INTRODUCTION
Chronic kidney disease (CKD) is a global public health problem. In countries, such as the United States of America and Australia, it affects 10-13% of the population 1,2. Over the last decade, there has been an increase in the incidence and prevalence of this disease, with a significant increase in the number of patients requiring dialysis therapy 3. Studies conducted in Brazil have shown a gradual increase in the prevalence of CKD, with a high proportion of patients in need of dialysis treatment. In 2016, 122.825 CKD patients were recorded to be on dialysis, and 92.3% of patients were on hemodialysis (HD) 4,5.
Uremia is a serious complication of CKD, and it is associated with renal injury, food restriction, and hydration status. Besides activating the renin-angiotensin-aldosterone system and favoring the occurrence of vascular calcifications, uremia also changes the microbiota (known as dysbiosis) and increases intestinal permeability 6,7,8. It results in an increased flow of urea into the intestinal lumen, which is then hydrolyzed by microbial urease. Bacterial urease catalyzes the hydrolysis of urea to produce ammonium hydroxide; this reaction leads to an increase in the local pH, facilitating the growth of pathogenic bacteria and promoting mucosal irritation and damage 9,10. These changes allow entry of endotoxins and other harmful luminal contents into the underlying tissues and systemic circulation, favoring the manifestation of other diseases 6,7,11,12.
Patients with CKD demonstrate significant quantitative and qualitative changes in intestinal microbiota, related to the overgrowth of aerobic and anaerobic pathogenic bacterial species 7,11. These bacteria can use nitrogen products, thus increasing the production of uremic toxins, such as indoxyl sulfate and p-cresyl sulfate. Such toxins induce inflammation, oxidative stress, and cause a pathophysiological impact, resulting in structural and functional changes that indirectly influence patient morbidity and mortality 13,14.
In uremic patients, oxidative stress and inflammation cause dysregulation of the immune system. This is evidenced by the presence of elevated oxidative biomarkers, such as lipid oxidation and protein oxidation products 15,16. A cross-sectional study involving patients with chronic renal failure demonstrated that the presence of indoxyl sulfate and p-cresyl sulfate was also associated with elevated concentrations of inflammatory markers and increased arterial stiffness, a key clinical finding associated with CKD 17. In the past decade, these toxins have been associated with the progression, cardiovascular morbidity and mortality of CKD patients 18. In addition to uremia and metabolic acidosis, routine therapeutic interventions for treating CKD, such as dietary restriction of fruits, vegetables, and foods with high fiber content, iron intake, phosphate binders, and antibiotics modify the colonic environment. These modifications negatively affect the intestinal microbiota and induce the production of uremic toxins and inflammatory markers 19.
Some interventions are being used to modulate the intestinal microbiota, block LPS or attenuate inflammation, or target adsorption of uremic toxin end products of microbial fermentation 20. Previously published review articles have described some of these interventions: administration of small intestine alpha-glycosidase inhibitor that increases the fermentation of carbohydrates in the colon and can reduce the colonic generation of p-cresol; utilization of essential oils as agents to treat dysbiosis; use of oral adsorbents to restore epithelial tight-junction proteins and reduce plasma endotoxin and markers of oxidative stress and inflammation; administration of synthetic TLR4 antagonists to inhibit LPS signaling; ingestion of prebiotics and/or probiotics that play an important role in the progression of CKD 12,20.
The results of a recent study suggest that the ingestion of prebiotics and probiotics can increase the production of short chain fatty acids, modulating the intestinal microbiota 17. They can also reduce intestinal permeability via blocking the entry of endotoxins into the bloodstream and suppressing inflammation 21; these events are believed to play an important role in the progression of CKD. Therefore, the objective of this study was to systematically review the literature on the effects of intake of prebiotic and/or probiotic products on the intestinal microbiota, oxidative stress, and inflammation in patients with CKD.
METHODS
This systematic review was conducted according to a pre-specified protocol and is described according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses statement 22. This article is based on previously conducted studies, and it does not include studies conducted by any of the authors of this study.
SEARCH STRATEGY
A literature review was conducted in computerized databases MEDLINE (PubMed), Latin American and Caribbean Health Sciences (LILACS), Cochrane Library of Clinical Trials and Science Direct. Databases were searched using the key words: "chronic kidney disease," "hemodialysis," "intestinal permeability," "intestinal/gut microbiota," "inflammation," "oxidative stress," "uremic toxins," "supplementation," "probiotic," "prebiotic," and "symbiotic." These terms were searched alone or in combinations with each other. The search was limited to articles published between 2005 and 2016.
First, a manual search on references of all selected articles was conducted. To ensure that no relevant data was missed, a survey of the gray literature was conducted using the databases of theses and dissertations from the following sources: the Coordination of Improvement of Higher Education Personnel (CAPES), the Digital Library of theses and dissertations of the Federal University of Viçosa, and the Brazilian digital library of theses and dissertations to ensure that no important studies were missed out. Next, the abstracts of these articles were analyzed to verify compliance with the inclusion criteria, and full-text articles were subsequently examined to confirm their eligibility.
SELECTION CRITERIA
In this review, we included randomized clinical studies that examined the efficacy of prebiotic, probiotic, or symbiotic supplementation in modulating intestinal microbiota and regulating nitrogen products and inflammation in CKD patients (both sexes) who had received the intervention for at least one day. Review articles, animal studies, articles not written in English, and those not related to the topic of interest were excluded.
DATA EXTRACTION AND SYNTHESIS
All relevant studies identified in the electronic databases were consolidated in a single database to remove all duplicates. After exclusion of the duplicates, two independent reviewers selected the references in three phases: analyses of titles, abstracts, and full texts. Any disagreements related to conflicting data or study eligibility were resolved by a third reviewer. Data including methodological quality, participant information, duration of intervention, and outcome type (changes in intestinal microbiota, nitrogen products, uremic toxins, total cholesterol, low-density lipoprotein cholesterol, high-density lipoprotein cholesterol, triglycerides, and inflammatory markers) were extracted and collected in duplicates in a Microsoft Excel worksheet. The quality of the included trials was measured using the Cochrane Collaboration's tool for assessing the risk of bias in randomized trials 23. Quality assessment was conducted by three independent reviewers, and disagreements were resolved by consensus.
RESULTS
SEARCH RESULTS
During the initial selection process, 1,679 articles were identified. Later, 781 duplicate articles were excluded, and 890 articles were removed after reading their titles and/or abstracts. Eight other articles were identified by reverse search and were considered as eligible; however, after reading their abstracts, six did not meet the inclusion criteria and were thus excluded from this study. Finally, we included and critically analyzed a total of ten articles (Fig. 1).
According to the Cochrane Collaboration's risk of bias tool for randomized trials, ten selected studies presented varying degrees of bias. All trials had a low or an unclear risk of bias for sequence generation, allocation concealment, blinding, selective outcome reporting, and other sources of bias.
STUDY CHARACTERISTICS
The selected articles described studies involving CKD outpatients who were either in stages 3-4 of the disease (five studies), stages 4-5 without dialysis (one study), or were receiving HD (four studies). These studies were further grouped based on the type of supplement that was used for treating the participating patients (Table I). While two studies tested the effectiveness of prebiotic products in patients with CKD, the remaining eight studies investigated the efficacy of either probiotics (four studies) or symbiotics (four studies) in these patients.
PARTICIPANT CHARACTERISTICS
A total of 423 subjects participated in the clinical trials, and the sample size ranged from 12 to 125. Their mean age ranged from 26 to 82 years and 64.18% of the participants were male. The sample sizes of three studies were similar, all of which involved patients with stages 3-4 of the disease (Table I).
Table I. Characteristics of selected studies and their major results
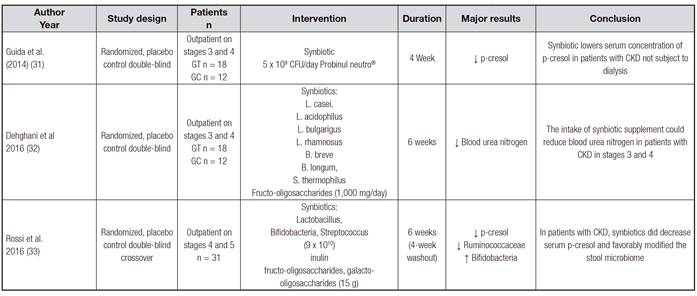
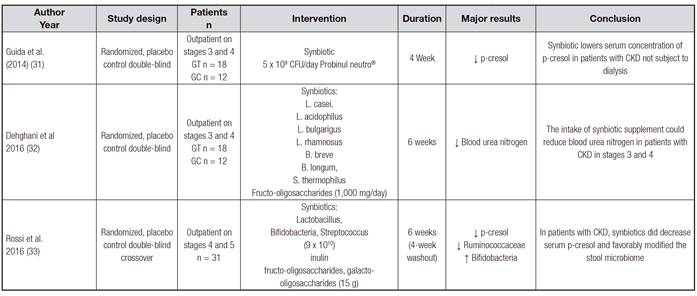
G1: group 1; G2: group 2; G3: group 3; GC: group control; GT: group test; IS: indoxyl sulfate; NF-kB: nuclear factor kappa beta; TC: triglycerides; CRP: C-reactive protein; TAC: total antioxidant capacity; MDA: malondialdehyde; TNF-α: tumor necrosis factor α; IL 6: interleukin 6; IL 8: interleukin 8. *Phases 3 and 4: phase of the chronic kidney disease preceding the hemodialysis phase.
INTERVENTIONS
Interventions with prebiotics in HD patients showed that the consumption of dietary fermentable fiber (10 g and 20 g for six weeks) and the consumption of lactulose (30 mm three times a day for eight weeks) improved lipid profiles (total cholesterol and LDL) and oxidative status (increased total antioxidant capacity and decreased malondialdehyde), suppressed the systemic inflammatory responses (TNF-α, IL-6, IL-8, and CRP), and increased bifidobacteria and lactobacillus counts 24,25.
Probiotic supplementation used in outpatient treatment (16 × 109 colony forming unit [CFU]/day of Lactobacillus casei shirota for two months; and 9 × 109 CFU/day of Lactobacillus acidophilus [L. acidophilus], Bifidobacterium longum [B. longum], and Streptococcus thermophilus [S. thermophiles] for three months) decreased the concentrations of blood urea and uremic toxins in treated patients. In addition, HD patients who received 2 × 109 CFU/day of B. longum demonstrated a reduction in their serum phosphate concentrations 26,27,28. However, probiotics had no effect on uremic toxin levels or inflammatory markers in HD patients who used 1.8 × 1011 CFU/day of S. thermophilus, L. acidophilus, and B. longum for two months 29.
Effects of symbiotics were studied in patients receiving outpatient treatment and those receiving HD. An increase in the Bifidobacterium population was observed in subjects who consumed a symbiotic containing L. acidophilus, Bifidobacterium bifidum (2 × 1012 CFU/day), and inulin (2.31 g) for two months. A reduction in serum p-cresol concentration and an increase in stool volume were observed in patients who received 5 × 109 CFU/day Probinul neutro(r) for four weeks. An intake of symbiotic supplement with seven strains of probiotics and fructooligosaccharides (500 mg twice a day for six weeks) reduced blood urea nitrogen in patients with CKD stages 3 and 4. The symbiotic intervention that used three different types of fibers (15 g) and a combination of probiotics (Lactobacillus, Bifidobacterium, and Streptococcus genus [9 × 1010 CFU] for six weeks [4-week washout]) also showed an increase in the Bifidobacterium population and a reduction in serum p-cresol concentration 30,31,32,33.
DISCUSSION
In CKD, oxidative stress and inflammation occurs at the onset of the disease and increases with its progression. HD individuals experience increased oxidative stress possibly due to loss of antioxidants during dialysis, interactions between blood and dialysis membrane, and malnutrition 34. However, despite the fact that HD patients present greater oxidative stress and inflammation than other outpatient-treated patients, the results of selected studies indicate that the consumption of prebiotic 24,25, probiotic 26,27,28,29, and symbiotic 30,31,32,33 supplementation causes positive changes in HD and CKD patients.
Prebiotics are non-digestible food compounds that stimulate the beneficial growth of microbiota conferring health benefits to the host. They decrease oxidative stress, systemic inflammation, and the production of uremic solutes in CKD patients 35,36. In a randomized placebo-controlled trial, prebiotic consumption for six weeks by individuals receiving HD was associated with the following changes: reduced levels of total cholesterol and LDL, increased oxidative stress through reduction of malondialdehyde and increase of total antioxidant capacity, and improvement in systemic inflammation (TNF-α, IL-6, IL-8 and CRP) 24. These effects may be due to the ability of dietary fibers to hinder the process of dietary fat digestion and absorption, and favor the production of short chain fatty acids. During micelle formation phase of the digestion process, dietary fibers bind to cholesterol or bile acids forming a gel. This binding reaction delays gastric emptying, decreases dietary fat absorption and bile acid reabsorption by the enterohepatic circulation, and drives the use of hepatic cholesterol for bile acid production 37. Dietary fibers are not digested by humans; they are rather fermented by the intestinal bacteria that release short chain fatty acids. These fatty acids are responsible for modulating the intestinal microbiota and exerting immunomodulatory effects 31,37. Such changes in the intestinal microbiota were observed in a randomized controlled clinical trial. In this study, 30 mm of lactulose supplement three times a day for eight weeks increased bifidobacteria and lactobacillus counts in HD patients 25.
Probiotics are live microorganisms that, when administered in appropriate amounts, may confer benefits to the host's health 27.
Their effect on the immune system is evidenced by an increased expression of anti-inflammatory cytokines (interleukin 10 and nuclear factor kappa b), and a decrease in proinflammatory cytokines (interleukin 6 and TNF) and levels of systemic inflammation 38,39.
In a randomized clinical trial, the consumption of probiotics containing 16 × 109 CFU/day of L. casei shirota for two months reduced the levels of serum urea in uremic patients with moderate to severe CKD (stages 3-4) 26. Similar results were observed in a pilot study that tested the effects of a probiotic containing different bacterial strains (L. acidophilus, B. longum, and S. thermophilus) at a dose of 9 × 109 CFU/day. After three months, the majority of the participants who received probiotic had reduced concentrations of serum urea nitrogen and uric acid, contributing to a better quality of life for those individuals 27. Oral administration of B. longum capsules in a placebo-controlled clinical trial was shown to reduce serum phosphorus concentrations in HD patients 28. This suggests that the reduction of these metabolites in CKD patients may be associated with the ability of the microbiota to use the metabolic waste as a substrate. A possible explanation for the observed reduction in uremia is related to the ability of certain anaerobic bacteria to degrade urea and uric acid through the production of enzymes, such as uricase, allantoinase, and urease. In an in vitro study, Lactobacillus exposure to an urea-enriched environment induced the production of enzymes responsible for urea reduction 40. Following the intake of probiotics, an increase in Lactobacillus and Streptococcus populations in the feces can be explained by the conversion of urea to ammonia, a source of nitrogen for metabolic purposes 27. Probiotics can increase dietary fiber fermentation, reduce the intestinal pH, modulate the intestinal microbiota, and increase calcium ionization. Calcium, in turn, binds to phosphorus, reducing its absorption and leading to a reduction in serum phosphorus concentration 28. On the other hand, serum levels of uremic toxins and inflammatory markers were not affected in HD individuals who received a daily dose of 1.8 × 1011 CFU/day of a probiotic (containing S. thermophilus, L. acidophilus, and B. longum) for two months. However, the results showed a trend for the reduction of C-reactive protein (p = 0.071), indoxyl glucuronyl (p = 0.058), and white blood cell counts (p = 0.057) 29. We believe that if the probiotics were administered in combination with soluble fibers, the results would have been different; this is based on our knowledge that soluble fibers can potentiate the effects of probiotics, resulting in a reduction of these markers. A decrease in uremic toxin concentration may be associated with fermentation of soluble fiber by intestinal anaerobic bacteria. This process of fermentation increases the production of short chain fatty acids and reduces colonic pH. The modified environment favors the growth of beneficial bacteria, inhibits the enzymes involved in generation of p-cresyl sulfate and indoxyl sulfate, improves epithelial barrier function (via induction of mucin production, blocking epithelial binding receptors, and strengthening epithelial tight junctions), and reduces the influx of uremic toxins 41 (Fig. 2).
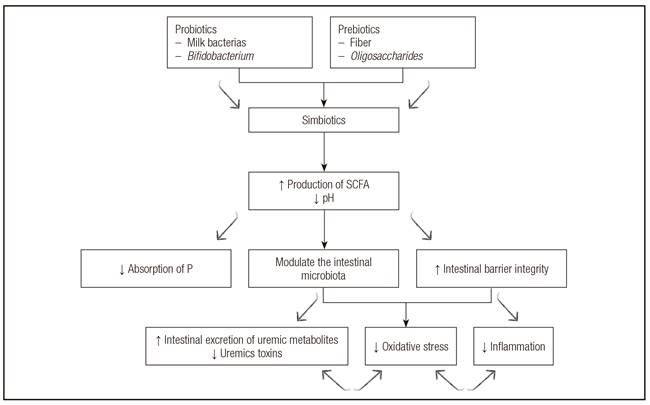
Figure 2 Potential mechanisms involved in the modulation of intestinal microbiota and the reduction of oxidative stress and inflammation by pre- and/or probiotic products in chronic kidney disease. SCFA: short-chain fatty acids; P: phosphorous.
Supplementation of a symbiotic compound containing L. acidophilus and B. bifidum (2 × 1012 CFU/day) and inulin (2.31 g) for two months improved intestinal dysbiosis in individuals receiving HD, increasing the population of Bifidobacterium and preserving the numbers of Lactobacillus in the gut 30. Symbiotic intake in different stages of CKD decreased p-cresol serum concentration and normalized bowel habits 31,33. The symbiotic supplement (seven strains of probiotics and fructooligosaccharides), when consumed 500 mg twice a day for six weeks, can reduce blood urea nitrogen in patients with CKD at stages 3 and 4. One of the mechanisms by which this supplementation can potentially benefit the kidneys is by stimulating growth of gut microbial biomass by increased consumption of dietary fibers; this subsequently decreases ammonia production, increases the ratio of ionized ammonia, and facilitates the use of nitrogenous wastes by bacterial cells. Thus, more ammonia is excreted through the feces, and there is a low level production of potentially damaging forms of nitrogen, such as urea, uric acid, and creatinin 32. These results indicate the need to conduct a study to assess microbiota composition, uremic parameters, and inflammatory biomarkers in response to consumption of symbiotics.
In summary, the mechanism by which prebiotics and/or probiotics modulate the intestinal microbiota and decrease oxidative stress and inflammation may be due to increased intestinal anaerobic bacteria count and maintenance of intestinal barrier integrity (Fig. 2). Intestinal barrier integrity may be improved by the production of mucin, blocking of connection receptors, and strengthening of the epithelial junctions 17.
Due to the inclusion and exclusion criteria adopted in this study, we could include only ten studies in our review, and this limitation did not allow us to carry out a meta-analysis study. Our search for relevant studies was confined to the main databases; thus, it is possible that we might have limited our numbers by missing out some studies that fulfilled our inclusion criteria. Nonetheless, despite these limitations, the present study allowed us to identify "the gaps" in the literature in relation to the topic of interest, allowing us to propose future studies to unravel the mechanisms by which the prebiotics and/or probiotics can control progression of CKD.
CONCLUSIONS
Prebiotics and/or probiotics can modulate the intestinal microbiota by promoting the growth and metabolism of anaerobic bacteria, decreasing the production of uremic solutes, and resulting in oxidative stress and systemic inflammation. There is scarcity of studies that address the effects of prebiotics and/or probiotics on the intestinal microbiota, oxidative stress, and inflammation in CKD patients. Therefore, future studies are needed to provide clarification on topics, such as mechanisms that link regulation of dysbiosis and manifestation of diseases associated with CKD or its precursor diseases, such as diabetes mellitus, hypertension, and atherosclerosis.















