INTRODUCTION
Hepatobiliary and pancreatic malignancies include hepatocellular carcinoma and gallbladder, bile duct and pancreas cancers (1). The prevalence of malnutrition in patients with gastrointestinal malignancies ranges between 45 % and 80 %, and is higher than that of patients with other tumours (2,3). The incidence of malnutrition in hepatobiliary and pancreatic malignancies, which are included within the gastrointestinal malignancies, is between 2.7 % and 36.3 % (4). Patients with malignant tumours are prone to malnutrition due to the high metabolism caused by rapid cancer growth that constantly consumes nutrients from the body (5). The trauma caused by surgery aggravates the state of malnutrition, leading to a long postoperative recovery time and an increase in complications, seriously affecting survival time and quality of life (4).
Studies have shown that assessing patient nutritional status (protein energy malnutrition) with hepatobiliary and pancreatic malignancies is an important diagnostic and treatment tool for providing reasonable nutritional support (6). Although there is no gold standard for malnutrition assessment, many nutritional screening tools are commonly used in clinical practice (7). The Patient-Generated Subjective Global Assessment (PG-SGA) is a globally accepted tool for evaluating cancer patient nutritional status (8,9). Nevertheless, the PG-SGA is often deemed excessively time-consuming and challenging to comprehend for medical staff (10). Meanwhile, the Global Leadership Initiative on Malnutrition (GLIM) criteria, published in 2019, have been increasingly recognised for diagnosing malnutrition in clinical settings (11). Recent studies have demonstrated the applicability and reliability of the GLIM criteria in diagnosing malnutrition in various types of cancer, including lung and gastric cancer (12-14). Interestingly, the GLIM criteria define a lower prevalence of malnutrition in patients with hepatobiliary and pancreatic diseases compared with the PG-SGA (14). However, agreement between the GLIM criteria and PG-SGA in hospitalised patients undergoing hepatobiliary-pancreatic surgery remains unexplored.
In this study, the GLIM criteria and PG-SGA were chosen to assess the prevalence of malnutrition and the nutritional status of patients undergoing surgery for hepatobiliary and pancreatic malignancies, and a comprehensive comparison was carried out to select the most suitable nutritional assessment tool for clinical use.
MATERIALS AND METHODS
PARTICIPANTS
Patients attending a tertiary city hospital between November 1, 2019 and August 1, 2020 to undergo surgery for hepatobiliary and pancreatic malignancies were selected as the population for this study. The inclusion criteria were as follows: 1) patients with hepatobiliary and pancreatic malignancies diagnosed and pathologically confirmed; 2) patients aged over 18 years with indications for malignant tumours and opting to undergo hepatobiliary and pancreatic surgery for them; 3) patients who were conscious and had the ability to communicate clearly; and 4) patients who were willing to participate in this study and gave informed consent. The exclusion criteria were as follows: 1) patients with critical conditions that were difficult to assess; 2) patients with unknown diagnoses and advanced malignancy; 3) patients with malnutrition due to other reasons, such as cirrhosis or pancreatitis; and 4) patients receiving enteral nutritional support before surgery. This study was approved by the Ethics Committee of the First Affiliated Hospital of Ningbo University (ethical batch number: 2020R306), and all patients provided written informed consent before participating in the study. The study was conducted in accordance with the principles of the Declaration of Helsinki.
Using the cross-sectional survey sample size estimation formula N = Z2 × (1 − P) / (ε2 × P), where ε represents the desired accuracy as a percentage of the expected incidence rate, and P represents the expected incidence rate, the study’s required sample size was determined. According to relevant literature, the nutritional incidence rate for gastrointestinal malignancies is approximately 70 %, with P equal to 70 %. With a confidence level of 90 %, Z is 1.64. Given that the true population rate is within 10 %, ε is set to 10 %. Therefore, n = 1.642 × (1 − 0.7) / (0.122 × 0.7), indicating that a sample size of 115 participants is required for this research.
RESEARCH METHODOLOGY
General patient information was collected within 48 h of admission by reviewing the patients’ medical records and having face-to-face meetings with them to obtain their medical histories. A qualified nutritionist assessed the patients 1 day before their scheduled surgeries, using the GLIM criteria and PG-SGA. The nutritional indicators used were body mass index (BMI), upper-arm circumference (AC) and triceps skinfold thickness (TSF). Laboratory tests were conducted for haemoglobin (Hb), serum albumin (ALB) and serum pre-albumin (PA).
Global Leadership Initiative on Malnutrition assessment
The GLIM assessment consists of two steps: malnutrition diagnosis and grading of the severity of the malnutrition (15). The diagnosis of malnutrition involves various criteria. Here, the manifestation criteria included: 1) weight loss > 5 % in the past 6 months or > 10 % over 6 months; 2) aged < 70 years with a BMI of < 18.5 kg/m2 or aged > 70 years with a BMI of < 20 kg/m2; 3) mild to moderate muscle loss (i.e. calf circumference ≤ 30 cm in men or ≤ 29 cm in women); and 4) severe muscle loss. If a patient had a positive score for 1 to 3 of the above indicators, they were given 1 point. The aetiological criteria included: 1) energy intake ≤ 50 % for > 1 week or reduced energy intake > 2 weeks; and 2) the presence of any chronic gastrointestinal disease (affecting the digestion and absorption of food) or acute illness/injury or inflammatory state associated with chronic disease. If one or two of the above indicators were positive, the patient was given 1 point. The manifestation criteria score plus the aetiological criteria score could result in a maximum score of 2. A score of 2 was assessed as malnutrition, while a score of 0 or 1 was considered absence of malnutrition.
Malnutrition severity was graded according to various performance indicators: 1) moderate malnutrition: weight loss of 5 %-10 % in the last 6 months or 10 %-20 % in more than 6 months, a BMI loss of < 20 kg/m2 in patients aged < 70 years or < 22 kg/m2 in patients aged > 70 years and a calf muscle circumference of < 30 cm in men and < 29 cm in women; and 2) severe malnutrition: weight loss > 10 % in the last 6 months or > 20 % in more than 6 months, a BMI loss of < 18.5 kg/m2 in patients aged < 70 years or < 20 kg/m2 in patients aged > 70 years and a calf muscle circumference of < 27 cm in men and < 26 cm in women.
Patient-Generated Subjective Global Assessment rating
The PG-SGA is designed for the nutritional assessment of oncology patients based on the subjective global assessment. The main evaluation of the PG-SGA consists of two parts, the patient’s subjective assessment and the healthcare worker’s assessment, which includes eight aspects: weight, eating status, symptoms, activity and physical fitness, weight loss, the relationship between disease and nutritional needs, metabolic stress status and physical examination (15).
The patient completed the first part of the PG-SGA, recording their weight, eating status, physical fitness and symptoms and activity. Points for weight and symptoms were cumulative, and points for eating status and activity and physical fitness were based on the highest score obtained from patient verification. The healthcare worker assessed the second part. 1) Weight loss was scored using January’s weight data or, if those data were unavailable, the weight data from the last 6 months. An additional point was added if there had been some weight loss in the previous 2 weeks. 2) The relationship between disease and nutritional requirements was recorded if the patient had cancer, acquired immunodeficiency syndrome, pulmonary or cardiac cachexia, a decubitus ulcer, an open wound or fistula, trauma or was > 65 years, with 1 point for each condition. 3) Metabolic stress was assessed based on three factors: fever, duration of fever and glucocorticoid dosage. One point was given for mild stress, 2 for moderate stress and 3 for severe stress. 4) A physical examination assessed mainly fat, muscle and body fluids. Points were given depending on the degree of effort, with 0 points given for no exertion, 1 for mild exertion, 2 for moderate exertion and 3 for severe exertion. Finally, all the scores were added for a measurement evaluation, and a plan was developed based on the scores. A score of 0 or 1 on scale A indicated good nutrition, a score of 2-8 on scale B indicated uncertain or moderate malnutrition and a score of 9 or higher on scale C indicated severe malnutrition.
All diagnoses were made individually by two specialist dietitians, and where there was disagreement, the final diagnosis was discussed. Each patient was assessed for malnutrition using both methods.
STATISTICAL ANALYSIS
The statistical analysis was conducted using SPSS 19.0 software. The measurement data were expressed as mean and standard deviation, and the data were tested for normality using the Shapiro-Wilk test. Two independent sample t-tests were used to compare continuous variables with a normal distribution. The Mann-Whitney U-test was used for comparing continuous variables with a non-normal distribution, and count data were tested using the chi-square test. The correlation analysis was carried out using Spearman’s rank correlation coefficient, and the consistency of different tools was analysed using Cohen’s kappa coefficient. Statistically, p < 0.05 indicated a statistically significant difference, and p < 0.01 indicated a highly significant difference.
RESULTS
BASIC INFORMATION ON THE STUDY POPULATION
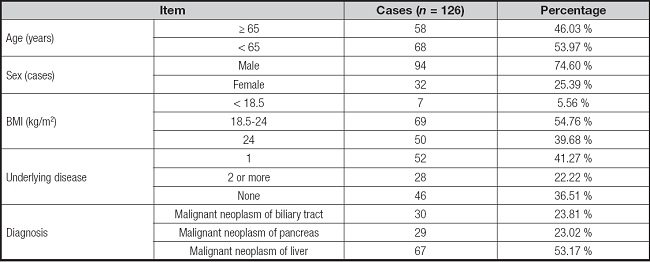
This study included 126 patients with perioperative hepatobiliary and pancreatic surgical malignancies. The patient’s age was ≥ 65 years in 58 cases and < 65 years in 68 cases. Ninety-four patients were men, and 32 patients were women. The patients’ BMI was < 18.5 kg/m2 in 7 cases (5.6 %), 18.5-24 kg/m2 in 69 cases (54.8 %) and > 24 kg/m2 in 50 cases (39.7 %). There was one underlying disease present in 52 cases (41.3 %), two or more underlying diseases in 28 cases (22.2 %), and no underlying disease in 46 cases (36.5 %). As table I shows, there were malignant tumours in the biliary tract in 30 cases (23.8 %), malig- nant tumours in the pancreas in 29 cases (23.0 %) and ma- lignant tumours in the liver in 67 cases (53.2 %).
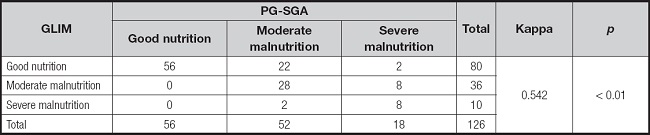
ANALYSIS OF CONSISTENCY BETWEEN THE NUTRITIONAL RATINGS OF THE TWO TOOLS
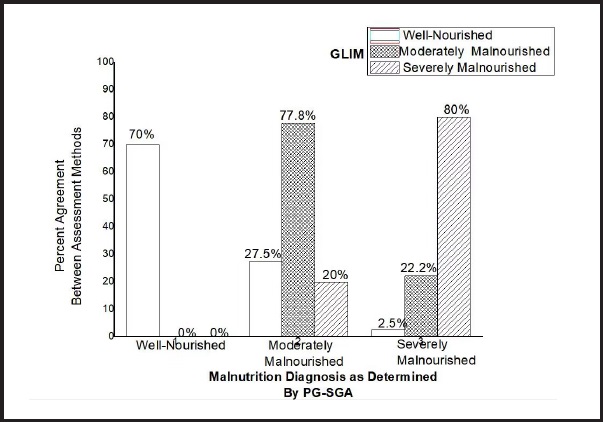
The GLIM assessment showed that 80 patients were well-nourished (63.5 %), 36 patients were moderately malnourished (28.6 %) and 10 patients were severely malnourished (7.9 %) (Fig. 1). The PG-SGA assessment showed that 56 patients were well-nourished (44.4 %), 52 patients were moderately malnourished (41.3 %) and 18 patients were severely malnourished (14.3 %) (Table II). The chi-squared test showed a kappa value of 0.542 (95 % confidence interval (CI), 0.424-0.672, p < 0.01), indicating a difference between the tools’ ratings.
Seventy percent of the patients diagnosed as well-nourished by the PG-SGA were found to be well-nourished on the GLIM scale. In addition, 77.8 % of the patients diagnosed as moderately malnourished by the PG-SGA were diagnosed as moderately malnourished according to the GLIM criteria, while 20 % were diagnosed as severely malnourished and 27.5 % were diagnosed as well-nourished. Furthermore, when the PG-SGA and the GLIM criteria were combined, severe malnutrition was diagnosed in 80 % of the participants, while the GLIM diagnosed good nutrition in 2.5 % and moderate nutrition in 22.2 %. This further suggests consistency in diagnosis between the PG-SGA and the GLIM criteria.
COMPARISON OF THE SENSITIVITY AND SPECIFICITY OF THE TWO ASSESSMENT TOOLS
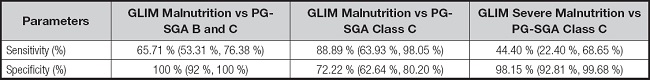
The sensitivity and specificity of the GLIM criteria versus those of the PG-SGA were calculated. An analysis of the GLIM’s and the PG-SGA’s diagnoses of malnutrition showed that the sensitivity rate of 65.7 % (95 % CI: 53.3 %-76.4 %) was moderate, and the specificity rate of 100 % (95 % CI: 92 %-100 %) was good. For the diagnosis of malnutrition, the GLIM criteria, with a sensitivity distribution of 88.9 % (95 % CI: 63.9 %-98.1 %), showed good sensitivity compared with the PG-SGA grade C, which had moderate specificity at 72.2 % (95 % CI: 62.6 %-80.2 %). When the GLIM diagnosis of severe malnutrition was compared to the PG-SGA diagnosis of grade C malnutrition, the specificity was good at 98.2 % (95 % CI: 92.8 %-99.7 %), the sensitivity decreased to 44.4 % (95 % CI: 22.4 %-68.7 %) (Table III).
CORRELATION BETWEEN ASSESSMENT OF MALNUTRITION AND VARIOUS NUTRITIONAL INDICATORS BY THE TWO TOOLS
The GLIM criteria classified 80 participants as well-nourished and 46 participants as malnourished. When comparing the nutritional status groups based on GLIM, statistically significant differences in the nutritional indicators, including ALB, PA, calf circumference, AC, TSF and PG-SGA scores, were observed (p < 0.05), except for Hb (Table IV).
Table IV. Comparison of GLIM and PG-SGA assessment of malnutrition with various one-way indicators.
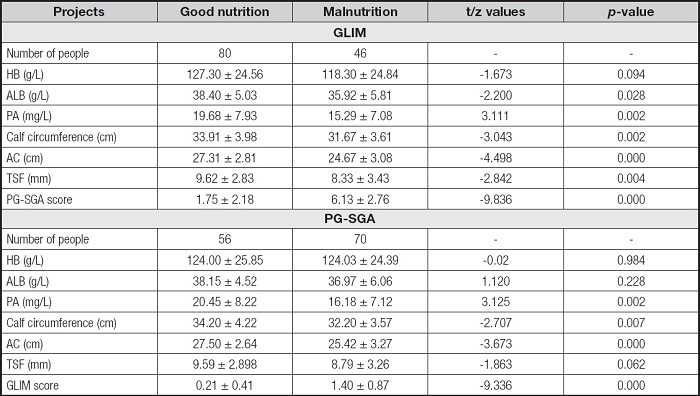
HB: haemoglobin; ALB: serum albumin; PA: serum pre-albumin; AC: upper-arm circumference; TSF: triceps skinfold thickness.
Conversely, the PG-SGA assessment categorised 56 participants as well-nourished and 70 as malnourished. The analysis revealed significant differences in all indicators across the nutritional status groups determined by PG-SGA, except for Hb, ALB, and TSF, where the differences were not statistically significant (p < 0.01) (Table IV).
Table V provides insights into the correlation analysis between GLIM and PG-SGA assessments and individual nutritional indicators. The results indicated negative correlations between the GLIM criteria and indicators such as ALB, PA, calf circumference, AC and TSF, while no significant correlation was observed with Hb.
Table V. Correlation analysis of each nutritional indicator with GLIM and PG-SGA.
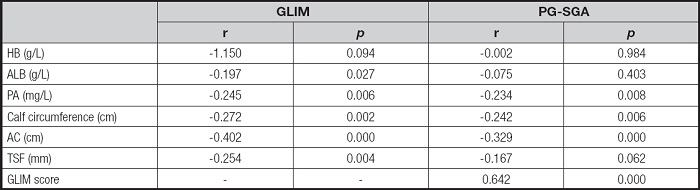
HB: haemoglobin; ALB: serum albumin; PA: serum pre-albumin; AC: upper-arm circumference; TSF: triceps skinfold thickness.
In contrast, the PG-SGA assessments exhibited negative correlations with all individual nutritional indicators, except for Hb, ALB and TSF. In addition, it is noteworthy that both PG-SGA and GLIM scores demonstrated significant correlations across all patients (p < 0.001) (Table V).
DISCUSSION
This study compared two nutritional assessment tools, the GLIM and the PG-SGA, within the context of patients undergoing surgery for hepatobiliary and pancreatic malignancies. These malignancies present a considerable risk of malnutrition, making accurate diagnoses crucial. The study’s findings revealed several significant differences and insights into these two assessment tools.
Initially, the GLIM assessment criteria, which necessitate the presence of positive nutritional screening alongside meeting performance-based and aetiological indicators, yielded a lower rate of malnutrition diagnoses (36.51 %) compared with the PG-SGA assessment (55.56 %). This discrepancy underscores the distinctiveness of these two tools. This study’s results align with previous cross-sectional studies that reported differences in malnutrition prevalence between the GLIM and PG-SGA assessments (14,16,17).
The higher malnutrition prevalence detected by the PG-SGA could be attributed to various factors. First, the two tools’ differing perspectives and evaluation criteria play a crucial role. The PG-SGA evaluates patients with mild to moderate malnutrition, whereas the GLIM assessment is preceded by nutritional risk screening, which assesses both the presence and severity of malnutrition (15,18). In addition, the PG-SGA strongly emphasises the patients’ subjective assessments of digestive symptoms and functional capacity, regardless of their weight loss percentage. Given that patients with hepatobiliary and pancreatic malignancies commonly experience reduced food intake and increased digestive tract reactions, the PG-SGA tends to yield higher malnutrition rates. Furthermore, the PG-SGA heavily relies on patients’ subjective assessments, which can introduce bias and data variability. Lastly, the GLIM assessment may encounter challenges in accurately assessing malnutrition in patients with ascites and oedema malignancies (19).
This study also demonstrated that combining the GLIM and PG-SGA diagnoses of malnutrition resulted in moderate sensitivity, which improved to good sensitivity when the PG-SGA diagnosed severe malnutrition. This suggests that the GLIM criteria are more sensitive in diagnosing severe malnutrition when severity ratings are not involved. However, including severity ratings led to a loss of consistency between the GLIM and PG-SGA assessments, indicating that not all patients with a PG-SGA grade C diagnosis were rated as severely malnourished by the GLIM. This discrepancy may be attributed to the presence of acute and chronic disease-associated inflammation in hospitalised patients, a factor not considered when introducing the aetiological criteria. This study suggests that incorporating acute and chronic disease-associated inflammation as an aetiological criterion, alongside c-reactive protein measurements as an objective indicator of inflammation, may enhance the validity of malnutrition assessments. Typically, the GLIM criteria exhibit better specificity than sensitivity due to the presence of acute and chronic infections in most oncology patients. While the PG-SGA lacks the inclusion of relevant inflammatory indicators, the GLIM’s aetiological criteria consider acute and chronic disease-associated inflammation, potentially improving specificity while reducing sensitivity.
In nutrition research, there is a growing need for streamlined tools that offer simple yet comprehensive assessments of nutritional status, reducing the burden of extensive testing. This study demonstrated that the GLIM criteria exhibited superior correlations with individual nutritional indicators compared with the PG-SGA. Notably, the GLIM assessment’s first nutritional risk screening component, BMI, emerged as a critical component, demonstrating direct correlations with two nutritional indicators. In contrast, the PG-SGA, developed specifically for oncology patients, provides a simple and easily synthesisable nutritional assessment without the need for extensive biochemical analysis. However, it focuses on assessing nutrient intake and body composition, overlooking intrinsic protein levels, which aligns with the absence of correlation with ALB (20).
To summarise, this study suggests that the GLIM criteria offer a more robust and comprehensive assessment of malnutrition, particularly in patients with hepatobiliary and pancreatic surgical malignancies. This echoes previous studies that have applied GLIM malnutrition assessment criteria in oncology patients.
It is essential to acknowledge the limitations of this research. The study’s sample size was relatively small and lacked follow-up data to assess the long-term prognostic implications of the two assessment tools. Moreover, the distinction between malnutrition and cachexia was not explored. Further investigations involving larger cohorts of patients undergoing surgery for hepatobiliary-pancreatic malignancies are warranted to assess the prognostic value of these assessments and provide more comprehensive insights into their clinical utility.
CONCLUSION
In conclusion, this study revealed distinctions in the diagnostic capabilities of the GLIM and PG-SGA nutritional assessment instruments. The GLIM tool demonstrates superior correlation with individual nutritional parameters, although relying solely on conventional nutritional metrics for impartial malnutrition evaluation, as per the criteria of either tool, is deemed insufficient. Importantly, concurrently using both tools results in a heightened incidence of severe malnutrition diagnoses, underscoring the congruity in their assessments. This investigation posits the potential suitability of GLIM as an effective means for appraising the nutritional status of patients in this cohort. Furthermore, it underscores the imperative for subsequent investigations to substantiate and enhance the selection of nutritional assessment tools in this specific context while considering the constraints associated with the study’s sample size and retrospective nature.