INTRODUCTION
Chronic kidney disease has become a public health problem for mankind in the 21st century. Relevant surveys have shown that 20 % of chronic kidney disease cases will evolve to end-stage renal disease (1,2). Maintenance hemodialysis (MHD) as renal replacement therapy for end-stage renal disease is the main approach to maintain patients alive. Although hemodialysis can expel toxins from the body, it also leads to loss of a variety of nutrients, resulting in malnutrition and various complications (3). Sarcopenia is characterized by loss of skeletal muscle mass, lowered strength, and reduced function accompanied by symptoms such as weight loss, weakness, easy falling, and motion difficulty, leading to a decline in quality of life. Moreover, it will increase the risk of cardiovascular complications, and increase the mortality of MHD patients. Previous investigations have shown that the incidence of sarcopenia in MHD is between 4 % and 63 %, and sarcopenia is a predictive risk factor for death in MHD patients (4,5). Lee et al (6) pointed out that the incidence of sarcopenia is related to malnutrition. MHD patients with sarcopenia have a single diet, insufficient protein intake, and reduced blood phosphorus and extracellular water ratio. Diet management is an effective way to prevent sarcopenia in MHD patients (7). The trans-theoretical model (TTM) believes that individual behavior change involves a gradual and continuous process. By formulating targeted nursing measures according to the characteristics of the behavior change process, individual behavior can be effectively changed. TTM-based diet nursing focuses on diet needs and the diet change process, featuring pertinence and timeliness. In this study, MHD patients received TTM-based diet nursing, which is reported as follows.
PATIENTS AND METHODS
SAMPLE ESTIMATION
The primary endpoint of this study was the incidence of sarcopenia, which was predicted to be 30 % in the control group and 9 % in the intrevention group based on the pilot study. With a two-sided α value of 0.05 and a power of 90 %, minimum sample size was 140 using the PASS15 software. Considering a 10 % dropout rate, 156 cases were finally selected.
RESEARCH SUBJECTS
The clinical data of 243 MHD patients admitted to our hospital from January 2019 to August 2020 were retrospectively analyzed. Inclusion criteria: ① Age ≥ 18 years, diagnosed with renal failure and MHD; ② Regular dialysis time ≥ 3 months; ③ Liver, kidney, heart and other organs were free from substantial lesions; ④ No coagulation, hemolysis dysfunction; ⑤ No gastrointestinal malignancy; ⑥ The principle of informed consent was followed. Exclusion criteria: ① History of kidney transplantation; ② Reading and communication disorders; ③ Complicated with mental disease. Using the SPSS 22.0 software and PSM method, patients who received routine care and dietary guidance, as well as patients who received a TTM-based dietary care intervention were matched 1:1. The matching variables included gender, age, education time, dialysis age, body mass index, underlying disease, annual income, and malnutrition. Finally, 82 patients were included in the control group and 80 patients in the observation group, respectively. This study was approved by the Ethics Committee of our hospital.
METHODS
Intervention methods in the control group
Routine nursing and diet guidance were given. The nurse in charge instructed the patients on hemodialysis-related principles and treatment ways. By referring to the relevant literature and consulting nutritionists, clinicians, a “Diet Management Handbook for Maintenance Hemodialysis Patients” was prepared. The nurse in charge explained the importance of diet management. Psychological counseling was given for patients with anxiety and depression to enhance their confidence in treatment. The intervention was performed once every 2 weeks, 30 min each time for 6 months.
Intervention methods in the experimental group
Establishment of a diet intervention team. On the basis of the control group, a TTM-based diet nursing intervention was given. The intervention team consisted of 1 clinician, 1 head nurse, 5 responsible nurses, and 1 dietitian. The team members were organized to learn the “Diet Management Handbook for Maintenance Hemodialysis Patients”, TTM theory, and other knowledge. Based on the TTM theory, the staged diet intervention program was determined. The duration of the intervention was 6 months.
Stage 1: preintention stage, that is, the patient is not on diet management and does not plan to start diet management in the future. a) Objective and content: to evaluate the patients' current awareness of diet management, to improve their awareness of diet management, so that patients change from unintentional stage to intentional stage. b) Intervention measures: ① Invite dietitians to explain the importance of diet management during hemodialysis, emphasize the possible good effects of diet management. The explanation lasted 30 min; ② Establish a WeChat group. Patients can communicate with doctors and nurses in the WeChat group when they have questions about diet-related matters. At the same time, use the WeChat group to explain diet-related knowledge. The management started in the first week for a total of 3 times, 30 min each time.
Stage 2: intentional stage, that is, the patient has planned to continue with diet management, but has not determined the specific plan. a) Objective and content: make patients understand the importance of diet management, and point out the possible harm of poor diet. b) Intervention measures: distribute the “Diet Management Handbook for Maintenance Hemodialysis Patients” for concentrated learning, enumerate the cases of good recovery due to diet management to inspire patients' confidence. c) Time and frequency: The management started in the second week, 3 times a week, 40 min each time.
Stage 3: preparation stage, that is, patients can follow the doctor's advice occasionally, but have not formed a regular diet. a) Objective and content: The responsible nurse analyzed the patients' skeletal muscle mass index (SMI), assessed whether sarcopenia was present, formulated detailed diet management methods, and informed the patients of detailed intake standards of protein, sodium, calcium, phosphorus and potassium. b) Intervention measures: determine the periodic diet intervention plan, and perform related knowledge education through concentrated health education and WeChat support.
Stage 4: action stage, that is, diet management starts. a) Objective and content: Develop behavioral change goals for patients, including improving diet management behavior, nutritional status, and improving individualized diet management programs. b) Intervention measures: Mainly through peer support education, MHD patients with excellent diet management behavior were invited as guest stars to team with patients in the action stage, teach them by examples, assist and guide action stage patients in positive behavior changes. The management started in the 5th-8th week, 5 times a week.
Stage 5: maintenance stage, that is, diet management is further carried out in this stage. a) Objective and content: Evaluate patients' diet management behavior once every 4 weeks, affirm patients with good eating behavior change, encourage patients to say problems in the diet management process, analyze existing problems, and evaluate whether patients have returned to previous stages. b) Intervention measure: regular follow-up for 9-24 weeks. The patients were followed up once a week by WeChat, once every 2 weeks by telephone, once every 4 weeks by clinic, and once every 12 and 24 weeks by family visits.
OBSERVATION INDEXES
Incidence of sarcopenia and body composition analysis: skeletal muscle mass index (SMI) was measured by bioelectrical impedance analysis (BIA) according to the diagnostic criteria of the “Asian Working Group for Sarcopenia” (AWGS) before and after the intervention. If SMI was < 7.0 for males, < 5.7 for females, handgrip strength (HGS) was< 26 kg for males, < 18 kg for females, or/and daily gait speed < 0.8 m/s, sarcopenia can be confirmed (8). Body composition analysis was performed by body composition analyzer to analyze body water (TBF), extracellular fluid (ECF), somatic cell mass, and calculate extracellular water ratio (ECF/TBF).
Diet management behavior: the “Renal Adherence Behaviour Questionnaire” (RABQ) developed by Rushe et al. was used for evaluation before and after the intervention (9). A total of 25 items were included in 5 dimensions and a higher score means a higher adherence to diet management.
Nutritional status: before and after the intervention, the subjective global assessment (SGA) (10) was used for evaluation, including 7 parts.
Nutritional serum index: before and after the intervention, 3 ml fasting venous blood were collected and centrifuged for 10 min with a radius of 3 cm. The supernatant was collected and the contents of albumin (ALB), prealbumin (PA) and transferrin (TRF) were detected using a Hitachi automatic biochemical analyzer.
Anthropometric index: midarm circumference (MAC), mid-arm muscle circumference (MAMC) and triceps skinfolds thickness (TSF) were measured before and after the intervention, respectively.
Quality of life: the SF-36 concise health scale was used to evaluate quality of life. The scale included 8 dimensions. A higher total score means better quality of life.
Follow-up: after the intervention, the patients were followed up for 1 year (telephone or outpatient follow-up once every 3 months), and the follow-up ended at the patient demise or in February 2022. The 1-year survival rate of the two groups was calculated and compared after the end of follow-up.
STATISTICAL PROCESSING
The SPSS 22.0 statistical software was used for processing. Enumeration data were described by the number of cases and incidence (%), and the χ2 test or Fisher's exact probability was used. Rank sum test was used for rank data. Measurement data were described by (mean ± SD), median and quartile, and two independent sample t-test or paired sample t-test or rank sum test were adopted. A Kaplan-Meier survival curve was used to analyze the 1-year survival rate of the two groups, and a log-rank test was performed. A p < 0.05 suggests a statistically significant difference.
RESULTS
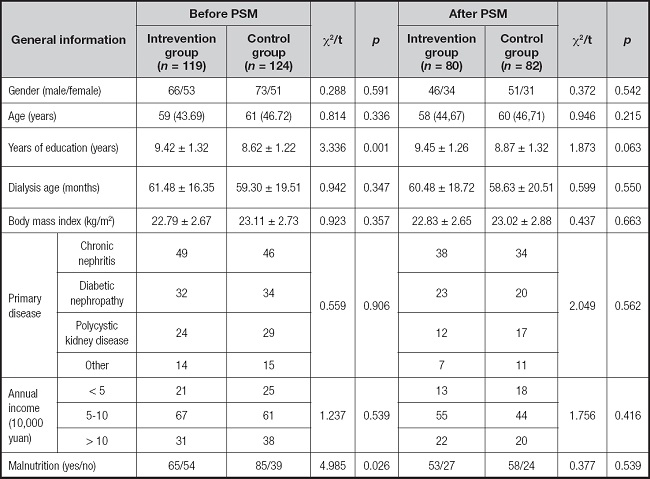
COMPARISON OF GENERAL DATA BEFORE AND AFTER PSM BETWEEN THE TWO GROUPS
Before PSM, the education time of the intervention group was significantly longer than that of the control group (p < 0.05), and the incidence of malnutrition was significantly lower than that of the control group (p < 0.05). There was no significant difference in all general data after PSM (p > 0.05). The general data before and after the intervention in the two groups of PSM are shown in table I.
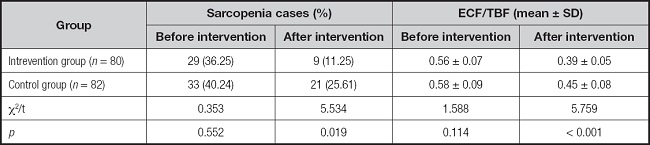
COMPARISON OF INCIDENCE OF SARCOPENIA AND ECF/TBF BETWEEN THE TWO GROUPS
Before the intervention, there was no statistically significant difference in the incidence of sarcopenia, and ECF/TBF between the two groups (p > 0.05). After the intervention, the incidence of sarcopenia and ECF/TBF were decreased in both groups, and the intervention group had a lower value than the control group (p < 0.05), as shown in table II.
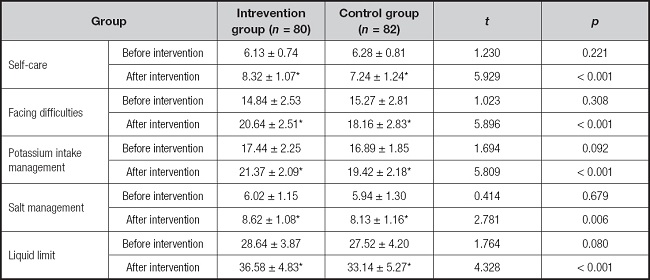
COMPARISON OF DIET MANAGEMENT BEHAVIOR BETWEEN THE TWO GROUPS
Before the intervention, there was no statistically significant difference in diet management behavior between the two groups (p > 0.05). After the intervention, the scores of self-care, difficulty handling, potassium intake management, salt intake management, and liquid limits were higher in group 2, with scores higher in the intervention group than in the control group (p < 0.05), as shown in table III.
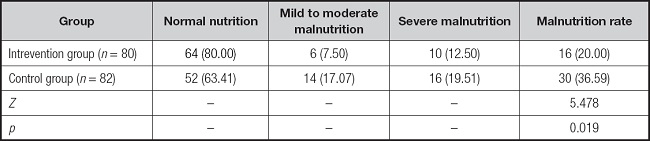
COMPARISON OF NUTRITIONAL STATUS BETWEEN THE TWO GROUPS AFTER THE INTERVENTION
The intervention group had lower malnutrition rates than the control group after the intervention (p < 0.05), as shown in table IV.
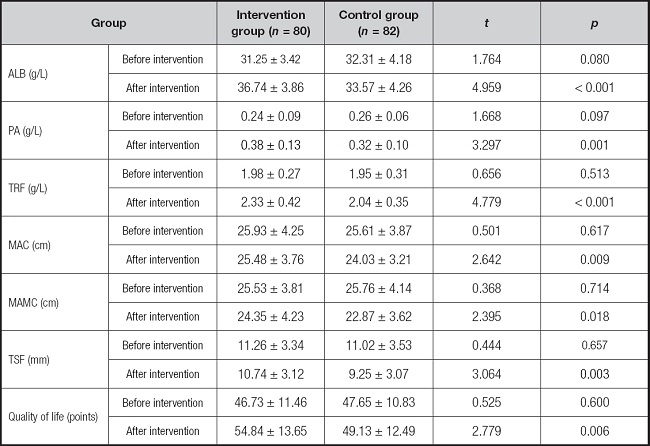
COMPARISON OF NUTRITIONAL SERUM INDEXES, ANTHROPOMETRIC INDEXES AND QUALITY OF LIFE BETWEEN THE TWO GROUPS
Before the intervention, there was no statistically significant difference in nutritional serum indexes, anthropometric indexes, and quality of life between the two groups (p > 0.05). After the intervention, the intervention group had higher contents of serum ALB, PA, TRF and quality of life scores, and the content was higher in the intervention group than in the control group (p < 0.05). Meanwhile, the intrevention group had significantly higher MAC, MAMC and TSF than the control group (p < 0.05), as shown in table V.
COMPARISON OF 1-YEAR SURVIVAL RATE BETWEEN THE TWO GROUPS
The Kaplan-Meier survival curve showed that the 1-year survival rate of the intervention group was 95.00 % (76/80), which was higher than the 85.37 % (70/82) of the control group. Log-rank χ2 = 4.251, p = 0.039, as shown in figure 1.
DISCUSSION
BASIS OF DIET MANAGEMENT IN MHD PATIENTS
MHD needs long-term adherence, requiring patients to follow their doctor's advice, and regularly seek hospital treatment. However, due to prolonged survival time, there are many complications such as cardiovascular complications, physical deterioration, malnutrition. Sarcopenia, an aging disease of skeletal muscle associated with aging, has a high incidence in renal function diseases. Previous investigations have shown that sarcopenia patients had lower protein and total energy than non-sarcopenia patients (11). Due to the loss of large amounts of nutrients in MHD patients, lack of diet management will affect the nutritional status of patients (12). It has been reported that insufficient energy intake can lead to reduced mitochondrial energy metabolism of muscle fibers, which in the long run can lead to negative nitrogen balance and muscle atrophy (13). Therefore, MHD patients need to strengthen diet management, get sufficient intake of energy and calories, and promote muscle protein synthesis. In the past, in the routine diet management of hemodialysis patients, the medical staff carried out knowledge “cramming” education to instruct patients on diet precautions, which lacked specificity and had a poor intervention effect. TTM is the nursing intervention theory for behavioral stage, which integrates different theories of education, nutrition, psychology, etc., evaluates patients' needs, and gives targeted support nursing to guarantee individualized and effective intervention measures. Some scholars have pointed out (14) that TTM-based diet nursing can improve the diet and exercise habits of patients with chronic diseases, thereby improving the nutritional status of MHD patients (14).
APPLICATION EFFECT OF A TTM-BASED DIET NURSING INTERVENTION IN MHD PATIENTS
This study showed that the scores of self-care, difficulty handling, potassium intake management, salt intake management, liquid limit, incidence of malnutrition, and sarcopenia were lower in the intervention group than in the control group. It suggests that a TTM-based diet nursing intervention can improve patient diet management behavior and reduce the incidence of malnutrition and sarcopenia. A TTM-based diet nursing intervention takes the current diet management behavior as the breakthrough point, and diet management handbook as the blueprint; divides diet behavior changes into preintention stage, intentional stage, preparation stage, action stage, and maintenance stage. The preintention stage attaches importance to cultivating patient awareness of diet management, makes them aware of deficiencies in self diet management to inspire intrinsic motivation for self-change. In the intentional stage, the awareness and behavior of diet management are strengthened. In the preparation stage, detailed behavior management methods are developed to determine the standard of action for patients. In the action stage and maintenance stage, peer support education and WeChat support are given to supervise patients and assist in diet management. The results achieved by patients should be affirmed, so as to enhance patient self-confidence in diet behavior change. The diet plan is specific and detailed, clarifying specific intake values of daily calories and high-quality protein. Improving caloric and protein intake is the main measure to manage malnutrition in MHD patients, while malnutrition is a risk factor for MHD patients with sarcopenia. Protein and caloric supplementation can improve muscle strength and correct sarcopenia (15).
The diagnosis of sarcopenia was made by BIA testing, with nutrient index ECF/TBF being highly analyzable. ECF/TBF is an important evaluation index of dry weight in MHD patients, and should be lower than 0.395 if there are complications of diabetes or hypoproteinemia (16). After the intervention in this study, the ECF/TBF value was lower in the intervention group than in the control group, which was nearer the ideal dry weight. Serum ALB, PA and TRF are effective indexes for nutritional status evaluation. This study showed that the serum ALB, PA and TRF were higher in the intervention group than in the control group, and the anthropometric indexes MAC, MAMC and TSF were higher in the intervention group than in the control group. It suggests that a TTM-based diet nursing intervention should fully take into account the nursing needs of MHD patients at different stages of behavior change, and help patients gradually form good eating habits and improve self-management ability through continuous and step-by-step intensive diet behavior management, thereby improving nutritional status and reducing the incidence of sarcopenia.
After the intervention, the quality of life score and 1-year survival rate were higher in the intervention group than in the control group. Sarcopenia is one primary factor leading to lower quality of life in MHD patients (17). A TTM-based diet nursing intervention can exercise a variety of nursing intervention modes according to the different stages of patient diet behavior change, so as to optimize the diet management effect. WeChat features immediacy and interaction, which can enable timely communication between nurses and patients, and the sent nursing information can be consulted by patients at any time. Peer support education can promote the formation of positive imitation behavior in MHD patients through demonstration effect. Family support can make patients feel cared for and valued, which can improve their psychological state, and facilitate the supervision of patient behavior change. Previous studies have shown (18) that a TTM-based nursing intervention can reduce blood potassium intake and effectively improve diet behavior (18). With correct and positive diet behavior construction, patients can access a more adequate nutrition, thereby reducing the incidence of malnutrition, preventing sarcopenia, and improving quality of life and the survival rate.
In conclusion, a TTM-based diet nursing intervention can help improve diet management behavior of MHD patients, prevent malnutrition, reduce the incidence of sarcopenia, and improve their quality of life and survival rate. However, there are still some limitations. For example, if the cases from only one hospital are collected, the homogeneity of the included population is relatively high, which may affect the extrapolation of study results. And due to the short intervention time in this study, it is impossible to observe the long-term effect of a TTM-based diet nursing intervention in the diet management of MHD patients. In the later stage, the intervention and follow-up time can be conducted in a multicenter study and further extended, the sample size can be enlarged, and continuous guidance can be provided for patient diet management with the help of mobile health care.