INTRODUCTION
The incidence and prevalence of overweight and obesity have progressively increased in recent years, reaching values of 10 % to 30 % in childhood, and 30 % to 40 % in adolescence (1,2). These health problems have been linked to various comorbidities such as metabolic syndrome, type-2 diabetes, high blood pressure, cardiovascular disease, brain atrophy, and even cognitive disorders. At the cognitive level, obesity has been linked to deficits in school performance, interfering with cognitive functions such as memory, attention, and verbal and motor skills at all ages. These deficits may be due to the fact that excess body fat causes various alterations: insulin and leptin resistance, reduction of anti-inflammatory mediators, and a significant increase in pro-inflammatory mediators, among others (3-7). The inflammatory phenomenon observed in patients with excess fatty tissue is capable of significantly promoting inflammation of the neural tissue (neuroinflammation), and therefore alterations in neural function (2,8). Several studies have detected a reduction in the performance of executive function and verbal memory in adults with a high body mass index (BMI), compared to those who have a BMI within normal values (9-11). Concerning the pediatric population, evidence shows conflicting results. In a case-control study, it was reported that obese children older than 12 years exhibited a decrease in cognitive flexibility, motion ability, and attention capacity when compared to the group with normal weight (12). Other authors have reported that there is no relationship between BMI and cognitive tests in children and adults (13); however, other studies have shown that obese children exhibit decreased memory, abstract reasoning, verbal skills, and executive function (14,15).
In the present study we aimed to determine the difference that exists in the cognitive function of children from 8 to 12 years of age with normal weight, overweight or obesity.
MATERIAL AND METHODS
STUDY DESIGN
An observational, analytical, cross-sectional study was carried out in 46 children (16 males and 30 females) between 8 and 12 years of age from a public school in the State of Mexico. A nutritional assessment was performed, and children were classified into three study groups: 1) normal-weight children (n = 17); 2) overweight children (n = 13); 3) obese children (n = 16). Table I shows the inclusion criteria for each group. After the nutritional assessment, four cognitive function tests were performed, which are described below.
As this investigation was an exploratory study, sample size was determined by the feasibility of recruitment. A sample of 13 children per group was established considering that the number of children per group at school—with the criteria required for the study (overweight and obese)—fluctuated between 13 and 18 children. This sample size allowed the detection of an effect size of 0.1 or larger. In order to reach the established sample, we recruited 17 children per group according to the inclusion criteria for each group (Table I). From these children, four from the overweight and one child from the obese group were excluded from the study, as they did not complete the cognitive tests.
ETHICAL CONSIDERATIONS
This investigation was carried out under the guidelines of the Declaration of Helsinki, the regulations of the General Health Law on Health Research Matters, and the Official Mexican Standard NOM-012-SSA3-2012. A letter of informed consent was obtained from family members and a letter of assent was obtained from each child included in the study. Patient records were always kept anonymous, and confidentiality was guaranteed for each child by providing a consecutive number on confidential files (16). All procedures were approved by the Research Committee at the Faculty of Health Sciences, Universidad Anáhuac México Campus Norte with the number 2015-08.
OVERWEIGHT AND OBESITY DIAGNOSIS
The nutritional diagnosis was made by nutritionists taking into account both anthropometric and clinical indicators. The standardization process was performed with prior training of personnel in the correct use of anthropometric equipment.
Anthropometric assessment
Weight (kg), height (cm), arm circumference (cm), tricipital skinfold (mm), and waist circumference (cm) were measured using the indicators of percentage of height for age, BMI (kg/m2), and percentage of body fat. Height for age and BMI were measured to rule out chronic and acute malnutrition, respectively. Triceps skinfold and arm circumference were measured to assess body fat percentage using Frisancho's formula (2).
The following measurement instruments were used for anthropometric assessment: scale with stadiometer (SECA), fiberglass measuring tape (SECA), and plicometer (Harpenden). A trained clinical nutritionist measured all parameters.
COGNITIVE FUNCTION ASSESSMENT
Two tests were carried out to determine cognitive impairment (CI). Two other tests were performed to define the degree of cognitive ability deficiency. All tests were applied and evaluated by an expert psychologist in cognitive function.
Karen Machover projective test
This test consists of the child drawing on a blank paper a person and writing a short story about the person drawn. For the interpretation, each part of the body, the dimensions of the parts of the body, the omission of a line, and other aspects are evaluated. This allows obtaining data on psychomotor disorders or cognitive deficiency. The suspicion of cognitive function impairment is based on the type of drawing that the child makes since, depending on age, the child must have certain motor, perceptual, and visual abilities. If the drawing shows characteristics that represent a lower chronological age (disproportionate dimensions, lack of congruence between the parts that make up the drawing, etc.), it would indicate potential cognitive impairment (17-21).
Projective test: draw a person in the rain
This test is a complement to the "Karen Machover projective test"; however, it has an important difference: there is a stress factor, a person in the rain. The interpretation of this test is very similar to that of Karen Machover; however, it also takes into account the way the child behaves with the presence of the stress factor. The latter could be observed with the presence of the following objects in the drawing: umbrellas, clouds, lightning, facial expression, among others (18-22).
This test defines the existence or not of cognitive impairment. The results are obtained in the same way as those from the "Karen Machover projective test".
Bender-Gestalt test
This test consists of asking the child to draw 9 white cards with 9 different figures. The interpretation is performed according to the Koppitz scoring system, which gives a score that represents the cognitive age of the child. Shape distortion, rotation, omissions, sequence, overlay of figures, presence of circles or stripes instead of dots, wavy lines, shape of circles, wrong number of dots, presence of angles in curves, omission or addition of angles and boxes, among others, are items taken into account to provide a score for the child. The higher the score, the lower the cognitive age. A score of 1 represents a cognitive age of 10 to 12 years while a score greater than 13 represents a cognitive age of 5 years. Subsequently, cognitive age is compared to the chronological age of the child to establish the degree of cognitive development (23).
Comparison of cognitive and chronological age:
André Rey for children test
This test consists of copying and later reproducing by memory a complex geometric drawing. The figures consist of a series of geometric elements that are identified separately. The results are classified according to the figures that are reproduced correctly (or according to the deformation of the figures) and the time required to carry them out. The results are then classified by percentiles according to the age of the patient. A percentile < 15 indicates medium cognitive ability deficiency; of 15-25, low cognitive-ability deficiency; of 25-75, average cognitive ability; and > 75, above-average cognitive ability (24).
STATISTICAL ANALYSIS
The results of the study were analyzed using the Statistical Package for the Social Sciences (SPSS). The statistical analysis was performed using the proportion z-Test. This test compares two proportions to find differences between them. In this study, we first compared, in the same group, the proportion of patients versus those without cognitive impairment. Afterwards, inter-group comparisons of patients with cognitive impairment were performed. Statistical significance was established at p ≤ 0.05.
RESULTS
The study was carried out in 46 children, 16 males and 30 females, with an average age of 10 years and 7 months, and a range of 8 to 12 years. Table II shows the demographic characteristics of the patients in the study.
Table II. Demographic characteristics of the patients in the study
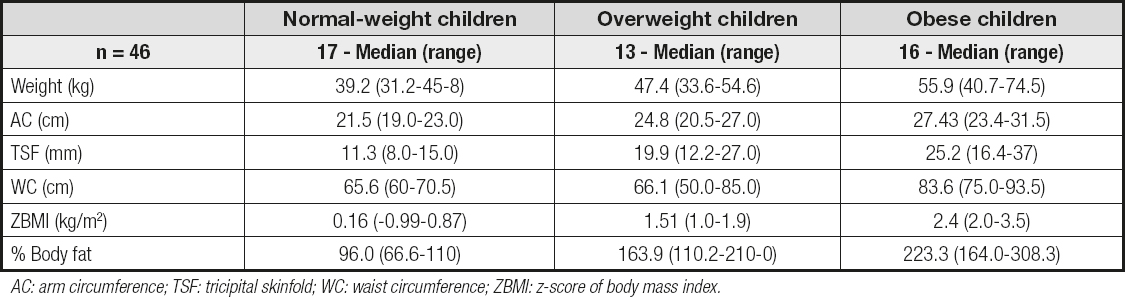
AC: arm circumference; TSF: tricipital skinfold; WC: waist circumference; ZBMI: z-score of body mass index.
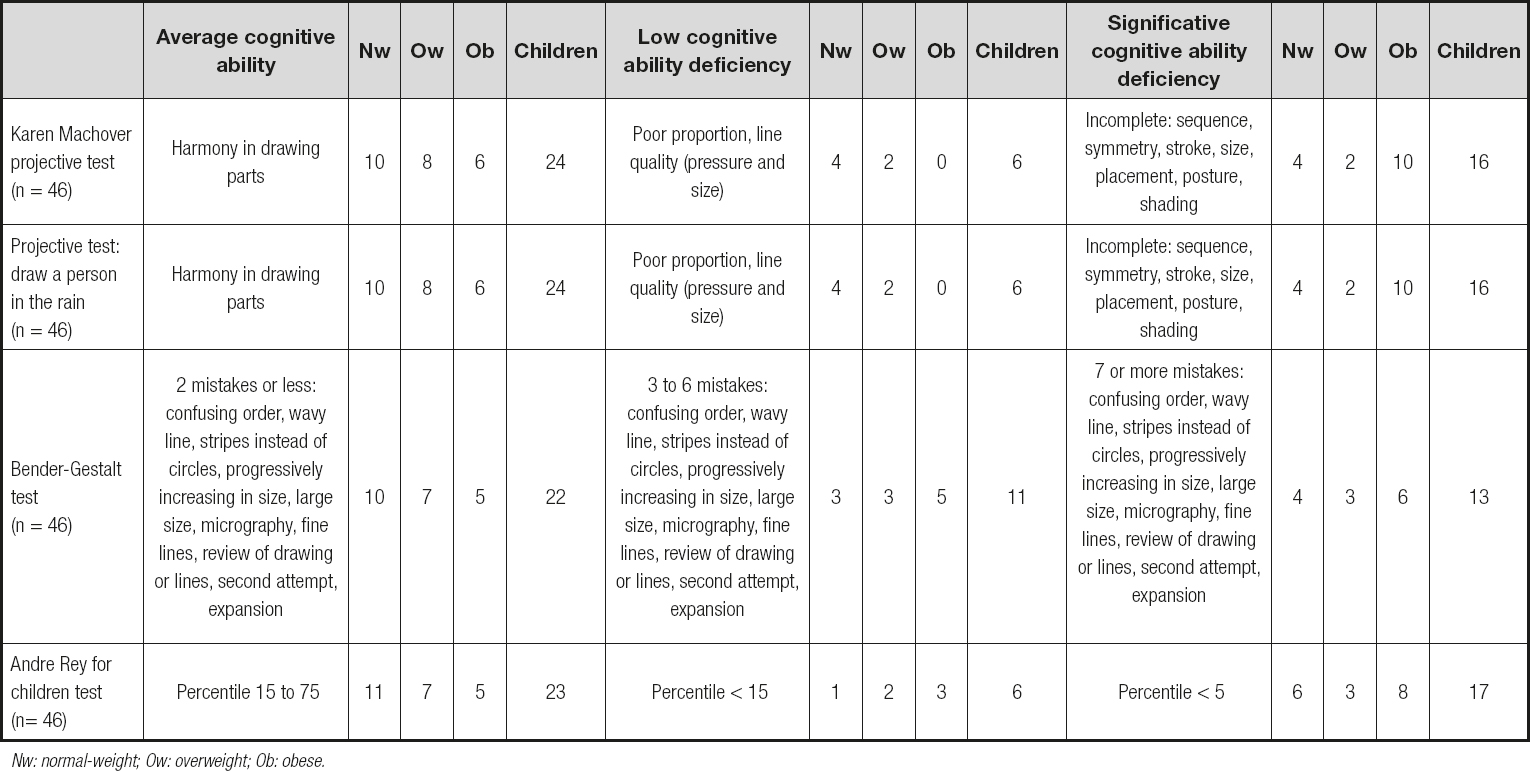
The results of each cognitive test are shown in Table III. This table also specifies how the cognitive status was classified.
Figure 1 shows that the majority of obese patients presented cognitive impairment (63 %), and this proportion was significantly higher than among those who did not show cognitive alterations in the same group (37 %; p = 0.012; proportion z-Test). This proportion was also significantly higher than the ones observed in the other groups (p = 0.02). In the group of overweight patients we found a very similar distribution to that presented in the normal-weight group. In both groups the proportion of patients without cognitive impairment was high. However, only in the case of the normal-weight group the difference between patients with and without cognitive impairment was significant (overweight group: p = 0.370; normal-weight group: p = 0.015; proportion z-Test).

Figure 1. Cognitive impairment in the study groups. A higher proportion of obese children presented cognitive impairment. The bars represent the percentage of the total children in each group. *p = 0.015; **p = 0.020; ***p = 0.012. CI: cognitive impairment.
With the objective of analyzing the degree of cognitive development, according to nutritional status, we determined the average cognitive ability in each group. According to this evaluation the cognitive ability deficiency could be low, medium or high (23,24). Figure 2 shows that a significant percentage of obese patients (80 %) presented medium cognitive deficiency (p = 0.019; proportion z-Test). This proportion was significantly higher than in the other groups (p < 0.05). In the case of overweight and normal-weight patients, the proportions were very similar between them and there was no significant difference between low and medium impairment.

Figure 2. Degree of cognitive ability deficiency in the study groups. A majority of obese children presented medium cognitive ability deficiency. The bars represent the percentage of the total number of children with cognitive impairment in each group. *p = 0.019; **p < 0.05. CI: cognitive impairment.
With the objective of analyzing whether excess body weight, that is, that of overweight and obese patients (OwOb), significantly changed the proportion of patients with cognitive impairment, the differences in cognitive function between patients with normal weight and OwOb were also evaluated. Figure 3A shows how the cognitive function behaves in the OwOb group and in the normal-weight group. The OwOb group exhibited a significant increase in the percentage of patients with cognitive impairment (p = 0.020; proportion z-Test). This proportion was significantly higher than the one presented by the normal-weight group (p = 0.015). On the other hand, the normal-weight group presented a significantly lower percentage of patients with cognitive impairment (p = 0.010).

Figure 3 A. Cognitive impairment in OwOb children. When analyzing OwOb children together, a higher proportion of children with cognitive impairment is still observed. The bars represent the percentage of the total children in each group. *p = 0.010; **p = 0.020; ***p = 0.015. CI: cognitive impairment; OwOb: overweight and obese. B. Degree of cognitive-ability deficiency in OwOb children. A majority of OwOb children presented medium cognitive deficiency. The bars represent the percentage of the total number of children with cognitive impairment in the two groups. *p = 0.010; **p < 0.05. CI: cognitive impairment; OwOb: overweight or obese.
When evaluating the degree of cognitive ability deficiency in the OwOb group, it can be seen in figure 3B that a higher proportion of OwOb patients exhibited a medium cognitive-ability deficiency level compared to those with low cognitive impairment (p = 0.010; proportion z-Test). This proportion with medium cognitive deficiency was also significantly higher than among patients with normal weight (p < 0.05). Regarding the normal-weight group, there was no significant difference in average of cognitive ability (p = 0.324).
DISCUSSION
In the present study, it was found that a higher proportion of obese children tend to present significant cognitive impairment, and that this group has a higher degree of severity when compared to both the overweight and normal-weight groups.
Our results agree with previous studies that had reported a significant effect of obesity on cognitive function in children and adolescents (25-28).
In the present study we found a significant increase not only in cognitive impairment but also in its degree of severity among obese patients. Similarly, when we analyzed OwOb patients together, a significant increase in the proportion of patients with cognitive impairment was observed. These results open the possibility that excess body weight could make a significant difference in the cognitive function of children, generating a long-term negative effect. Our work also suggests that children who are only overweight still have the possibility of avoiding the development of cognitive impairment if they change their habits, since in the present study the results of these children were very similar to those found for normal-weight children.
The possible inducing mechanisms of cognitive impairment in obese patients are diverse, including alterations in glycoregulation, reduction of neurotrophin levels, neuroinflammation, and structural alterations of the blood-brain barrier. Cytokines appear to have an important role in obesity and neurodegeneration (25,29).
Recent research has suggested that, under conditions of obesity, in adipose tissue there is an increase in the release of adipocytokines that are highly inflammatory, such as leptin, tumor necrosis factor alpha (TNF-alpha) and interleukin 6 (IL-6), among others (30).
These alterations lead to a chronic inflammatory state with repercussions at both the local and systemic levels, which causes alterations in the brain, especially in the hypothalamus. This neuroinflammation is likely causing synaptic remodeling and neurodegeneration in the hypothalamus, thereby altering the internal and output circuits to other regions of the brain. The final result is a disruption of cognitive function (31).
Although the mentioned mechanisms remain theories, the increase in IL-6 has been shown to cause long-term memory impairments. Similarly, insulin resistance seems to play an extremely important role in cognition, since excess abdominal adiposity and insulin resistance have been shown to cause cognitive impairment in patients of all ages (29,32-40).
CONCLUSIONS
In the present study it is observed that cognitive impairment is greater in obese children from 8 to 12 years of age when compared to those who are only in the overweight or normal-weight groups. Cognitive processes can be influenced by chronic inflammation as induced by excess body weight.