INTRODUCTION
Childhood overweight and obesity are a global problem that has worsened in recent decades, affecting countries regardless of their income (1). The multiple factors that cause these metabolic diseases have spread throughout societies, reaching economically and socially disadvantaged populations (2). Furthermore, the consequences of the COVID-19 pandemic can trigger higher prevalences of overweight and obesity in children, as poverty worsens, and sedentary lifestyle widens (3).
The World Health Organization (WHO) defines overweight and obesity as an excessive store of fat that can damage health. In the case of boys and girls, diagnoses of overweight and obesity are considered if the BMI for age is +1 and +2 standard deviations above the median established in the WHO child growth standards, respectively (2).
Excess fat during childhood can cause significant physiological and psychosocial damage affecting quality of life. These damages can extend into adulthood and generate an excessive socioeconomic burden for nations (4).
Risk factors for the development of obesity are numerous and of a different nature (5). They arise from genetics, fetal environment, particular aspects of the mother during pregnancy, current and early childhood diet, physical activity (PA) level, sedentary habits, sleep patterns, family, environment, socioeconomic status, and availability and accessibility of food (6-12). Due to the complexity of this disorder, its control is not easy.
Strictly speaking of vulnerable groups or populations, several definitions emerge in the literature. In general, these suggest that individual characteristics such as age, sex, gender, race, ethnicity, displacement, disability, health status, income level, insurance coverage, and lack of a usual source of care, can cause greater vulnerability in people and communities, and lead to poorer health (13). For this review, we adhere to the definition of a vulnerable population that includes economically disadvantaged racial/ethnic minorities, low-income children, rural residents, the elderly, homeless people, people with the human immunodeficiency virus (HIV), and individuals with chronic illnesses, including mental illness (14).
A lifestyle is demarcated by the deliberate decisions about the behavior and daily consumption practices of everyone. However, the choice and maintenance of lifestyle is strongly influenced by the economy, sociocultural and political environment, exerting effects on health and behavior (15).
It has been pointed out that obesity varies according to socioeconomic level (16), as higher rates are found in boys and girls with fewer resources (17-19). Similarly, schoolchildren from vulnerable groups, such as indigenous and rural communities, have a higher risk of being overweight and obese due to changes in diet and increased sedentary lifestyle in a context of poverty and marginalization (20-23). It has been observed that children from households with food insecurity, closely linked to poverty, have higher figures in variables related to adiposity (BMI Z-score and waist circumference) and higher risk of developing overweight or obesity when compared to children from households with food security (24). For their part, the children of migrants and unemployed parents show a higher risk of sedentary behavior (screen time) and less probability of being part of a sports club (25).
A recent systematic review reported that the variables related to an increased risk of childhood obesity were having parents without support networks, with little help from formal and occasional sources, having parents without work, belonging to a minority group or with an immigrant background, suffer from unfavorable experiences (household disintegration, violence and child abuse), having gender imbalances, and belonging to a non-traditional family. The authors proposed that variables associated with childhood obesity, which are also characteristics of vulnerability, are not related to socioeconomic level. However, they indicate that the socioeconomic level plays a very important role since it is capable of exacerbating or lessening the impact that these variables may have on the lifestyle and mental health of schoolchildren. Similarly, they reported conduct, biological, and mental-related mechanisms as conceivable explanatory factors in the relationship between vulnerability and childhood obesity. Hence, dietary intake, physical activity level, sedentary behavior, and sleep pattern are altered by stress and impair mental health due to the status of vulnerability (26).
In order to face the consequences of obesity, previously intervention programs were designed and applied with an isolated approach, which only treated some of the risk factors, and their results were usually partial, with a short-term effect (27-29). Therefore, in recent years, a new perspective has emerged to address the prevention, maintenance and remission of the disease, giving way to the creation and implementation of Multicomponent Lifestyle Intervention Programs (MLIPs) with a more comprehensive approach (30). These are characterized by a combination of varied components, selected according to the objectives and available resources, that seek to mitigate triggers of overweight and obesity, and can reinforce family and community structures (31-33). The most widely implemented interventions are aimed at generating behavioral changes, modifying dietary habits, and increasing physical activity (34), emphasizing that most obesity intervention programs in children do not consider the characteristics of vulnerability and social inequality, which makes them ineffective in the most vulnerable groups (26).
Other reviews have explored the effectiveness of MLIPs in schoolchildren in high- and middle-income countries. However, knowing the results of these interventions in children from vulnerable groups will be very useful to propose and design projects consistent with the needs, characteristics and response of this population (29). Accordingly, this review aims to elucidate whether these interventions are effective in improving adiposity indicators in the selected groups and, if so, which of them are the most effective.
METHODOLOGY
ELIGIBILITY CRITERIA
Population
The interest group for this review were schoolchildren (5 to 12 years old) with characteristics of vulnerability, whether they lived in a rural area, had a low socioeconomic level and/or belonged to an indigenous community or not. Age was established to include boys and girls who attended elementary school or its equivalent, according to the school system of each country. Studies encompassing populations with a broader age range were eligible for inclusion if ≥ 75 % of the participants were within the specified age range. Boys and girls with any BMI classification were included to incorporate intervention programs with preventive and treatment approaches. Studies in which the population was predominantly made up of schoolchildren with chronic illnesses or disabilities were excluded.
Intervention components
The included MLIPs had to contain at least two components, which could be nutrition, PA, psychology, providing school meals, and/or family/community involvement (FCI), regardless of other elements. The intervention programs were analyzed according to their effect on the variables of interest. Without exception, all intervention programs had to be taught in elementary schools or equivalent settings, during class time or at the end of the school day. No restrictions were imposed on the duration of the interventions, nor on the personnel who delivered them.
Comparison
Studies without a control group and studies in which the control group did not receive the program (they continued with the usual classes) or received only one component were included.
Result variables
This review defined, as primary outcomes, variables related to adiposity such as the prevalence and/or incidence of overweight and obesity, as well as indicators of these health conditions (BMI/BMI Z-score, waist circumference, and percentage of body fat). The secondary outcomes were those related with dietary intake (micro and/or macronutrients), knowledge of nutrition, PA and sedentary behavior. Studies reporting at least one outcome of interest were considered.
SEARCH STRATEGY
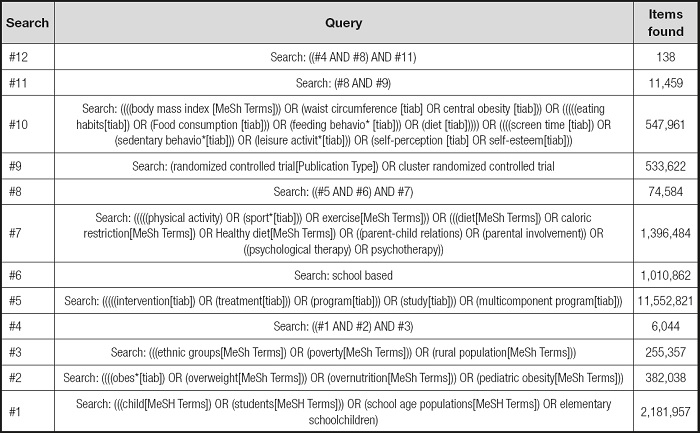
The search was carried out in the electronic databases PubMed (interface National Library of Medicine); MEDLINE (OVID interface); The Cochrane Library - Cochrane Central Register of Controlled Trials (CENTRAL) via Cochrane Register of Studies Online (CRSO); EMBASE (Excerpta Medica database) and in Google Scholar, during the months of November and December 2020. The search strategy consisted of entering the combination of keywords: “multi-component program”, “childhood obesity”, “nutrition assessment”, “education”, “ethnic groups”, “health education”, “elementary schools”, “indigenous populations”, “pre-post tests”, “randomized controlled trials”, among others. The search strategy for PubMed is described in table I; for the other databases, modified versions were used according to the controlled language of each search engine (MeSh terms for MEDLINE and Emtree for EMBASE). The search was filtered by date, considering studies published in English, from 2000 to December 19, 2020. In addition, throughout the search, systematic reviews that included possible relevant studies were identified and the references of these reviews were screened in accordance with the Cochrane Handbook recommendations (35).
SELECTION OF STUDIES
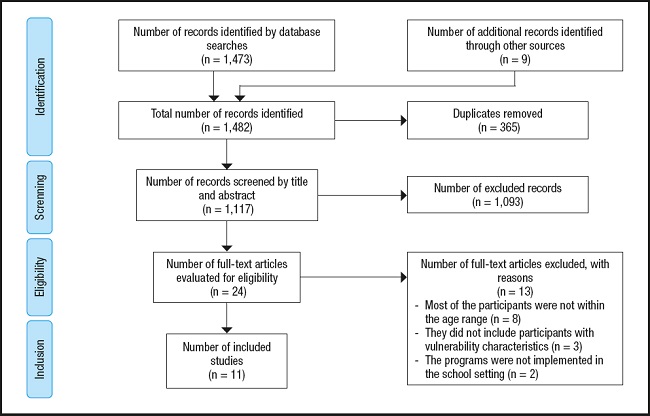
The results obtained from the different databases were imported into the EndNote 20 reference software, which helped eliminate duplicate studies and organize references for further screening. Titles and abstracts of potentially relevant studies were reviewed. Subsequently, the full studies were assessed for inclusion. If the vulnerability condition of the population and the application environment of the program was not clearly defined in the summary section, the study was conducted to the full-text evaluation stage. The study selection process is detailed in the PRISMA flow diagram (36) (Fig. 1).
DATA EXTRACTION
Data on the authors, country of application of the program, study design, sample size, age of participants, description of the program, duration and follow-up, description of control, and variables of interest were extracted from the selected studies. With the results reported by the authors, tables were prepared to visually illustrate the most important changes obtained, also, they were explained narratively and a discussion of them was conducted. A meta-analysis was not possible due to the limited data available and the high variability between studies.
RESULTS
SEARCH RESULTS
The systematic search strategy identified 1,473 articles, plus 9 studies obtained from the references of systematic reviews.
After removal of duplicates, 1,117 titles and abstracts were screened. A total of 11 studies were chosen for inclusion in this review (Fig. 1).
DESCRIPTION OF THE STUDIES
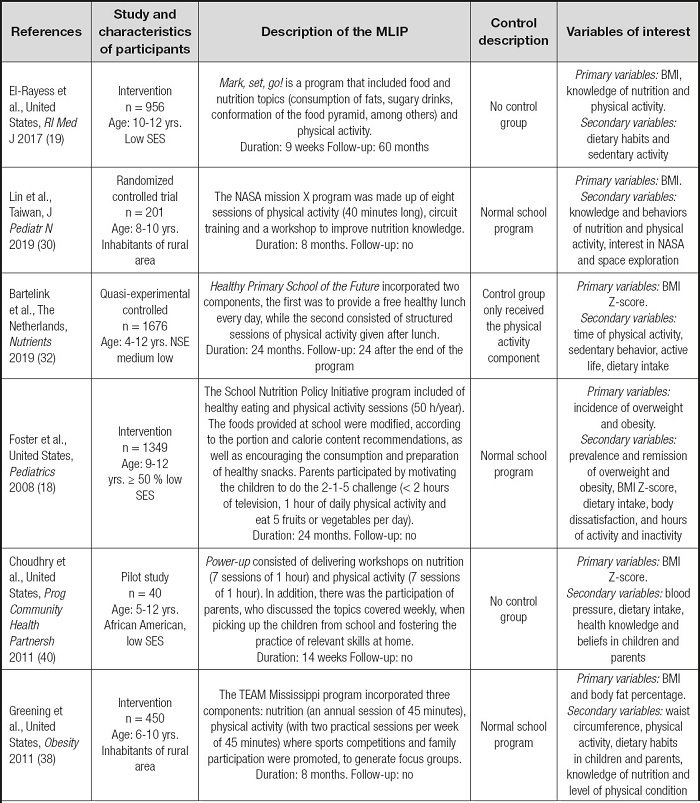
This review considered 11 MLIPs in schoolchildren, made up of two or more components. The studies were conducted in the United States (n = 5), United Kingdom (n = 2), Canada (n = 1), Portugal (n = 1), Taiwan (n = 1) and the Netherlands (n = 1), with publication dates of the articles between 2008 and 2019. The samples of participants were located between 40 and 1,676 children, while the duration of the intervention programs was between 9 weeks and 24 months. The studies included evaluations at different times and only three indicated that there was follow-up, from 6 to 60 months (29,41,45). Most of the studies (n = 6) had a control group, five of them did not receive any intervention component (18,30,37-39) and one received an intervention with partial components (32) (the characteristics of the included studies are in Table II).
Table II (cont.). Characteristics of the included studies.
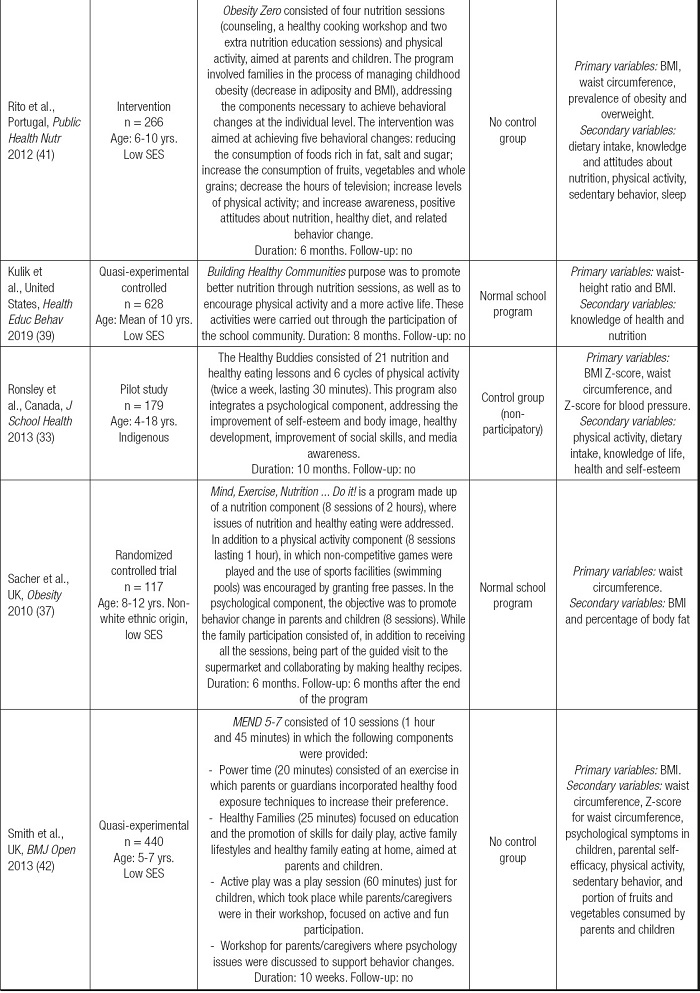
SES: socioeconomic status; BMI: body mass index.
All of the intervention programs included a PA component, 91 % nutrition, 64 % had FCI, 27 % integrated a psychology component, and 9 % provided school meals. Interventions with three components (55 %) predominated, followed by two (27 %) and four (18 %). Regarding the delivery of the interventions, most of them were provided by health professionals (n = 5) and by trained teachers (n = 4) and only two studies were given by trained peers (Table III). Previously trained teachers and peers were those teachers or students who, before starting the intervention, received training courses by the research team that directed the studies, to provide the intervention in the manner established in the different protocols.
Table III. Summary of the results of individual studies grouped by characteristics of the MLIP.
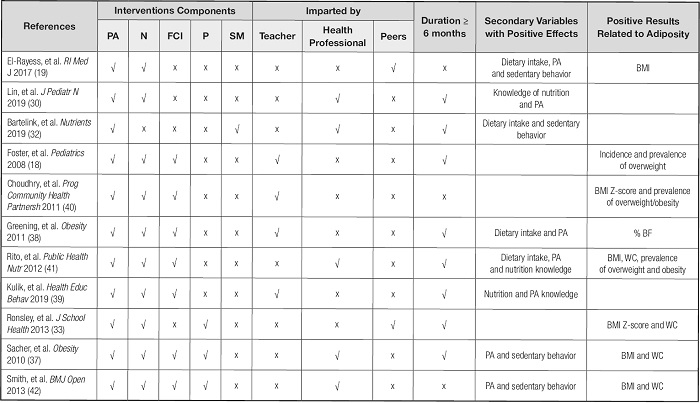
PA: physical activity; N: nutrition; FC: family-community involvement; P: psychology; SM: school meals; BMI: body mass index; WC: waist circumference; % BF: percentage of body fat.
Only three of the 11 included studies investigated the adverse effects of the interventions on the participants (18,32,37). The general features of the components contained in the included MLIPs are described below:
− PA components: they consisted of sessions of knowledge and practice of physical activity and a more active lifestyle. With complementary activities such as raffles for sporting goods, non-competitive games, tournaments, free passes to sports facilities.
− Nutrition components: they were based on sessions on healthy eating and nutrition. With complementary activities such as nutritional counseling, guided visits to the supermarket, healthy cooking workshops, modifying the school cafeteria menu and playing various games to reinforce knowledge.
− FCI components: they consisted of fostering support and motivation for children; in addition to the family receiving the rest of the interventions. The community was also involved in recreational activities.
− Psychology components: psychological sessions were provided with a focus on behavior change, self-esteem improvement, body image and social skills.
− School meal components: free breakfast, snack and/or healthy lunch delivery.
EFFECTIVENESS OF INTERVENTIONS
Table IV summarizes the findings of the individual studies, categorized according to the results related to adiposity, dietary intake, knowledge of nutrition, PA and sedentary behavior. The statistical significance values (p-values) shown in interventions with a control group refer to the differences between these groups, while the p-values in interventions without a control group show the differences before and after the intervention.
Table IV. Results of individual studies grouped according to variables related to adiposity and secondary variables.
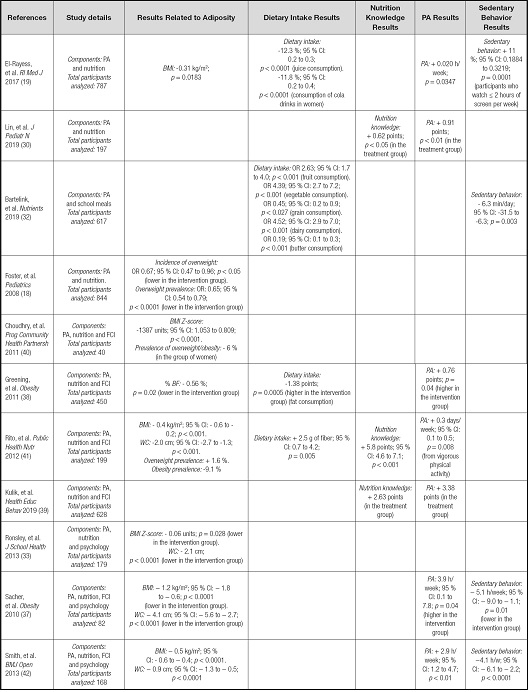
PA: physical activity; FCI: family-community involvement; BMI: body mass index; WC: waist circumference; % BF: percentage of body fat; CI: confidence interval.
Variables related to adiposity
Eight of 11 studies reported significant effects on at least one variable associated with adiposity (18,19,33,37,38,40-42). These changes occurred in one of two studies made up of physical activity and nutrition (19); in four of five interventions made up of PA, nutrition and FCI (18,38,40,41); in the only study of PA, nutrition and psychology (33), and in the two interventions that included PA, nutrition, FCI and psychology (37,42). Of the interventions lasting ≥ 6 months, five out of eight had a favorable effect on some adiposity variable (18,33,37,38,41) (Table IV).
Prevalence and incidence of overweight and/or obesity
Three of 11 studies reported a reduction in prevalences, one for overweight (18), another for obesity (41), and the third presented decreased for overweight/obesity joint (40). The three studies were made up of PA, nutrition and FCI, two of them lasted ≥ 6 months (18,41). The only intervention that achieved a reduction in the incidence of overweight had the aforementioned characteristics (18).
BMI/BMI Z-score
Six of 11 studies showed significant effects on BMI or BMI Z-score (19,33,37,40-42), three of them had a duration of ≥6 months (33,37,41). Such changes were mainly found in interventions that included PA, nutrition and FCI (40,41), and in those that included, in addition to the three previous elements, the component of psychology (37,42).
Body fat percentage
Of all the included studies, one reported a significant reduction in body fat percentage. This consisted of PA, nutrition and FCI and lasted ≥ 6 months (38).
Waist circumference
Four of 11 studies presented a reduction in waist circumference (33,37,41,42), three of them with a duration of six or more months (33,37,41). The interventions that were most effective for this variable were composed of PA, nutrition, FCI and psychology components (37,42).
Result in dietary intake
Four of 11 interventions presented a significant change in dietary intake (micro and macronutrients) (19,32,38,41); three of them with a duration equal to or greater than 6 months (32,38,41). The studies that achieved more consistent changes in this variable, specifically on macronutrients (fats and fiber), according to the components that integrated them were those of PA, nutrition and FCI (38,41).
Nutrition knowledge outcomes
Three of the total of the studies had significant improvements regarding nutrition knowledge (30,39,41). Two of them lasted 6 months or more and consisted of PA, nutrition and FCI components (39,41).
Physical activity results
Seven of 11 interventions reviewed showed favorable changes in physical activity (19,30,37-39,41,42), of which five lasted ≥ 6 months (30,37-39,41). The components of the interventions with the most consistent results were PA, nutrition, and FCI (38,39,41), followed by those that also included psychological aspect (37,42).
DISCUSSION
As a summary of the results, the narrative synthesis suggests that MLIPs integrated by PA, nutrition and FCI components are more effective in achieving changes in variables related to adiposity (prevalence and incidence of overweight and obesity) and in indicators of these conditions, specifically in BMI/BMI Z-score and fat percentage, in schoolchildren from vulnerable groups. In relation to the secondary variables dietary intake, knowledge of nutrition and physical activity, the interventions that include PA, nutrition and FCI also obtained better results.
Around 80 % of the interventions with components of PA, nutrition and FCI, had a duration of ≥ 6 months. This characteristic is favorable for achieving significant changes in the variables associated with adiposity (29). These interventions were also characterized for having been taught mostly (80 %) by teachers who received prior training, which is consistent with what has been reported in other studies (43-45).
The significant improvements in these interventions may be due to the fact that they actively involve parents, who have an essential influence on the acquisition and maintenance of healthy eating habits in children (46). Likewise, it has been described that parental control, attitudes and behavior are closely associated with childhood overweight and obesity (47). One study showed that parental monitoring of children's food choices has been shown to reduce non-nutritious food intake and total caloric intake (48). Therefore, the involvement of the family is an element that must be considered in the MLIP, especially in schoolchildren from vulnerable groups who are additionally affected by the social deficiencies of the parents.
The conjunction of interventions that promote physical activity and a balanced dietary intake confront the fundamental aspects related to the increase in overweight and obesity in schoolchildren, such as the characteristics of the diet, the level of PA and the degree of sedentary lifestyle (49), closely related to dynamic energy balance (50).
The interventions that, in addition to PA, nutrition and FCI, included a psychology component, achieved notable results by improving the BMI/BMI Z-score, waist circumference, PA and sedentary behavior. However, when designing and implementing MLIPs, it is sought not only that they be effective but also that they be efficient, that is, that the best results are achieved with the least amount of resources employed as possible (51). Thus, integrating one more component would entail the use of more physical, material and human resources; consequently, opting for the design of three components (PA, nutrition and FCI) would be more beneficial in all aspects, and would facilitate its replication in different environments, especially in those affected by poverty (51,52).
This is the first review of MLIPs in schoolchildren from vulnerable groups for the prevention, maintenance and remission of overweight and obesity, when evaluating indicators of adiposity. In the particular context of vulnerability that these children live in, a greater increase in the prevalences of the disease is observed compared to the rest of the population (12,21-23). Given the situation, the design and implementation of specific interventions is recommended (52), and the importance of knowing and understanding which interventions work best in these settings is highlighted.
The search strategy did not include gray literature, articles in a language other than English, and a publication date was established as of the year 2000. All the elements mentioned above can cause publication and language biases, and influence the representativeness of the articles that were selected for the review, in relation to the studies that have been performed.
The validity of the findings presented is a function of the methodological quality of the individual studies. Since the risk of bias assessment was not carried through for the different domains (design, performance and presentation of the results), suggested in the Cochrane manual for systematic reviews in interventions (53), it is not possible to classify the quality of the evidence for each study.
In conclusion, the review suggests that MLIPs are effective in preventing and treating overweight and obesity, finding that 73 % of the studies had significant improvements in at least one variable related to adiposity. The most successful intervention programs in schoolchildren from vulnerable groups were made up of nutrition, PA and FCI components, lasting 6 months onwards, and were delivered by trained teachers. The findings of this work should be considered with caution due to reported methodological limitations.