INTRODUCTION
Diabetes mellitus (DM) is a group of metabolic diseases characterized by hyperglycemia, which has gradually developed into one of the health-threatening factors leading to premature death worldwide (1). According to the data released by International Diabetes Federation (IDF) in 2017, there are currently about 425 million DM patients in 2017 around the world, and this number is estimated to increase to 629 million by 2045. In 2017, about 352 million patients were at risk of DM, about 4 million people died of DM, and about 21 million newborns were affected by DM during pregnancy; additionally, the global DM-related medical costs have reached 727 billion US dollars in 2017, accounting for 12 % of adult medical costs (2). DM is mainly divided into three different types: type-1 DM (T1DM), type-2 DM (T2DM) and gestational DM (GDM). T2DM accounts for more than 90 % of the total number of DM patients (3).
The causes and pathogenesis of DM are complex, and this disease can develop many complications resulting in severe consequences (4,5). Therefore, early treatment and early intervention are needed in DM patients. Treatment modalities for DM now include drug therapy, exercise therapy, lifestyle intervention, and dietary therapy (6,7). Although great progress has been achieved in drug therapy in recent years, the adverse reactions and potential hazards of drugs still make people maintain a great vigilance for the safety of this therapy. Thus non-pharmacological treatment options tend to be more popular, such as very low-carbohydrate ketogenic (VLCK) diet therapy composed of low carbohydrate, high fat, and moderate protein (8).
VLCK diet, as one of the non-pharmacological treatments for refractory epilepsy, has been used for nearly a hundred years (9,10). This diet recently has begun to be introduced for treating DM patients and has achieved some therapeutic effect (6). Most of the existing studies have pointed out that VLCK diet can effectively reduce glycosylated hemoglobin content, body weight, and triglyceride levels in DM patients (11,12). Also, there is strong evidence that VLCK diet can reduce blood glucose and glycosylated hemoglobin in T2DM patients (13). However, there is no sufficient data regarding whether this low-carbohydrate and fat-rich diet adversely affects lipid metabolism while lowering blood glucose. Therefore, this meta-analysis based on comprehensive literature retrieval in English databases, intends to systematically evaluate the selected randomized controlled trial (RCT) and subsequently investigate the lipid metabolism of T2DM patients after VLCK diet treatment. This study is expected to provide a new scientific basis for non-drug therapy of DM.
METHODS
LITERATURE RETRIEVAL
This meta-analysis was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines (14). PubMed, Cochrane Library, Embase, and Web of Science databases were searched for RCTs published up to September 2021 and regarding VLCK diet therapy in T2DM patients. The keywords searched were as follows: “diabetes mellitus”, “T2DM”, “diabetes”, “VLCK”, “ketogenic diet”, “very low-carbohydrate ketogenic”, “human”. The search language was limited to English. The search was performed jointly by two investigators, and finally a comprehensive analysis was performed to reach an agreement.
INCLUSION CRITERIA AND EXCLUSION CRITERIA OF THE LITERATURE
Inclusion criteria: a) each included study was a RCT; b) the experimental group received a VLCK diet, defined as carbohydrate intake of 50 g/d or 10 % of energy, while the control group had any diet recommended for patients with T2DM; c) studies published in English; d) the study subjects were adult patients with T2DM.
Exclusion criteria: a) incomplete data of original study; b) animal experiment, letter, review, etc.; c) literature with low quality; d) follow-up time < 2 months.
QUALITY EVALUATION
The quality of the included RCTs was assessed according to the modified Jadad scale. The total Jadad score is 7, with a score > 3 indicating a study of high quality, and a score ≤ 3 indicating a study of low quality. The assessment was performed jointly by two investigators.
DATA EXTRACTION
The following information was extracted from the included literature: a) name of the first author, country, year of publication, age and weight of the experimental group and control group, number of participants, treatment method and duration of the intervention; b) mean and standard deviation of outcome measures: triglycerides, total cholesterol, high-density lipoprotein (HDL) and low-density lipoprotein (LDL).
STATISTICAL ANALYSIS
The data were statistically analyzed using Stata 15.0. The I2 statistic was used to quantify the degree of heterogeneity among studies. When I2 was < 50 % and p > 0.05, heterogeneity was considered low and a fixed-effects model (FEM) was adopted; otherwise, a random-effects model (REM) was used. Given that not all outcome measures were reported using absolute values, this study utilized the standardized mean difference (SMD) and 95 % confidence interval (CI) as the effect size. A subgroup analysis of follow-up time was carried out. Further funnel plots and Egger's test were employed for jointly determining publication bias. Finally, a sensitivity analysis was performed to verify the robustness of the obtained conclusions. A p < 0.05 was considered statistically significant.
RESULTS
LITERATURE RETRIEVAL RESULTS
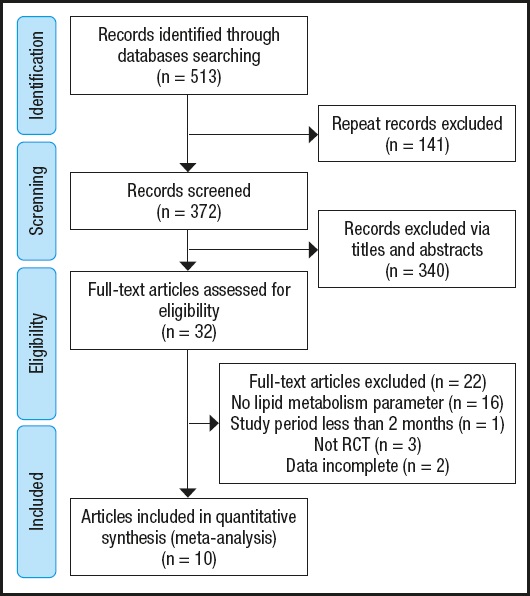
After strict screening, a total of 10 English articles were selected as candidates for inclusion in this meta-analysis (15-24). All the included studies are RCTs with humans as study subjects. The overall screening process is shown in figure 1. The basic characteristics of the included studies are shown in table I.
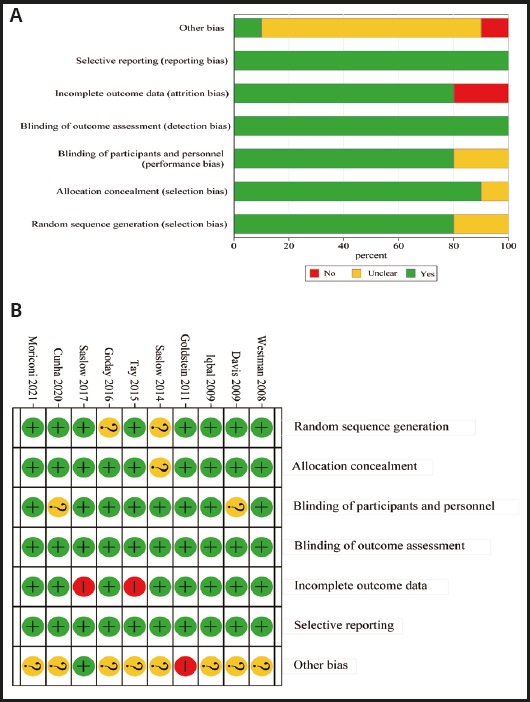
The assessment results of bias risk of the included literature are provided in figure 2 A-B. The modified Jadad scores of the included studies were all > 3, indicating that all included studies were of high quality.
META-ANALYSIS RESULTS
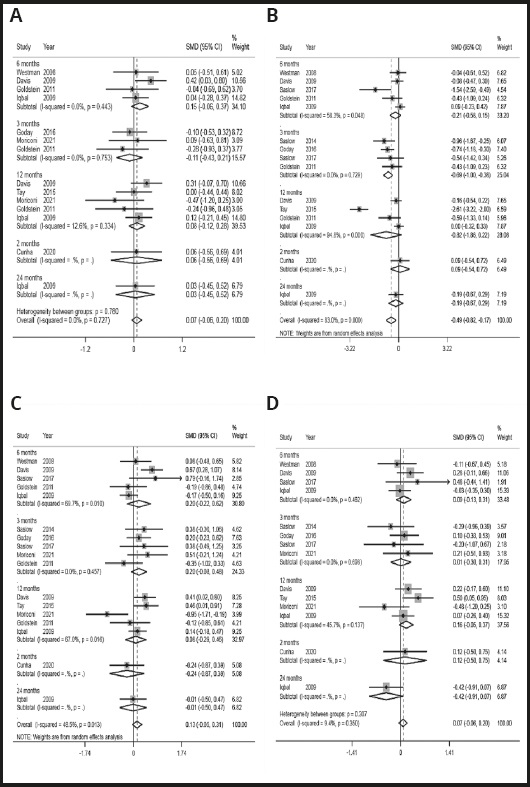
Effect of VLCK diet on total cholesterol
Eight articles reported the changes of total cholesterol levels in DM patients. No significant heterogeneity was identified among the included studies (I2 = 0.0 %, p = 0.727), so a FEM was used for analysis. The results showed (Fig. 3A) that there was no significant difference in total cholesterol levels after treatment in the experimental group and control group (SMD = -0.07, 95 % CI: -0.06-0.20, p > 0.05). A subgroup analysis of follow-up time showed that there was no difference in total cholesterol levels between the two groups after 3, 6 and 12 months of treatment (p > 0.05).
Effect of VLCK diet on triglycerides
Nine articles investigated the changes in triglyceride levels in DM patients. A REM was adopted for analysis due to significant heterogeneity among the included studies (I2 = 83 %, p = 0.000). The results showed (Fig. 3B) that triglyceride levels decreased significantly after VLCK diet treatment compared with the control group (SMD = -0.49, 95 % CI: -0.82 to -0.17, p = 0.003).
The subgroup analysis of follow-up time showed that after 3 months of VLCK diet treatment, triglyceride levels were significantly reduced (SMD = -0.69, 95 % CI: -1.00 to -0.38), without significant heterogeneity (I2 = 0.0 %, p > 0.05). However, after 6 and 12 months of treatment, there was no significant difference in triglyceride levels between the two groups (p > 0.05).
Effect of VLCK diet on HDL
Ten articles compared the changes of HDL levels in DM patients. Marked heterogeneity was identified among the included studies (I2 = 48.5 %, p = 0.013), so a REM was used for analysis. The results showed (Fig. 3C) that there was no significant difference in HDL levels after VLCK diet treatment compared with control group (SMD = 0.13, 95 % CI: -0.05-0.31, p > 0.05). According to the subgroup analysis of follow-up time, no difference was found in HDL levels between the two groups after 3, 6 and 12 months of treatment (p > 0.05).
Effect of VLCK diet on LDL
Nine articles compared the changes of LDL levels in DM patients. A FEM was employed for analysis (I2 = 9.4 %, p = 0.35), and the results revealed (Fig. 3D) that there was no significant difference in LDL levels after VLCK diet treatment compared with the control group (SMD = 0.07, 95 % CI: -0.06-0.20, p > 0.05). According to the subgroup analysis of follow-up time, there was no difference in LDL levels between the two groups after 3, 6 and 12 months of treatment (p > 0.05).
PUBLICATION BIAS
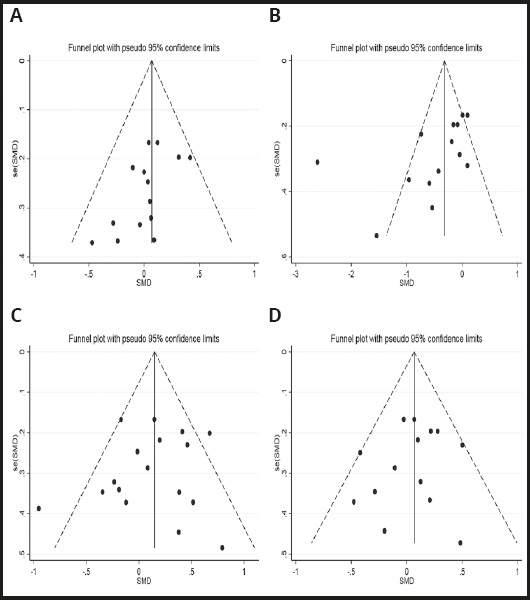
Publication bias was assessed using funnel plots and Egger's test. Funnel plots were drawn regarding total cholesterol (Fig. 4A), triglyceride (Fig. 4B), HDL (Fig. 4C), and LDL (Fig. 4D), respectively. By observing the plots, asymmetery was present in both the funnel plots of total cholesterol and triglyceride, and the p-values of Egger's test were 0.037 and 0.044, respectively; the results indicated that there was a certain publication bias in these two indicators. By contrast, both the funnel plots of HDL and LDL levels were basically symmetrical, and the p- values of Egger's test were all > 0.05, suggesting that there was no significant publication bias in these two indicators.
SENSITIVITY ANALYSIS
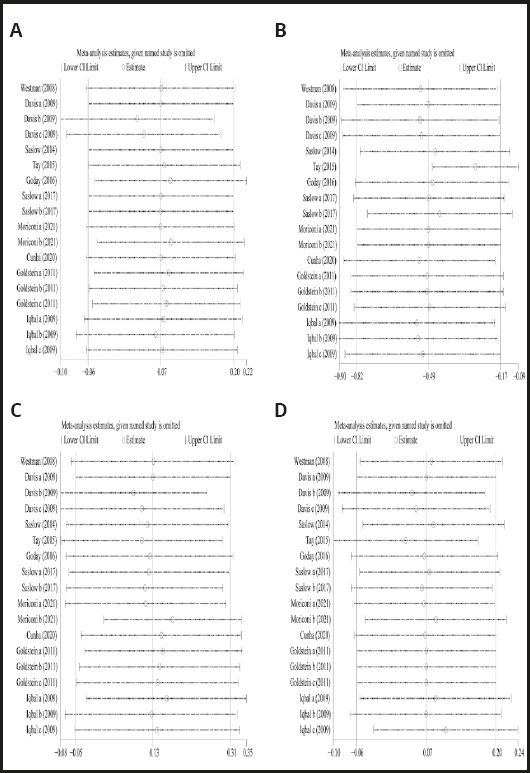
After each study was removed, one by one, a meta-analysis was performed to compare the differences before and after removal. After removing the studies regarding total cholesterol (Fig. 5A), triglyceride (Fig. 5B), HDL levels (Fig. 5C), or LDL levels (Fig. 5D), one by one, the meta-analysis results were not significantly different from those before removal, indicating that the conclusions obtained in this study were robust.
DISCUSSION
People's living standards have been continuously improved, but the consequent poor dietary habits and heavy pressure of city life have led to an increasing incidence of DM. If DM is not treated with long-term appropriate and comprehensive treatment to delay its progression, the incidence of the short-term and long-term complications of DM may increase, resulting in a threat to people's health (25,26). Among the treatments for DM, dietary management and dietary treatment may be an economical and effective non-pharmacological treatment (27,28). VLCK diet, as a non-drug alternative dietary therapy, is relatively safe and effective (28).
All 10 articles included in this study were English-language articles, and their modified Jadad scores were above 3. This means that we ensured the reliability of the included articles in the section of study selection. VLCK diet for DM patients is a low-carbohydrate diet accompanied by high fat content. A concern with a high-fat diet is whether it affects the patient's lipid metabolism, leading to increased levels of total cholesterol, triglycerides, and LDL, decreased HDL levels, and ultimately risk of cardiovascular disease. Also, it has been reported that elevated levels of LDL and cholesterol significantly increase the risk of coronary heart disease (29). A meta-analysis by Pullinger et al. showed that prebeta-1 HDL levels are an independent positive risk factor for coronary heart disease and myocardial infarction (30). Our meta-analysis results found that there were no differences between T2DM patients receiving VLCK diet and control diet in total cholesterol, HDL, and LDL levels. Further, a subgroup analysis revealed no significant differences between the two groups in these three indicators after 3, 6, and 12 months of treatment. Triglycerides is another important indicator of blood lipid metabolism; in this study, triglycerides decreased significantly in the experimental group compared with the control group, indicating a favorable effect of the VLCK diet; however, there is also significant heterogeneity among studies regarding triglyceride. In the subgroup analysis of follow-up time, the decrease in triglycerides in T2DM patients receiving VLCK diet was still statistically significant when compared with the controls after 3 months of treatment, and moreover, heterogeneity was low; however, this difference disappeared after 6 and 12 months of treatment. That is, the VLCK diet presented a short-term effect of lowering triglyceride levels. The sensitivity analysis of these four lipid metabolism indicators showed that after excluding any study, the conclusion had had no significant change compared with that before removal, indicating that the conclusion obtained in this meta-analysis had good robustness. But we also noticed that both the funnel plots and Egger's test suggested that there was some publication bias in total cholesterol and triglycerides. Therefore, the conclusion on these two indicators still needs to be cautious, and more studies need to be included to reduce publication bias and therefore to obtain a more robust conclusion. A meta-analysis by Rafiullah et al. (31) showed that the VLCK diet was associated with a significant decrease in triglycerides when compared with control diet after 3, 6, and 12 months of treatment, and a risk of increased LDL levels was found after 12 months of VLCK diet treatment (weighted mean difference = 6.35, 95 % CI: 2.02 to 10.69). This is not very consistent with the conclusion obtained in our study in which triglycerides only showed a statistically significant difference after 3 months of treatment, with no marked difference after 6 and 12 months after treatment. Additionally, different from the above meta-analysis, our study found that LDL levels had no difference between VLCK diet and control diet after 3 and 12 months of treatment, that is, the VLCK diet did not increase the risk of LDL. The reason for the differences between these two meta-analyses is that our meta-analysis excluded one study (32) that did not meet the inclusion criteria because it included patients with prediabetes. Second, our meta-analysis selected the latest researches. Moreover, given that some original studies use absolute values while others use difference changes, we selected SMD as the effect size. Collectively, the conclusions drawn from our study represent strong evidence.
However, this meta-analysis still has some limitations. First, the number of included studies is relatively small. Second, the number of included cases is also limited. Third, the included articles were all in English, and most of these studies report Caucasian populations but lack investigation on Asian and African populations. Populations in different regions have different dietary habits and living environments, which may cause differences in the effect of VLCK diet for DM patients. Therefore, this study may have limitations in providing a treatment basis for DM in other countries and regions. Fourth, all 10 articles analyzed are published articles, and no unublished high-quality studies were included; therefore, there may be some publication bias. Fifth, the funnel plots and Egger's test showed some publication bias in total cholesterol and triglycerides.
In conclusion, T2DM patients who receive a VLCK diet to lower blood glucose are not associated with increased levels of total cholesterol and LDL, and decreased levels of HDL. Additionally, this diet can achieve a short-term reduction of triglyceride levels. This study has crucial clinical significance and can provide an evidence-based medicine basis for clinicians in the treatment of DM. However, considering the limitations of this study, more in-depth studies are required, carried out in larger samples to verify that the VLCK diet does not affect the lipid metabolism of patients while lowering blood glucose in DM patients, or even has a favorable effect.