INTRODUCTION
Older and immunocompromised individuals are at an increased risk for herpes zoster-induced shingles. The initial symptom of the disease is most frequently a unilateral pain or a tingling sensation. Other concurrent symptoms may be fever, malaise, headache and sensitivity to light [1]. One to two days post-symptomatic onset, a blistering rash usually appears in a dermatomal distribution; with the highest prevalence in the thoracolumbar region followed by the facial and sacral areas [2]. These blisters ulcerate then proceed to scab over and become non-infectious [3]. Although often uncomplicated, complications do occur. These may include postherpetic neuralgia occurring in 10-15% of cases, superimposed skin infection in 2% of cases, herpes zoster ophthalmicus in 2% of cases, herpes zoster oticus in 1% of cases, and motor neuropathy and radiculopathy in 4.5-5% of cases [3, 4]. Radiculopathy can affect the sacral nerve roots and cause urinary voiding dysfunctions. Although this complication is relatively infrequent, due to the high incidence of shingles, it is critical to recognize this complication as a possible manifestation. A missed diagnosis of Varicella Zoster Virus (VZV) induced urinary dysfunction may lead to long term complications [5]. In this manuscript, we review a rare case report of zoster-induced urinary dysfunction and aim to aid physicians in recognizing and providing treatment for the condition.
Cases, such as the one presented above, should be studied and added to the growing body of medical literature. In doing so, both patients and physicians can be more knowledgeable which will decrease the diagnosis-to-treatment time.
CASE REPORT
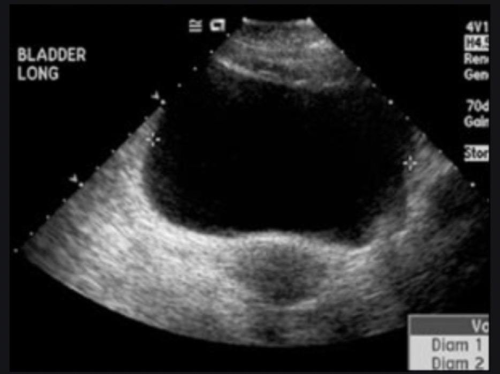
A 42-year-old female presented to the emergency department (ED) with a painful rash on her left buttock and urinary retention for the past two days. She was previously diagnosed with shingles four days before appearing in the ED and was started on a ten-day course of valacyclovir. She had no past medical conditions and was afebrile on the day she was seen. The physical exam was remarkable only for a distended bladder on palpation and an S2-S4 dermatomal vesicular rash (Figure 1) extending onto the vulva and introitus. Tramadol was administered in the ED to relieve the pain. A post void bladder scan revealed a residual volume of 824 ml (Figure 2). A neurology consult was obtained, which recommended MRI of the cervical, thoracic and lumbar spine. These scans were unremarkable as were urinalysis and routine blood tests. A urology consult suggested the likely etiology was bladder areflexia due to shingles. The urologist recommended that the patient be discharged with a Foley catheter and leg bag. The patient refused and requested the removal of the Foley catheter. The patient was able to void successfully as measured by follow up bladder scan indicating 0mL residual volume. The patient was discharged with instructions to return for urinary retention and urologic follow up.
DISCUSSION
VZV-induced bladder dysfunction was first reported by Davidshon in 1890 [6]. Although rare, it is an important complication of Varicella Zoster. A large institutional review found that approximately 4.0% of cases resulted in urinary voiding difficulties with a large percentage increase in urinary dysfunction if the dermatomal distribution was in the sacral region [6]. Other studies indicate a strong positive correlation between zoster-related pain and voiding dysfunction [7]. In addition to a sacral distributed rash and severe pain, other noteworthy associated symptoms which increase suspicion of VZV-induced urinary dysfunction include concurrent constipation, meningitis, or erectile dysfunction [8]. Acute VZV urinary retention is more common in the elderly, but has been reported in all ages including congenitally [9].
Possible etiologies of VZV-induced bladder dysfunction include cystitis-induced dysfunction, neuritis-induced dysfunction and myelitis-associated dysfunction. Cystitis-induced zoster infection occurs due to virion invasion and proliferation within the bladder and presents as hematuria, dysuria, and urinary dysfunction. Myelitis-induced urinary dysfunction typically presents as an overactive bladder. Neuritis-induced bladder dysfunction typically occurs with invasion of lower motor neurons and presents with bladder and detrusor areflexia. Due to the lack of hematuria, negative urinalysis, and lack of history indicating an overactive bladder in the patient, neuritis-induced bladder areflexia is the most likely diagnosis [6].
The condition often resolves without intervention [10]. The time for resolution of urinary symptoms could range from four to eight weeks [6]. Possible complications include an increase in susceptibility to urinary tract infections (UTI) secondary to urinary stasis [11]. Although VZV-induced urinary dysfunction is largely self-limiting, it is important to address and alleviate the immediate symptoms [2]. Urinary-specific alpha blockers such as terazosin or urinary catheterization are quick, cost effective therapies that can significantly improve disease course [2, 12]. These therapies are only needed for short-term management as there typically is no chronic clinical component with regards to urinary involvement [2].
Although the incidence of urinary dysfunction due to detrusor and bladder areflexia secondary to zoster is relatively low, the high prevalence of shingles in the general population yields a large absolute number of cases with significant urinary involvement [13]. It is also well documented that urinary retention increases risk for urinary tract infections and pyelonephritis, which can further complicate the clinical course of the patient. Further, the reported incidence is most likely an underestimation due to the high variability in clinical presentation and lack of clinical awareness; both imaging and urinalysis can come back unremarkable, often leading to an inconclusive diagnosis from those who do not have varicella-induced urinary dysfunction on their differential. This could greatly decrease the time required for treatment of symptoms, unnecessarily prolonging patient harm [11].
Cases, such as the one presented above, should be studied and added to the growing body of medical literature. In doing so, both patients and physicians can be more knowledgeable which will decrease the diagnosis-to-treatment time.