INTRODUCTION
Myopia is a complex trait influenced by genetic factors and numerous environmental (1). It has become increasingly common worldwide, most dramatically in urban Asia, and is rapidly inflicting on the United States and Europe (2). In a meta-analysis, it was estimated that the global prevalence of myopia reached 22.9 % in 2010, with a prediction that 49.8 % of the world's population would have it by 2050 (3). As a potentially sight-threatening condition, myopia has had major implications worldwide, both visually and financially (4,5). Therefore, it is important to identify modifiable risk factors for controlling the myopia development, especially preventing low and moderate myopia from developing high myopia.
The risk of myopia is higher with higher socioeconomic status, education, proximity to work, prenatal factors, and urbanization (2,6). Several studies have demonstrated that spending time outdoors has a protective effect on myopia in young adults and school-aged children (7,8). Different aspects of myopia occurrence, development, and clinical treatment have been studied in several studies focusing on metabolomic changes (7,8). Exposure to sunlight produces vitamin D endogenously. Vitamin D status is usually determined by the serum concentration of 25-hydroxyvitamin D [25(OH)D]. The relationship between serum 25(OH)D and myopia is few investigations (9-11). In recent years, the correlation between 25(OH)D and myopia increasingly has paid attentions. However, it remains controversial associated between serum 25(OH)D concentrations and myopia. In some studies, serum 25(OH)D concentration was associated with the prevalence of myopia, but not in all studies (12,13).
Therefore, we exploited this cross-sectional study to evaluate the association of serum 25(OH)D concentrations with myopia in a U.S. population using the National Health and Nutrition Examination Survey (NHANES) database.
SUBJECT AND METHODS
DATA SOURCES AND STUDY POPULATION
In this study, NHANES is an ongoing, two-year-cycle program administered by the Centers for Disease Control and Prevention of the United States. Physical and laboratory exams and standardized interview questionnaires were administered to all participants, including socioeconomic, demographic, and health-related questions. The National Center for Health Statistics Research Ethics Review Board has approved NHANES study protocol. Informed consent is obtained from all participants in writing. The NHANES database is available online with more information and details (https://www.cdc.gov/nchs/nhanes.htm). All reporting followed the Strengthening the Reporting of Observational Studies in Epidemiology guidelines (14).
In this study, we used public data from four cycles of the NHANES (2001-2002, 2003-2004, 2005-2006 and 2007-2008). Between 2001 and 2008, there were 41,658 participants in NHANES. Only participants (aged > 12 years) who underwent an examination of visual function were included. We excluded participants with surgery for myopia, cataract, and unknown surgery.
OPHTHALMIC DATA
In this study, participants aged 12 years or older were asked to undergo a visual function test. Our objective refraction measurements were taken using an autorefractor/keratometer (Nidek ARK-760A, Nidek Co. Ltd., Tokyo, Japan) in non-cycloplegic state and taken as the average of three measurements.
A spherical equivalent was calculated by dividing the cylindrical value by the spherical value. This is commonly used in epidemiological studies as a mean measurement. Myopia was defined as a spherical equivalent of -0.75 diopters (D) or less (low myopia, ≤ -0.75D to > -3D; moderate myopia, ≤ -3D to > -6D; severe myopia, ≤ -6D) (1). Those with a spherical equivalent greater than -0.75D were not considered to have myopia.
BLOOD MEASUREMENT
Liquid chromatography-tandem mass spectrometry was used to measure serum 25(OH)D concentrations, which is more sensitive and specific than immunoassays (15). The limit of detection of serum concentrations was 3.75 nmol/L for 25(OH)D. As mentioned above, NHANES used an imputed value for 25(OH)D when out of range. There were no values below the limit of detection of 3.75 nmol/L. Serum 25(OH)D concentration was classified as deficient group (< 50 nmol/L), insufficient group (50-75 nmol/L), and sufficient group (≥ 75 nmol/L) in our study. The measurement and assessment of these metabolites are described in detail on the NHANES website (https://wwwn.cdc.gov/nchs/data/nhanes/2009-2010/manuals/lab.pdf).
COVARIATES
In this study, covariates included sex (male or female), age, marital status (married, unmarried and other), education level (less than high school, high school or equivalent, college or above and other), poverty income ratio (PIR) (< 1, ≥ 1), body mass index (BMI) (< 25.0, ≤ 25.0 to < 30, and ≥ 30.0 kg/m2). Current smokers, former smokers, and never smokers were categorized according to their smoking status. Participants who had smoked more than 100 cigarettes in the past and reported smoking either some days or every day were considered to be current smokers, and who had smoked more than 100 cigarettes during their lifetime but did not smoke currently were considered former smokers. Participants who do not have smoked even 100 cigarettes during their lifetime were considered never smokers. TV or video hours per day was determined by the answer to the following question: “Over the past 30 days, on average, about how many hours per day did you sit and watch TV or videos?” According to answers, it was categorized as none; ≤ 1 hours; 2 hours; or ≥ 3 hours. Using a computer hours per day was determined by the answer to the following question: “Over the past 30 days, on average about how many hours per day did you use a computer or play computer games?” According to answers, it was categorized as none; ≤ 1 hour; or ≥ 2 hours. Dietary calcium intake and dietary magnesium intake were performed before the interview at MEC to collect the previous 24 h dietary information. The season of examination was categorized as summer or winter, according on whether the period of examination was between May to October or November to April, respectively (16).
STATISTICAL ANALYSIS
All normally distributed and skewed continuous variables are expressed as mean and standard deviation (SD) or median and interquartile range (IQR), and categorical variables as frequencies (%). The chi-square test (categorical variables), One-Way ANOVA (normal distribution), and Kruskal-Wallis test (skewed distribution) were used to compare variables. Multivariable logistic regression analyses were adopted to assess the association between serum 25(OH)D concentrations and myopia. We investigated serum 25(OH)D concentrations as a continuous variable and categorical variable. Subgroup analysis examined the relationship between serum 25(OH)D concentrations and the prevalence of myopia according to ages, sex, and education. Odds ratios (ORs) and 95 % CIs were calculated.
Our analyses were conducted using R 4.0 (http://www.R-project.org, The R Foundation) and Free Statistics version 1.4 (17). Statistical significance was determined by a two-tailed test. A p-value of 0.05 was considered significant.
RESULTS
BASELINE CHARACTERISTICS OF THE STUDY POPULATION
Four cycles of NHANES, 2001-2002, 2003-2004, 2005-2006, and 2007-2008, were used in our study. The flowchart of participants in the study design is illustrated in figure 1. The full and final data included 14,051 participants who met all inclusion and no exclusion criteria, of whom 4668 (33.2 %) had myopia. Table I shows the demographic, socioeconomic and baseline characteristics of no-myopia and myopia. Included participants had a mean (SD) age of 37.3 (19.6) years, of which 6914 (49.2 %) were males. In the myopic group, the mean (SD) age was 34.2 (17.4) years, and 2155 (46.2 %) were males. In non-myopic group, the mean (SD) age was 38.8 (20.4) years, and 4759 (50.7 %) were males. Age, sex, education level, marital status, BMI, PIR, smoking status, computer hours per day, dietary calcium, dietary magnesium, and season of examination were significantly different between the non-myopic and myopic groups. Compared with the non-myopic group, the myopic group was mostly accounted of females, and more likely to be younger, well-educated, higher income, and higher dietary calcium and dietary magnesium.
ASSOCIATION BETWEEN SERUM 25(OH)D CONCENTRATIONS AND THE PREVALENCE OF MYOPIA
We used regression analysis to identify factors which were associated with the prevalence of myopia in the entire study population. The results of univariate ordinal regression analysis indicated that age, sex, education, marital status, PIR, BMI, computer hours per day, season of examination, dietary calcium, and dietary magnesium were positively associated with the prevalence of myopia (Supplementary Table I).
Supplementary Table I. Univariate analysis between 25(OH)D and the prevalence of myopia.

PIR: a ratio of family income to poverty threshold; BMI: body mass index.
In the multivariable logistic regression, we observed that the odd ratios (ORs) of serum 25(OH)D concentrations were non-significant in all models (p > 0.05 for all) (Table II). There was no clear evidence for an association of serum 25(OH)D concentrations as a continuous variable with the prevalence of myopia (adjusted OR, 0.98 [95 % CI, 0.97-1.00]) after adjustment for age, sex, education, marital status, PIR, BMI, season of examination, dietary calcium, and dietary magnesium. We also investigated serum 25(OH)D concentrations as a categorical variable. In contrast, participants in the deficient group had no association with the prevalence of myopia compared with those in the insufficient group and sufficient group (adjusted OR, 0.96 [95 % CI, 0.89-1.05], 0.95 [95 % CI: 0.86, 1.06]) after adjustment for all covariates.
Table II. Association between 25(OH)D and the prevalence of Myopia (n = 14,051), NHANES 2001-2008.
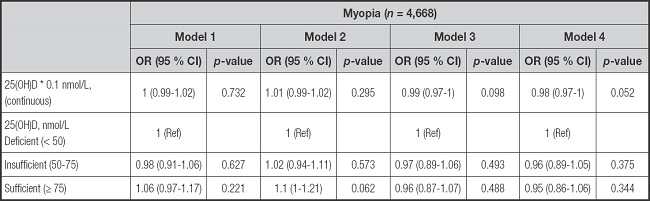
Adjusted covariates: Model 1: unadjusted; Model 2: adjusted by age, sex; Model 3: Model 2 + education, marital status, PIR, BMI, season of examination; Model 4: Model 3 + dietary calcium, dietary magnesium.
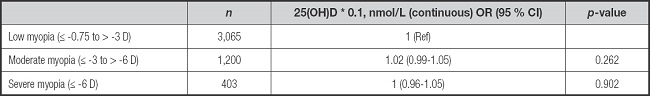
ASSOCIATION BETWEEN SERUM 25(OH)D CONCENTRATIONS AND THE SEVERITY OF MYOPIA
Myopia was classified as low myopic group (≤ -0.75 to > -3D), moderate myopic group (≤ -3 to > -6D), and severe myopic group (≤ -6D). In our study, the 4668 participants were included in the myopic participants with low myopic group (n = 3065), moderate myopic group (n = 1200), and severe myopic group (n = 403). In multinomial logistic regression, there was clear evidence for a non-significant association of serum 25(OH)D concentrations with increasing myopia severity after adjusting all covariates (adjusted OR, 1.02 [95 % CI, 0.99-1.05], 1.00 [95 % CI: 0.96, 1.05]) (Table III).
SENSITIVE ANALYSIS
To render our findings more robust, we excluded the participants without smoking status (n = 4328), TV or video hours per day (n = 4327), and computer hours per day data (n = 4058). The remaining 6613 participants were included. In the multivariable logistic regression, we made additionally adjusted smoking status, TV or video hours per day, and computer hours per day. The results remained stable (Table IV). Serum 25(OH)D concentrations as continuous variable do not associate with the prevalence of myopia (adjusted OR, 0.98 [95 % CI, 0.95-1.00]). Meanwhile, we investigated serum 25(OH)D concentrations as a categorical variable in the remaining 6613 participants. Participants in the deficient group had no association with the prevalence of myopia compared with those in the insufficient group and sufficient group (adjusted OR, 0.97 [95 % CI, 0.85-1.10], 0.95 [95 % CI: 0.81, 1.10]).
Table IV. Association between 25(OH)D and the prevalence of myopia (n = 6,613), NHANES 2001-2008.
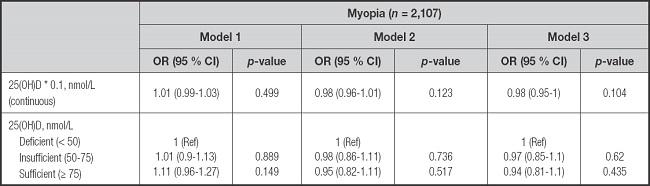
Adjusted covariates: Model 1: unadjusted; Model 2: adjusted by age, sex, education, marital status, PIR, BMI, season of examination, dietary calcium, dietary magnesium; Model 3 + smoking status, TV or video hours per day, computer hours per day.
We also performed a stratified analyses to robust our findings. We investigated whether the association between serum 25(OH)D concentrations and the prevalence of myopia varied at different ages, sex, and education. In the stratified analyses, the results remain stable (Fig. 2). The multiplicative interactions of serum 25(OH)D concentrations and ages (p for interaction = 0.409), serum 25(OH)D concentrations and sex (p for interaction = 0.131), and serum 25(OH)D concentrations and education (p for interaction = 0.241) in regard to the prevalence of myopia were not significant.
DISCUSSION
In this study, we investigated the associations between serum 25(OH)D concentrations and the prevalence of myopia in the U.S. population. We found that serum 25(OH)D concentrations were not associated with the prevalence of myopia. In stratified analysis, the results remained stable with different ages, sex, and education. In our analyses, there was scant evidence that serum 25(OH)D concentrations were themselves associated with myopia. Vitamin D could not be a possible target for myopia interventions. It may be not directly involved in the prevalence of myopia, just as a marker of time spent outdoors.
Our findings about serum 25(OH)D concentrations and the prevalence of myopia are consistent with results of some previous studies (18-20). In Specht IO's case-control study, it observed no statistically significant associations between neonatal 25(OH)D3 and myopia in young adulthood (n = 1737) (19). Lingham et al. found that low 25(OH)D concentration was not associated with odds of myopia or spherical equivalent in middle-aged and older western (n = 1737) (20). However, our study had much larger numbers of participants (n = 14,051) and used sensitive analysis to minimize the potential confounders, and found no relationship between serum 25(OH)D concentrations and the prevalence of myopia.
In a Multicountry European Study, Katie M's cross-sectional study (n = 4166) indicated that in the adjusted analyses, no convincing evidence was reported for an association of 25(OH)D3 concentrations with myopia aged older than 65 years old (adjusted OR, 0.99 [95 % CI, 0.98-1.00]) (1). Their results are akin to our findings. However, this study only enrolled 4166 patients. And it still overlooked several important confounders, such as dietary calcium intake (17) and dietary magnesium intake (16). Our study had much larger sample size (n = 14051) and considered dietary calcium intake and dietary magnesium intake as confounders.
Xiaoman Li et al. conducted a cross-sectional study in China (n = 383) and described serum 25(OH)D concentrations were not associated with myopia in the 6-14 years old Chinese children (adjusted OR, 0.99 [95 % CI, 0.97-1.02]) (21). In a cross-sectional observational study Sahira Aaraj et al. found that association of low vitamin D levels and myopia was not significantly in Pakista children aged 5-15 years (22). These phenomenons also can be found in our study, serum 25(OH)D concentrations were non-significantly with myopia in the 12-19 years old U.S. participants (adjusted OR, 0.98 [95 % CI, 0.95-1.00]). Participants (n = 4051) aged between 12-19 years old were all included in our study.
In our study, the serum 25(OH)D concentrations were not associated with the prevalence of myopia in different ages. However, some previous studies were inconsistent with our results. Previous national survey studies in Korean populations had observed a significant association between low serum 25(OH)D concentration and myopia prevalence in Korean adolescents and adults, particularly notable in adolescents with high myopia (23,24). Compared with our study, some pivotal risk factors, such as the season of examination (13) and dietary magnesium intake (16) were not effectively controlled in these studies. In this study, we used stratified analyses to investigated the association between serum 25(OH)D concentrations and the prevalence of myopia varied at different ages, sex, and education. Using different populations may be the other reason for the inconsistency between the two studies.
In some studies, there was a significant association between the prevalence of myopia and vitamin D in young people. In three cohort studies, the prevalence of myopia was significantly associated with vitamin D in children and young adulthood (13,25,26). In a cross-section study, serum 25(OH)D concentration is related to the prevalence of myopia in Chinese children (27). Compared with our study, these studies only included people under the age of 20, whereas our study included the entire population, with much larger sample size (n = 14,051). Meanwhile we conducted sensitivity analysis for different ages, the results remain stable with different ages.
It is still unclear the role of serum 25(OH)D concentrations in the prevalence and severity of myopia. In a Mendelian randomization study, it showed that the true contribution of vitamin D levels to degree of myopia is very small. In previous observational studies, the association between vitamin D levels and myopia were likely confounded by time spent outdoors (28). It has been identified as the protective effect of time outdoors on myopia in young adults (7). However, whether 25(OH)D is directly involved in myopia or merely acts as a biomarker of time spent in outdoor activities needs to be verified.
This study has several limitations. First, as a cross-sectional study it could not show causality. Second, we considered many covariates. However, the results may be affected by unmeasured confounding factors. For example, time spent outdoors was not considered in our study because of inadequate data in the NHANES database. We adjusted for possible confounders in order to minimizing the influence of factors which may lead to outcome bias, and we also used stratified analyses. We investigated the association between serum 25(OH)D concentrations and the prevalence of myopia varied at different ages, sex, and education. The result was robust. Finally, non-cycloplegic auto-refractor for myopia assessment may be the other limitation, because the effect of accommodation in adolescents was not excluded. In the NHANES database, the use of cycloplegic medication was also not specified before refracting the subjects. These might lead to classification bias in our study. However, we conducted sensitivity analysis for different ages, it is also robust.
CONCLUSIONS
This study suggests that serum 25(OH)D concentrations were non-significantly associated with myopia in the U.S. population. This might provide some clinical clues, however further randomized controlled studies are required to provide more evidence.
Ethical approval:
the survey protocol for the NHANES was approved by CDC's National Center for Health Statistics Institutional Research Ethics Review Board. All participants provided written informed consent, and the study was approved by the NCHS Research Ethics Review Board (https://wwwn.cdc.gov/nchs/nhanes/default.aspx).