INTRODUCTION
In the last two decades, more attention has been focused on eating behaviors in men; however, research is still scarce, and men are systematically overlooked in this area. Research in men does not have the same proportion as in women, and men continue to be excluded from many studies (1).
Emotional eating (EE) represents a maladaptive eating behavior (2), which refers to an increased food intake in response to emotions, especially negative mood states, such as anxiety, frustration, sadness, and anger, among others. Emotional eating could be considered as eating with emotion-focused coping, which attempts to minimize, regulate, and prevent emotional tension, often related to difficulty in controlling the quality (food choice) and quantity of food intake (3,4). According to affective theory (5) and the five-way model proposed by Macht (6) about the bidirectional relationship between emotions and eating behavior, some individuals cannot recognize their hunger and satiety cues and confuse emotional needs and biological hunger.
Previous studies reported that women had higher scores of emotional eating than men and this behavior was associated with weight fluctuations, difficulties with weight loss or weight maintenance, binge eating, and depression symptoms (7,8). In the study by Van Strien et al. (4) it has been found that emotional eating acted as a mediator between depression and weight gain in women; however, no such mediation effect was found for men.
Studies have suggested that depression symptoms are related to eating behaviors, especially in women (4,9); nevertheless, there are contradictory findings with respect to their role in men (10,11). A study performed among United States college students by Turel et al. (12) reported no differences in depression scores between men at risk and not at risk of eating disorders.
Regarding depression symptoms and eating behaviors, according to the American Psychiatric Association (13) depression is frequently accompanied by appetite changes: decreased or increased appetite (atypical depression). Cognitive mechanisms that explain overeating in mood disorders may be a desire to achieve an instant reward and reduction of affective self-control (impulsive food choice, particularly for “comfort foods”, high in fat and sugar) (14,15). In previous studies, a mediation effect of emotional eating between depression and weight gain has been found (4,16).
The biological theoretical framework on eating behavior has been focused on neurobiological processes referred to dopamine systems: food represents a natural reward and gratification related to dopamine production that influences food selection towards high-energy foods (17). Furthermore, sugar consumption is associated with reduction of stress-induced cortisol and hippocampus activation, which is typically inhibited during acute stress (18). In studies on food cravings focused on carbohydrate consumption, it has also been found that this behavior was related to serotonin deficit; therefore, some people tend to overeat sweet food to improve mildly dysphoric mood (19-21).
Konttinen et al. (22) examined the association of emotional eating and depression symptoms with food choices in Finnish men and women, aged between 25 and 64. In men, emotional eating and depression symptoms were related to a higher body mass index, and emotional eating was associated to a higher consumption of sweet foods (frequency/week), as well as with the consumption of non-sweet energy-dense foods. In France, Camilleri et al. (23) studied associations among emotional eating, depression, and the consumption of energy-dense snack food in 7,378 men over 18 years old. However, there were no relationship between emotional eating and sweet foods intake (chocolate and cakes/biscuits/pastries) in men with depression symptoms. In a systematic review of 45 studies (24) on relationship between emotional eating, consumption of hyperpalatable energy-dense foods and nutritional status, it has been indicated that emotional eating had an association with greater consumption of energy-dense snacks, particularly sweet and high-fat foods, especially with relation to negative emotions. Additionally, a mediator effect of emotional eating between depression and weight gain has been reported (4,16); however, the studies have been mostly focused on women’ populations, and there is no information about mediating effect of emotional eating between depression and foods consumption.
In Mexico in recent decades, an “obesogenic environment” characterized by greater availability of high-energy foods and physical inactivity, factors related to weight gain, has been experienced widely. According to the National Survey of Health and Nutrition (NSHN) (25), the increasing prevalence of overweight/obesity in all age groups of the Mexican population has been linked to the consumption of sugary drinks, fried food, and fast food on a daily basis, as well as to a large proportion of high-energy food consumed away from home and decreased physical activity. It is worth considering that poor eating patterns acquired at a young age may persist into adulthood and lead to weight gain or other chronic diseases. The results of the Mexican NHNS reported that the prevalence of overweight or obesity (≥ 25 kg/m2) were quite high, 35.7 % in adolescent men and 73 % in those over 20 years of age; therefore, the identification of risk factors that contribute to unhealthy eating behavior is of great significance (25).
The current study aims to assess the associations among emotional eating, depression symptoms, and frequency of unhealthy food consumption in first-year Mexican college men. We hypothesized that depression symptoms are associated with high frequency of unhealthy food consumption and that this relationship is mediated by EE.
MATERIAL AND METHODS
STUDY POPULATION
A cross-sectional study was performed in a public university in Mexico City with first-year college men (n = 775, which represents 48.14 % from a total population of 1,610 men and women enrolled at the university) who participated in the 2017-year health survey that included anthropometry and online questionnaires. These questionnaires were applied for freshman students during the first week of trimester in the computer classrooms. Students who did not complete the questionnaires were excluded from the study (n = 11); therefore, 764 men were included for analysis. The response rate was 98.58 %.
ETHICS
This study was part of the institutional project “Healthy University: disordered eating behaviors related to mental health in young adults”. The questionnaire was completed anonymously, and the participants were assured of data confidentiality. The students participated on a voluntary basis, and they acknowledged informed consent on-line. This study has been carried out in accordance with the Code of Ethics of the World Medical Association, Declaration of Helsinki, Ethical Principles for Medical Research Involving Human Subjects. The University Review Board of Biological and Health Science approved the project and ethical aspects were revised (project approval date: session 1/17 February 2, 2017; project number 3450336).
INSTRUMENTS
Eating and Appraisal Due to Emotions and Stress Questionnaire (EADES)
To assess EE, the subscale Self-Efficacy in Emotion- and Stress-Related Eating (26), the Spanish-language version of the EADES was applied (Cronbach's alpha = 0.87) (27). In the present study, Cronbach's alpha was 0.91. The subscale consists of 12 items related to emotional and stress-related eating (e.g., I use food to cope with my emotions, I eat when I am upset with myself, I comfort myself with food, I eat when I am sad, I overeat when I am stressed, I feel out of control when I eat, it is hard for me to stop eating even though I feel full, among others). Participants responded to the questionnaire in accordance with their level of agreement on a scale from 1 to 5 from strongly disagree to strongly agree (the higher the score the more involvement in EE).
Center for Epidemiologic Studies Depression Scale (CES-D)
To identify depression symptoms, a Spanish-language version of the 20-item depression scale elaborated by the Center for Epidemiologic Studies (CES-D) was used, which was validated in non-clinical Mexican populations (28), with Cronbach's alpha = 0.83 in the student population (29). In the present study, Cronbach's alpha was 0.84. Likert-type items assessed the frequency of depressive symptomatology in the previous week, including depressed mood, feelings of guilt and worthlessness, psychomotor retardation and sleeping difficulties. A cut-off point of 16 was used to identify clinically significant depression symptoms (28). Prior psychological treatment was reported with a yes or no answer.
Food Frequency Questionnaire
The assessment of frequency of food consumption was based on the Food Frequency Questionnaire (30) and on dietary items from the NSHN (25). For the present study, foods classified as “not recommended for daily consumption” were analyzed (25). The carbohydrate-rich and/or energy-rich foods were categorized into four groups following the Mexican Center for Research in Nutrition and Health recommendations (30): fried food (e.g., potato chips, corn chips and tortilla chips, French fries, flour chicharron, and fried bananas, among others), sweet foods (cakes, cookies, pastries, sweets, chocolate, biscuits, sweet bread, among others), sweetened beverages (e.g., soft drinks, soda, sweetened ice-tea, natural and industrial juices), as well as fast food (hamburgers, fried chicken, pizza or sausages, hot dogs, white-bread sandwiches, among others). Frequency of food consumption was analyzed and measured in the number of days a week with the corresponding answers: less than once a week or once a week, two, three times a week, four or more times a week.
Anthropometry
Using the recommended techniques and procedures, a certified dietitian took body weight and height measurements (International Certification in Kinanthropometry, Isak Level 1).
A senior researcher supervised the anthropometric evaluation. Body weight and height were measured using a portable, electronic digital scale, equipped with a built-in stadiometer (SECA scale, model 813 and SECA stadiometer, model 213) with a precision of 0.1 kg and 0.1 cm, respectively.
Body mass index (BMI weight/height2) was calculated. Based on the World Health Organization (WHO) criteria, the cut-off point for being overweight was BMI ≥ 25 kg/m2, for being obese ≥ 30 kg/m2 and for being underweight < 18.5 kg/m2.
DATA ANALYSIS
The analysis for categorical variables was performed using Chi-squared test. A bivariate analysis (ANOVA and linear regression) was performed between EE and the following variables: depressive symptoms, psychological treatment, BMI, and frequency of food consumption. The Bonferroni post-hoc test was used for multiple comparisons. Statistical significance was set at p < 0.05.
A mediation analysis was conducted using EE as a mediator between depression symptoms and frequency of sweet food consumption. This analysis was performed using the Karlson, Holm and Breen (KHB) method for comparing estimated coefficients of two nested nonlinear probability models. Additionally, to determine the significance of each mediation path, the indirect effects were examined over one thousand bootstrap replications; a 95 % confidence interval (95 % CI) was reported. The statistical analysis was performed using the Stata V17.0 (Stata Corp, College Station Tx, USA, 2021) statistical package.
RESULTS
A total of 764 college men were evaluated, the mean age of 21.12 years (SD, 2.85), ranging from 18 to 30 years old. Table I presents the descriptive characteristics of the participants. The mean BMI was 24.04 (SD: 3.23); 34.56 % of college men were overweight or obese.
Table I. Distribution of college men according to the study variables (n = 764).

BMI: body mass index.
*Center for Epidemiologic Studies-Depression Scale (CES-D).
About one-fifth of them reported depression symptoms (20.42 %) and a similar proportion received psychological treatment (20.55 %). Regarding food consumption, the results revealed that the most common frequency of fried food consumption was twice a week (39.14 %) and of sweetened beverages three times a week (37.96 %). About half of the students (49.74 %) consumed fast food twice a week and 38.48 % of them sweet food three times a week. Consumption of sweetened beverages and sweet foods almost daily (≥ 4 times a week) was observed in 15.44 % and 10.86 %, respectively, of the participants.
The mean EE score was 23.98 (SD: 9.13). Students with depression symptoms (CES-D ≥ 16) presented a higher mean EE score, (27.63; SD: 9.13) than students with CES-D score < 16 (23.05; SD: 8.90; p < 0.001). Similar results were observed when comparing students with (mean EE score = 27.08; SD: 8.79) and without (mean EE score = 23.99; SD: 9.80) psychological treatment (p < 0.001). However, mean BMI was not associated with EE score (p = 0.396).
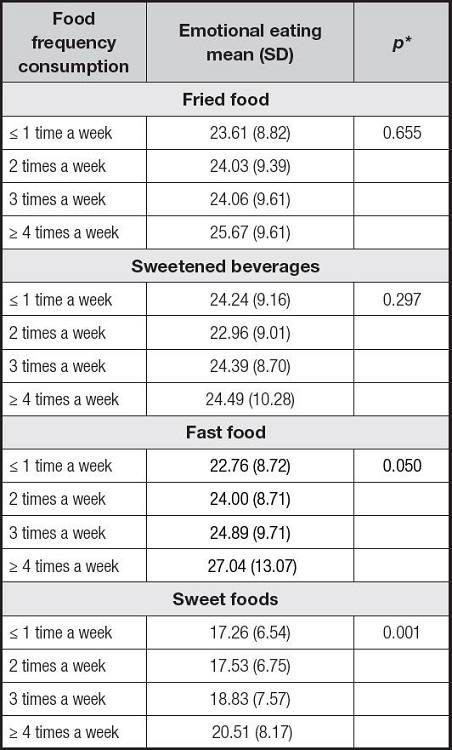
Table II presents the percentage of the students with depression symptoms by frequency of fried food, sweetened beverages, and sweet food consumption. Students with depression symptoms had a higher frequency (≥ 4 times a week) of fried food (p = 0.049); sweetened beverages (p = 0.050) and sweet food consumption (p = 0.005).
Table II. Depressive symptoms and frequency of fried food, sweetened beverages, fast food, and sweet foods consumption in college men.
*Cut-off value: four or more times per week.
†Depressive symptoms CES-D ≥ 16.
‡Column percentage.
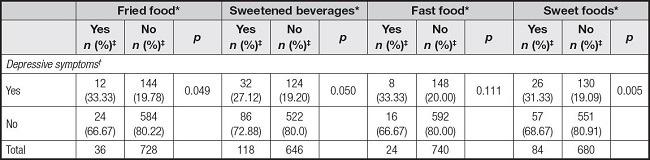
Regarding EE and frequency of food consumption (Table III), higher mean EE scores were found in students with a higher frequency of fast food (p = 0.050) and sweet foods consumption (p = 0.001). Particularly, students with frequency ≥ 4 times a week of sweet foods consumption had a score 20.51 (SD: 8.17), while their counterparts with frequency ≤ 1 time a week had a mean EE score 17.26 (SD: 6.54). Figure 1 presents students’ responses to three items of EE questionnaire, where a greater percentage difference by sweet foods consumption frequency was observed. Students with a higher consumption frequen- cy had a greater agreement of eating when they felt sad or stressed, or unable to control how much they ate.
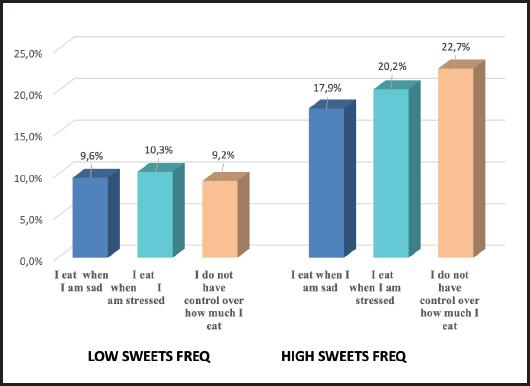
Figure 1. Percentage of participants who indicated agreement with three questions of the emotional eating scale by frequency of sweet food consumption (low and high).
Based on path analysis results, EE did not have a significant effect in the relationship between depression symptoms and frequency of fat, fried food, or sweetened beverages consumption. However, a significant effect of EE was observed between depression symptoms and frequency of sweet foods consumption; figure 2 depicts the path analysis results. Depression symptoms had a positive effect on EE (β1 = 3.54, CI: 2.28-4.79, p < 0.001) and, in turn, EE had a positive effect on sweet foods consumption (β2 = 0.04, CI: 0.01-0.07, p = 0.015).

Figure 2. Graphical representation of the path analysis. *Depression symptoms assessed with the Center for Epidemiologic Studies Depression Scale (CES-D), cut-off value CES-D ≥ 16. †Emotional eating (continuous variable) assessed with the Eating and Appraisal Due to Emotions and Stress Questionnaire (EADES). ‡Sweet foods consumption frequency cut-off value ≥ 4 times per week. §Coefficients, 95 % confidence interval (CI), unstandardized coefficients.
Table IV presents the results of the mediation analysis. The total effect of depression symptoms on frequency of sweet food consumption was significant and positive (0.71, p = 0.005). The direct (0.55, p = 0.035) and indirect (0.17, p = 0.011) effects were also significant and positive. According to this analysis, the indirect effect of EE represented 23.11 % of the total effect of depression symptoms on frequency of sweet food consumption.
DISCUSSION
The results of the present study support our hypothesis that depression symptoms are associated with high frequency of unhealthy food consumption and that this relationship is mediated by EE. Students with depression symptoms had a higher frequency of fried food, sweetened beverages, and sweet food consumption. Additionally, greater mean EE scores were observed among students with higher frequency of fast food and sweet foods consumption.
The results of our study indicated that the relationship between depression symptoms and frequency of sweet foods consumption was partially mediated by EE (23.11 % of the total effect). This suggests that EE plays a significant role in the relationship between depression symptoms (atypical depression with increased appetite) and frequency of sweet foods consumption, together with other mechanisms that intervene in this relationship (17,18), such as food selection and eating habits, parenting styles, personality, physical activity, and type of depression. Individuals with atypical depression are frequently prone to develop abnormal eating behavior, such as overeating in response to negative emotions, which may be considered as a coping mechanism to improve altered emotional state. It is common for these individuals to have difficulty in recognizing and managing their moods. Additionally, they confuse hunger and satiety with physiological distress and turn to food consumption as a means of coping with negative emotions. In this case, emotional eating may mediate the relationship between depressive symptoms and food choices (overconsumption of “comfort food”), which can consequently lead to weight gain or eating disorders among other health problems (4,16,31).
Our findings are in accordance with Ling et al. (32), who have reported that in the United States college men and women, between 18 and 25 years old, EE was positively related to sweet foods consumption. Regarding exclusively college men, in a qualitative study performed in the United States (33), it was found that boredom and anxiety were triggers for overeating sweet foods. Similarly, in a study of Finnish men, Konttinen et al. (22) have identified that emotional eating was associated with higher consumption of sweet foods, as well as non-sweet energy dense foods (pizza, hamburgers, French fries, sausages, and chips).
The results of the present study revealed that about a fifth of the study group reported depression symptoms (20.42 %). This finding proposes areas of future research to recognize how negative emotions may affect eating behavior in men, as well to identify young men at risk of developing eating disorders, weight gain in adulthood, and/or other unhealthy behaviors related to depression.
The association between depressive symptoms and EE reported herein is consistent with previous studies performed in college men. Sze et al. (34) have identified that EE was not uncommon among Chinese college men and mild depression was significantly associated with EE. However, in the United States, Turel et al. (12) have indicated that depression symptoms were not associated with risky eating behaviors in college men, in contrast to women. In the study by Mikolajczyk et al. (10), conducted in three countries (Germany, Poland, and Bulgaria) among first-year college students, there was no positive association between food consumption (i.e., fast-food, cakes, snacks, sweets) and stress and/or depressive symptoms among male students. These contradictory results, especially for men, may be explained by cultural and social factors. According to the Mexican National Health and Nutrition Survey (25), sugar consumption is very high, and this eating habit is determined to a large extent by social and environmental factors (35). Mexico is one of the highest sugar-consuming nations in the world (36). Excessive sugar intake is a risk factor for metabolic and cardiovascular diseases and has an adverse effect on the gut microbial ecosystem. The Western diet, characterized by excessive consumption of saturated fats and added sugars, can affect the composition and balance of the gut microbiota, leading to chronic inflammation and gut dysbiosis (37). Brain-gut axis function is affected by the microbiota of the gastrointestinal tract, which, in turn, is influenced by food consumption. It has been established that depression is closely linked to this axis. It is crucial to improve intestinal dysbiosis because depression, food consumption, and intestinal function are related in a complex way (38).
The sex difference in the prevalence of mood or anxiety disorders (39), and the fact that men and women express their emotional problems according to traditional gender stereotypes (40), may affect the way in which EE mediates the relationship between depressive symptoms and the frequency of sweet food consumption. In the present study, BMI was not associated with emotional eating score and depression symptoms in first-year college men. This may be explained by the young age of the participants (most of them had 18-19 years old) and their physical activity, which is common in college men.
Among the limitations of the study was its cross-sectional design, which does not allow causal interpretation of the associations identified by the statistical models. Additionally, we applied self-reported questionnaires, an assessment method which is susceptible to response bias. However, the questionnaire was completed anonymously, and the participants were assured of data confidentiality.
The questionnaires applied in the sample for evaluating EE and depression only identified tendencies to risky behaviors, as well as symptoms of depression. These questionnaires do not diagnose any clinical condition; nevertheless, the instruments applied have been previously validated in different population groups including young Mexican adults and have been frequently used to identify unhealthy behaviors.
Further research is required to assess the role of EE in the relationship between depression symptoms and food consumption in men, as well as to identify the underlying factors of “obesogenic” environment, which may help develop targeted and coordinated prevention programs in depression and eating disorders.
CONCLUSIONS
A significant number of college men reported depression symptoms that represent a challenge for clinical practitioners and the public health sector considering the increased incidence, particularly in young population groups. The relationship between depression symptoms and frequency of sweet foods consumption was partially mediated by EE. Therefore, it is important to understand how men experience and perceive their eating behaviors, which could be useful in enhancing awareness and self-regulation in these situations. In addition, it can help develop effective targeted programs in prevention or treatment of obesity and eating disorders in this population.