Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
REC: Interventional Cardiology
versão On-line ISSN 2604-7276versão impressa ISSN 2604-7306
REC Interv Cardiol ES vol.5 no.1 Madrid Jan./Mar. 2023 Epub 18-Mar-2024
https://dx.doi.org/10.24875/recic.m22000350
CLINICAL CASE
Percutaneous treatment of partial anomalous pulmonary venous connection with dual drainage
aUnidad de Cardiología, Hospital Universitario Reina Sofía, Instituto Maimónides de Investigación Biomédica de Córdoba (IMIBIC), Universidad de Córdoba, Córdoba, España
bUnidad de Radiología, Hospital Universitario Reina Sofía, Instituto Maimónides de Investigación Biomédica de Córdoba (IMIBIC), Universidad de Córdoba, Córdoba, España
SEE RELATED CONTENT:
https://doi.org/10.24875/RECICE.M22000298
https://doi.org/10.24875/RECICE.M22000299
CASE PRESENTATION
Anomalous pulmonary venous connection is a rare condition that occurs when 1 or more pulmonary veins abnormally return to the right atrium or systemic venous circulation. The most common type in adults is drainage of the left upper pulmonary vein (LUPV) into the left innominate vein. Anecdotally, an anomalous LUPV may have dual drainage into the left innominate vein and the left atrium (LA). In the absence of other congenital heart defects, partial anomalous pulmonary venous connection is often an incidental finding and individuals are usually asymptomatic.
In this article, we'll be reporting on a case of dual drainage partial anomalous pulmonary venous connection where the LUPV is both connected to the left innominate vein and the LA in a patient with coronary heart disease and left ventricular systolic dysfunction.
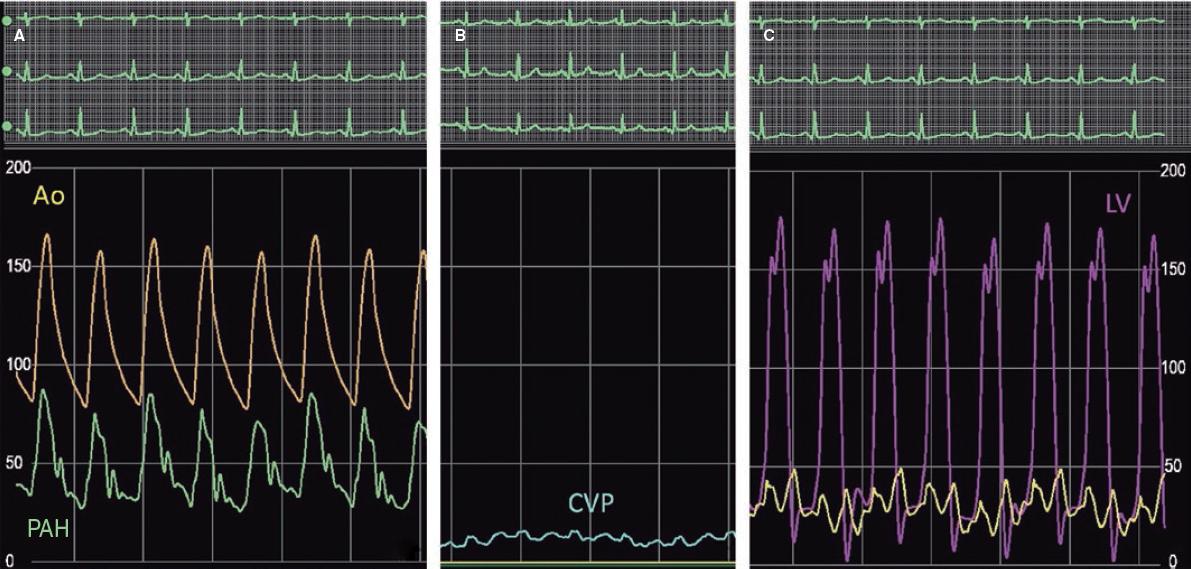
This is the case of 56 year-old man with a past medical history of diabetes and dyslipidemia referred to the cardiac center due to an incidental finding on a thoracic computed tomography scan requested by the pulmonologist as part of a dyspnea diagnostic work-up. At the visit the patient presented with exertional dyspnea with NYHA functional class III and complained of angina on moderate exertion. The physical examination revealed normal auscultation and peripheral edema. The mentioned thoracic computed tomography scan revealed the presence of a LUPV connected to the LA and the left innominate vein trough a vertical vein (VV), as well as pulmonary artery dilation, cardiomegaly, and right pleural effusion (figure 1). Transthoracic echocardiography showed a moderate left ventricular dysfunction (ejection fraction, 35%) with global hypokinesis, LA and right atrium enlargement, right ventricular dilation and dysfunction (a 14 cm tricuspid annular plane systolic excursion) and elevated pulmonary artery systolic pressure (63 mmHg) (video 1 of the supplementary data). Right heart catheterization confirmed the presence of pulmonary hypertension (figure 2). Coronary angiography revealed severe and diffuse 3-vessel coronary artery disease.

Figure 1. Preoperative thoracic computed tomography scan. Multiplanar reformatted (A) and 3D reconstructed (B) images reveal the presence of a left upper pulmonary vein (LUPV) with dual drainage into the left innominate vein through a vertical vein (*) and the left atrium (LA). The vertical vein (*) runs anteriorly to the left pulmonary artery (C). LIV, left innominate vein; RA, right atrium; RSVC, right superior vena cava.
AUTHORS' CONTRIBUTIONS
R. González-Manzanares, and G. Flores-Vergara drafted the manuscript, and completed the critical reviews. S. Ojeda, J. Suárez de Lezo, S. Espejo, and M. Pan reviewed and revised the manuscript and approved its final version before submission. All authors gave their final approval to the version that would eventually be published.











 texto em
texto em