9 argues, the goal for the healthcare professional is to feel comfortable working in a team without negative hierarchical conditioning factors and with active communication between them.
The questions with a greater number of intermediate responses were those about "Fear of asking questions about incorrect facts" (within D6 "Communication openness"), 3 questions about the role of hospital management staff in promoting patient safety (D10), and 1 question about “Teamwork across units” (D11). These inconclusive responses were perhaps indicative that scoring clearly negative on these items may have been pejorative or derogatory to the patient safety monitoring system in general.
Aspects such as “Staffing” (D9) and “Management support for patients safety” (D10) were clearly deficient in both groups, surgical and non-surgical (less than 35% positive responses). Despite the obligatory nature of feedback and promotion of patient safety improvement processes in all areas, these data could indicate a higher priority for initiating improvement actions in this block compared to the rest of the departments. The perception that there is a lack of staffing is notable, as the deficit in human resources directly limits the care we can provide to our patients, overloading the entire team and increasing the probability of making a mistake.
Despite the differences between the surgical block and the rest of the hospital, the dimensions on which most of the work should be done to improve the culture or climate of security are the same: improving staffing levels, increasing the involvement of hospital managers in patient security issues (or improving the visibility of their actions in favour of greater security), improving the subjective perception of security and improving teamwork across units.
The results of our study were analogous to those of other research papers conducted in similar settings to ours. Mella et al 10 describe that medical units had a higher number of strengths (D3 and D5) and a lower number of weaknesses (D9 and D10) than surgical units. The hospital areas with the highest number of weaknesses were surgical and ICU, both with the same weaknesses (D9, D10 and D11).
The difference in the questions referring to “Teamwork within units” (D5), with high percentages in the surgical group and other areas to consider it a Strength, but with a difference between them of 20%, was described in other studies (11, 12). Although this is not a weakness, this result should make us think about the quality of teamwork in the operating room, as well as the working environment and support between colleagues, regardless of their care work.
The role of hospital management staff (D10) is extremely important so that the principles of Safety Culture to be translated into action. In the studies reviewed, there are different valuation of this dimension. In the works by Bravo 11 and Pérez Bolaños13 it is shown as a strength. In other studies 6,10,14,15 and in our own, there is a negative perception. Senior health officials need to take tangible actions in favour of quality of care and patient safety, and to promote closer communication between levels, as well as a culture of learning from mistakes.
“Teamwork across units” (D11) was shown as a weakness for operating room staff and not for the rest, with a small difference in percentages. This was a fact that could be evaluated from different points of view. The operating room area is the place in the hospital where a higher percentage of different specialties converge, with their respective actions and protocols, which can lead to greater difficulty in understanding. The group most likely to be affected is Nursing, due to the frequency of rotation between operating rooms of different specialties. The lack of sub-specialization is another handicap. This problem is not only attributable to the organisation of a hospital, but to that of the entire National Health System, employing different workers at this level in different positions depending on the needs of the moment.
Our work had several strengths. Opinions were collected from different key departments within the important care work of our hospital in order to obtain a broad perspective on the security perception of the hospital's staff. The questionnaires were anonymous, which could encourage respondents to express their views truthfully. It also had several limitations. The low completion rate in some areas reduced the representativeness of its results. The questionnaire was distributed at a time of low pressure of care for COVID patients; the dramatic situation experienced previously, in surgical and non-surgical departments, may have influenced the responses obtained.
The future intention of the study is to provide a basis for future actions. According to the cycle of continuous improvement, after the implementation of concrete improvement actions it would be advisable to carry out new measurements of the perception of security culture.
CONCLUSIONS
The safety culture perception is generally acceptable in both surgical and non-surgical settings.
"Staffing" and "Management support for patient safety" were weaknesses in both blocks. "Overall perceptions of patient safety" and " Teamwork across units" were only weaknesses in the surgical block. “Supervisor / manager expectations and actions promoting patient safety", althought not a weakness, were lower in the surgical block.
It is necessary to establish an efficient system for the reporting of adverse events and the continuous evaluation of the safety culture in the hospital environment, understanding them as the basis for the enhancement of the safety culture, without fear to retaliation or belittling by their superiors.
Acknowledgments
The authors would like to thank the healthcare staff (nurses, healthcare assistants, porters, hospital cleaners and physicians) in general for the enormous effort they put into patient care and, in particular, for responding to the questionnaire submitted by the authors.
REFERENCES
1. Rocco C, Garrido A. Seguridad del paciente y cultura de seguridad. Rev Med Clin Condes 2017; 28 (5): 785-95. [ Links ]
2. Dinas Montoya, X. Percepción de la cultura de seguridad del paciente en el personal asistencial y administrativo de una institución de cirugía plástica y estética de Cali en el 2020. Colombia: Universidad del Valle. Web: https://bibliotecadigital.univalle.edu.co/handle/10893/21707 [ Links ]
3. Haugen AS, Sevdalis N, Søfteland E. Impact of the World Health Organization Surgical Safety Checklist on Patient Safety. Anesthesiology. 2019 Aug;131(2):420-425. doi: 10.1097/ALN.0000000000002674. PMID: 31090552. [ Links ]
4. Lara H. Importancia de la Pausa de Seguridad Quirúrgica. Rev. Actuali. Clinic. Meds. Vol. 2. Num 2, Julio - Diciembre (2018). ISSN 0719-8620, pp 40-48. [ Links ]
5. Hospital Survey on Patient Safety Culture, versión 1. Web: Hospital Survey on Patient Safety Culture: User's Guide 2018 (ahrq.gov) [ Links ]
6. Saturno PJ, Da Silva Gama ZA, de Oliveira-Sousa SL, et al. Análisis de la cultura sobre seguridad del paciente en los hospitales del Sistema Nacional de Salud español. Med Clin (Barc). 2008 Dec; 131 Suppl 3: 18-25. [ Links ]
7. Hanghom J. Five Deming principles that help healthcare process improvement. Health Catalyst. 2018. Web: https://www.healthcatalyst.com/insights/5-deming-principles-for-healthcare-process-improvement [ Links ]
8. Alanazi F. K., Sim J.,Lapkin S.(2022). Systematic review: Nurses' safety attitudes and their impact on patient outcomes in acute-care hospitals. Nursing Open 2022; 9, 30-43. DOI: https://doi.org/10.1002/nop2.1063. [ Links ]
9. Pérez Bolaños L. Percepción de enfermería. Una mirada actual a la cultura de seguridad en el quirófano. Investigación en Enfermería: Imagen y Desarrollo. 2020;22 DOI: https://doi.org/10.11144/Javeriana.ie22.pema [ Links ]
10. Mella Laborde M, Gea Velázquez MT, Aranaz Andrés JM, Ramos Forner G, Compañ Rosique AF. Análisis de la cultura de seguridad del paciente en un hospital universitario. Gac Sanit 2020; 34 (5): 500-13. [ Links ]
11. Bravo Gómez M.A., Arboleda de Pérez L.B., Arguello D.K., Becerra Moreno X., Peñaranda Vega M., Oyola Naranjo D.J., Rivera Carvajal R. Cultura de seguridad en profesionales del quirófano en una institución de atención materno infantil. Revista Cubana de enfremería. 2020;36(1):e3155. [ Links ]
12. Carvalho PA, Göttems LBD, Pires MRGM, Oliveira MLC. Cultura de seguridad en el centro quirúrgico de un hospital público, en la percepción de los profesionales de la salud Rev. Latino-Am. Enfermagem nov.-dic. 2015;23(6):1041-8. [ Links ]
13. Pérez Bolaños L. Evaluación de la cultura de seguridad del paciente en un quirófano. Revista Cubana de Enfermería. 2017;33(2):1-13 [ Links ]
14. Viayen A, Hellings J, Claes N, et al. National Hospital Survey on Patient Safety Culture in Belgians hospitals: setting priorities at the launch of a 5-year patient safety plan. BMJ Qual Saf 2012; 21: 760-7. [ Links ]
15. Danielsson M, Nilsen P, Rutberg H, et al. A National Study of Patient Safety Culture in Hospitals in Sweden. J Patient Saf. 2019 Dec; 15(4): 328-333. [ Links ]
Received: September 01, 2022; Accepted: January 13, 2023











 texto em
texto em