Meu SciELO
Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares em
SciELO
Similares em
SciELO -
 Similares em Google
Similares em Google
Compartilhar
REC: Interventional Cardiology
versão On-line ISSN 2604-7276versão impressa ISSN 2604-7306
REC Interv Cardiol ES vol.5 no.2 Madrid Abr./Jun. 2023 Epub 18-Mar-2024
https://dx.doi.org/10.24875/recic.m22000299
CLINICAL CASE
Intracoronary fibrinolysis as a bailout strategy for massive thrombotic catastrophe
SEE RELATED CONTENT:
https://doi.org/10.24875/RECICE.M22000305
https://doi.org/10.24875/RECICE.M22000306
CASE PRESENTATION
This is the case of a 57-year-old man Canadian immigrant who presented to the emergency department due to chest pain. His past medical history showed hypertension, previous smoking, rheumatoid arthritis, and ischemic heart disease. He had previously undergone percutaneous angioplasty in 2006 in Canada. He had no past family history of heart condition or sudden cardiac death. His usual medication included aspirin, clopidogrel, ramipril, metoprolol, leflunomide, and prednisolone. He complained of constrictive chest pain of 2-hour evolution associated with dizziness. He denied syncope. He was admitted while clinically stable, and pain-free. Physical examination was normal. We performed serial electrocardiograms that appeared normal. Blood work showed elevated troponin I levels (5.23 ng/mL, normal range < 0.05 ng/mL). The remaining blood study was normal. Transthoracic echocardiogram showed good biventricular systolic function with inferior wall hypokinesis. The most likely diagnosis was acute coronary syndrome without ST-segment elevation (typical chest pain accompanied by elevated troponin I levels, and segmental hypokinesis). Other diagnoses like Takotsubo syndrome and myocarditis were less likely.
Due to suspected acute coronary syndrome, he started anticoagulation with weight-adjusted enoxaparin (1 mg/Kg) and loading doses of ticagrelor (180 mg). About 24 hours later, the coronary angiography performed revealed the presence of right dominance (figure 1 and videos 1 and 2 of the supplementary data). A stent was seen at left anterior descending coronary artery level with an acceptable angiographic result up to the distal segment, a location in which a 90% in-stent lesion was found. The right coronary artery had an 80% stenosis in the middle segment, an intermediate in-tent restenosis in the distal segment, and a 90% stenosis proximal to the crux. Additionally, the posterior descending coronary artery had an ostial lesion of 90%. It was decided to proceed with angioplasty (Figure 1, videos 1-4 of the supplementary data) of right coronary artery due to the high thrombotic load reported at this location and de novo segmental wall motion abnormalities. Two protection guidewires were advanced towards the distal portion of the vessels. We subsequently predilated the lesion in the right coronary artery distal segment. Almost immediately after deflating the balloon, we observed an interruption of distal flow. The patient developed chest pain and the electrocardiogram revealed the presence of ST-segment elevation. A stent was quickly implanted into the distal segment without flow improvement. Proximal thrombus propagation continued, and 2 additional stents were implanted. Despite these efforts, the artery remained occluded. Intensive intracoronary aspiration was attempted with 2 different EXPORT systems (Medtronic, Portugal) with removal of large amounts of thrombus. Despite the extraction, the scenario remained the same. Additionally, an attempt was made to dilate various segments of the artery throughout its length. Again, recanalization was unsuccessful. The patient's written informed consent was obtained.
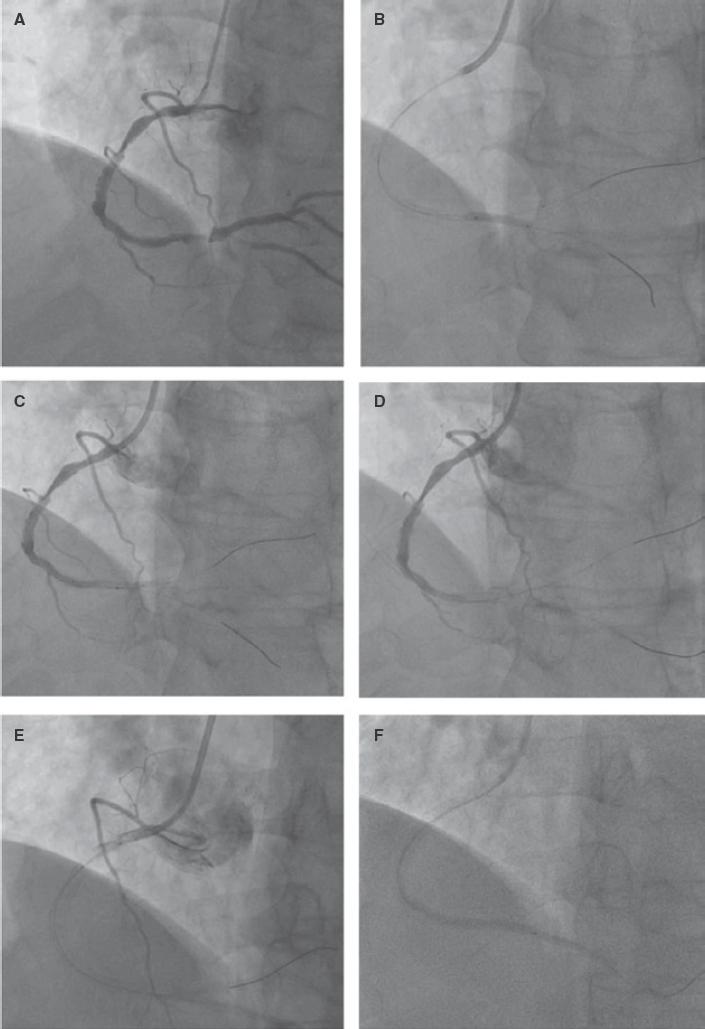
Figure 1. Coronary angiography images. A: dominant right coronary artery showing an 80% stenosis in the middle segment and a 90% stenosis in the segment distal to the crux. Additionally, the posterior left descending coronary artery has an ostial lesion of 90%. B: lesion predilatation on the right coronary artery distal segment. C: no-reflow phenomenon after balloon deflation. D: implantation of a Synergy stent [Everolimus, 2.75 mm x 32 mm] without flow improvement. E: proximal thrombus propagation after implantation of 2 additional Synergy stents [Everolimus, 3.5 mm x 18 mm; 3.5 mm x 12 mm]. F: intracoronary aspiration with 2 different EXPORT systems facilitated the removal of large amounts of thrombus.











 texto em
texto em 


