INTRODUCTION
Waist circumference (WC) is the main indicator of abdominal adiposity and reflects the amount of visceral adipose tissue (VAT). Therefore, it is considered the best measurement for detecting patients at risk of cardiovascular disease (CVD) (1). CVD risk assessment in children with obesity has gained relevance because it may predict increased mortality in adulthood owing to coronary heart disease and stroke (2). Obesity in children is associated with type 2 diabetesmellitus (T2DM), dyslipidemia, arterial hypertension, non-alcoholic fatty liver disease, genu valgum, and obstructive sleep apnea (3). The pathophysiological mechanisms that lead to an increased risk of developing CVD with early atherosclerosis in patients with obesity (4) are related to increased insulin resistance (IR) (5) and activation of chronic inflammation (6). The CVD risk in children is assessed based on the presence of metabolic syndrome (MetS). The “Third Report of the National Cholesterol Education Program (NCEP) in Adults Panel of Treatment III” (7) defined MetS when a patient has three of the following components: abdominal obesity measured by WC, increased triglyceride (TG), decreased high-density cholesterol (HDL), hypertension, and fasting hyperglycemia or T2DM (8).
The detection of CVD risk factors is perform with WC measurement in the routine physical exam. Although this evaluation is practical and simple; several recommendations should be made for each anatomical measurement site (Fig. 1). The WC at the narrowest visual abdominal part (WCnarrow) was initially described by Lohman et al. (9) and later by the International Society for the Advancement of Kinanthropometry (ISAK) (10), the WC at the midpoint between the lower rib and the top of the iliac crest (WCmiddle) by the World Health Organization (WHO) (11), and the WC above the border of the iliac crest (WCiliac-crest) by the National Health and Nutrition Examination Survey (NHANES) (12). WC at the level of the umbilicus (WCumbilicus) was described by Croft et al. (13) and Eisenmann et al. (14). WC4 was unusual and described by Rudolf et al. (15).
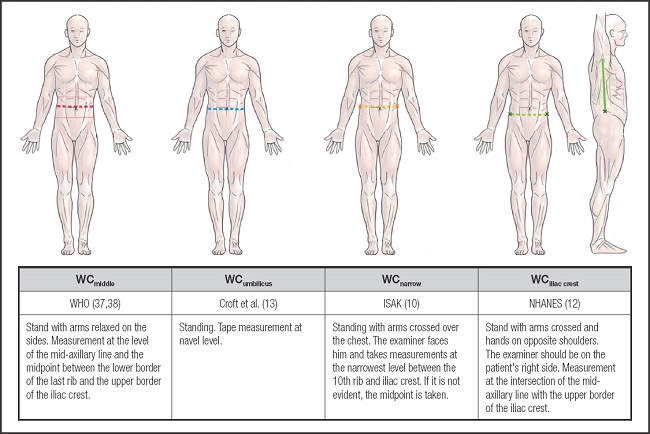
Figure 1. WC measurement recommendations (WHO: World Health Organization; ISAK: International Standards for Anthropometric Assessment, United Kingdom; NHANES: National Health and Nutrition Examination Survey).
Interestingly, the anatomical WC measurement site was not based on comparative correlation studies between different WC measurement sites and cardiovascular risk. The objective of this review is to evaluate anatomical WC measurement sites and their comparative correlation with other MetS components in children.
METHODS
The study protocol was registered in the Prospero ID CRD42023454847.
SEARCH STRATEGY
The literature search was conducted by AMBT, without language restriction in Lilacs, MEDLINE/PubMed, Web of Science, and Scopus databases on October 2023. Papers published between January 2005 and August 2023 were included. The PICO framework was used to develop search strategies and ensure comprehensive and bias-free searches: Population: Patients between 2-18 years. Intervention: WC measurement. Comparison: WC measurement at different anatomical sites (≥ 2). Diagnostic outcomes: CVD risk or other MetS components.
The combination of the boolean descriptors were: “Waist circumference” AND (“measurement anatomical sites” OR “Waist circumference AND pediatric OR cardiometabolic risk factor”). “Waist circumference” AND (“measurement anatomical sites” OR “Waist circumference AND pediatric OR metabolic syndrome”). “Waist circumference measurement sites” and “metabolic syndrome.”
ELIGIBILITY CRITERIA
Observational studies that had ≥ 2 anatomical sites of WC and their correlation with MetS or other components of MetS.
STUDY QUALITY AND RISK OF BIAS ASSESSMENT
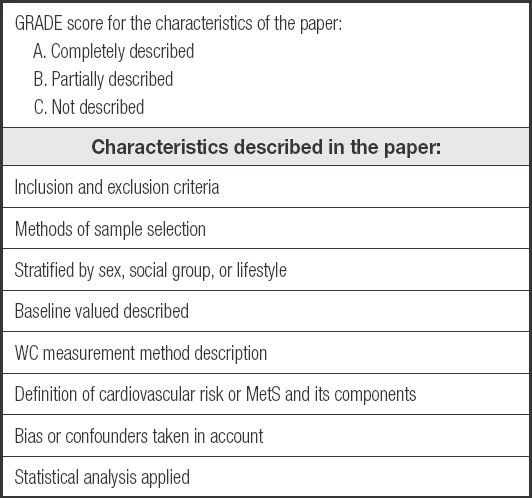
Eligible studies were assessed by two investigators independently (RGM and DBML). Any divergence was resolved by a third evaluator (LFMR). The quality of each study was determined using the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) checklist (22 items) (16). The modified Grading of Recommendations Assessment, Development, and Evaluation (GRADE) scale (Table I) was applied, considering A (good), B (moderate), and C (low) when the paper characteristics were complete, partial, or non-specific, respectively.
THE STRATEGY OF DATA SYNTHESIS
The methodology of the systematic review followed the Cochrane Manual guidelines (17), and was adjusted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines (18).
STATISTICAL ANALYSES
Meta-analysis was performed with Jamovi 2.2.5 version (by EELH and MLEV) using WC coefficients of correlation with components of MetS included in 4/5 articles. Bosy-Westphal et al. (19) were excluded because they included both children and adults. The WC measurements included in the meta-analysis were the WCiliac-crest and WCmiddle. Other WC measurements were excluded because there were only two publications of each one. A random effects model was used to fit the data. Analysis was performed using the Fisher r-to Z-transformed correlation coefficient. Heterogeneity was estimated using the Cochran Q test and I² statistic. If I2 > 50 % orp < 0.1, heterogeneity of the results was considered. Studentized residuals and Cook distances were used to determine whether the studies were outliers or influential in the model context. Studies with a studentized residual larger than the 100 × (1 – 0.05 / [2 × k]) th percentile of a standard normal distribution were considered potential outliers. Studies with Cook's distance greater than the median and six times the interquartile range of Cook's distance were considered influential. The Begg and Muzumbar rank correlation test and Egge's regression test, using the standard error of the observed outcomes as a predictor, were used to verify the funnel plot asymmetry.
RESULTS
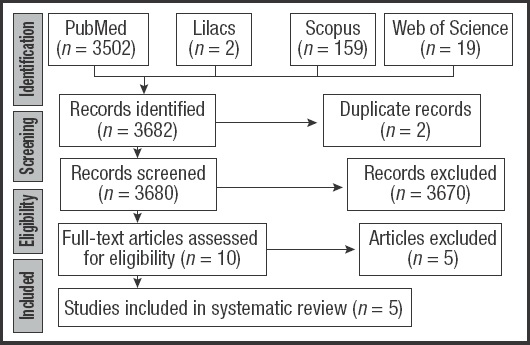
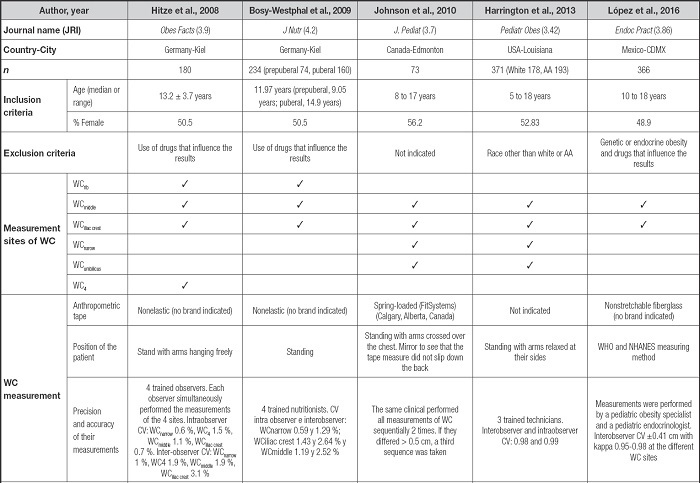
From 3,680 non-duplicate records, ten studies were selected because they evaluated ≥ 2 WC anatomical sites. After the full texts were reviewed, five studies were excluded because they did not include MetS components (Fig. 2). Finally, we included five studies with 1,224 children (5-18 years old) of both sexes: Hitze et al. (20) and Bosy-Westphal et al. (19) (both in the German group), Johnson et al. (21), Harrington et al. (22), and López et al. (23).Table II presents the characteristics of the studies. Bosy-Westphal et al. studied prepubertal and pubertal children and adults. Except for the study by López et al. (23), all other studies divided their results by sex. Harrington et al. (22) assessed children according to ethnicities(21). Each article measured WC at to 2-4 anatomical sites, which showed adequate reproducibility. WC of the inferior margin of the ribs (WCrib) was measured in the German group (19,20). The WC at the level of the umbilicus (WCumbilicus) and WCnarrow was measured by Johnson et al. (21) and Harrigton et al. (22). WC was measured four centimeters (cm) above the umbilical scar (WC4) and was evaluated by Hitze et al. (20). The WCiliac-crest and WCmiddle were measured in all studies included in this review.
Table II (cont.). Structured summary of the results of the included studies.
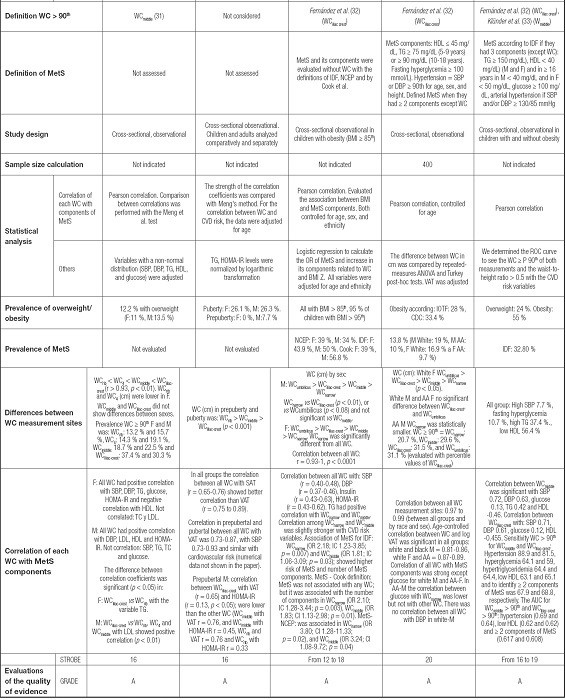
JRI: journal rank indicator; AA: African American; WHO: World Health Organization; NCHS: National Center of Health Statistics; CV: coefficient of variation; MetS: metabolic syndrome; IDF: International Diabetes Federation; NCEP: National Cholesterol Education Program; HDL: high density lipoprotein cholesterol; TG: triglycerides; SBP: systolic blood pressure; DBP: diastolic blood pressure; M: male(s); F: female(s); BMI: body mass index; CVD: cardiovascular disease; HOMA-IR: Homeostatic Model Assessment for Insulin Resistance; OR: odds ratio; VAT: visceral adipose tissue; NPV: negative predictive value; PPV: positive predictive value. BMI: body mass index; IOTF: International Obesity Task Force; CDC: Centers for Disease Control and Prevention; NHANES: National Health and Nutrition Examination Survey; TC: total cholesterol; LDL: low-density lipoprotein cholesterol; SAT: subcutaneous adipose tissue; CI: confidence interval; AUC: area under the curve; STROBE: Strengthening the Reporting of Observational studies in Epidemiology; GRADE: Grading of Recommendations; Assessment; Development and Evaluation.
All studies evaluated WC while standing but with different arm positions: hanging freely (19,20) or crossing over the chest (21).
STATISTICAL EVALUATION IN THE INCLUDED STUDIES
Pearson's correlation was performed between each WC measurement site and MetS components in all articles. In some cases, adjustments for age (19,22), ethnicity (21), or logarithmic transformation of variables are necessary (19-23). The prevalence of obesity and MetS differed between these studies (21-23). Johnson et al. (21) described a different prevalence of MetS according to each definition criterion: the modified National Cholesterol Education Program (NCEP) (24), International Diabetes Federation (IDF) (25), and Cook et al. (26). López et al. (23) described MetS according to the IDF (Table II).
DIFFERENCES BETWEEN WC MEASUREMENT SITES
The studies showed that the magnitude of WC (cm) was different in measurement sites and that there were inherent to sex, ethnicity and puberal stage (20). The correlation between the magnitude of all WCs was strong (r = 0.93-0.99).
WC MEASUREMENT SITES AND METS
In Hitze et al. (20), in the female (F) group, all WC measurements showed positive correlations with systolic blood pressure (SBP), diastolic blood pressure (DBP), TG, glucose, and Homeostatic Model Assessment for Insulin Resistance (HOMA-IR), but they did not show any correlation with total cholesterol (TC) and low-density cholesterol (LDL). In the male (M) group, all WC measurements were positively correlated with DBP, LDL, and HOMA-IR. They did not show any correlation with the SBP, TG, TC, or glucose levels.
Bosy-Westphal et at. (19) showed that the WC measurement correlation at all anatomical measurement sites was adequate with abdominal fat, but it was better with subcutaneous adipose tissue (SAT) than with VAT. In prepubertal M, the relationship between the WCiliac-crest with VAT and HOMA-IR was lower than that in the other WC.
In Johnson et al. (21) the correlation coefficient showed a significant positive association between all WC measurement sites and the SBP, DBP, and HOMA-IR. The TG levels were positively correlated with WCnarrow and WCmiddle. Correlation between CVD risk variables and WCnarrow or WCmiddle was slightly higher. The correlation between MetS and CVD risk was similar for all WC measurements, with only differences. According to the IDF definition of MetS, WCnarrow and WCmiddle were significantly associated with MetS, and the number of MetS components. According to Cook's definition of MetS, there was no association between MetS and all WC; however, WCnarrow and WCmiddle showed significant odds ratios (OR) with the number of MetS components. For the definition of MetS according to the NCEP, an association was observed between MetS and WCnarrow or WCmiddle but not with WCiliac-crest or WCumbilicus.
Harrington et al. (22) evaluated the age-controlled correlation between WC and logVAT was significant in all the groups. The correlation between all anatomical measurement sites and MetS components was good, except for the glucose levels in the white-M and AA-F groups. There was no correlation between any WC measurement site and DBP in the white-M.
López et al. (23) reported a statistically significant correlation between WCmiddle and WCiliac-crest and SBP, DBP, TG, and HDL levels. Glucose levels showed a low correlation with all WCs measurements.
The STROBE scale yielded a result between 12 and 20 points for 22 items. The modified GRADE scale results for all included articles were A (good evidence) (Table II).
META-ANALYSIS
Figure 3 shows the results of the meta-analysis. The random-effects model showed that the correlation of WCiliac-crest and WCmiddle with the average variables of MetS differed significantly from 0. The WCiliac-crest and WCmiddle I2 test in all evaluations with the CVD risk variables showed heterogeneity: HDL (66.4 %,p = 0.028 and 69.12 %,p = 0.019), TG (77.96 %,p = 0.006 and 68.78 %,p = 0.028), SBP (94.68 %,p < 0.001 and 95.7 %,p < 0.001), and DBP (90.09 %,p < 0.001 and 90.56 %,p < 0.001). Glucose presented low heterogeneity in both WC (0 %,p < 0.634; 0 %,p < 0.722). In the studentized analysis, López et al. (23) presented atypical values for HDL, SBP, and DBP for WCmiddle and WCiliac-crest. Glucose analysis in both WC and TG in WCmiddle showed no outliers. Hitze et al. (20) showed the possibility of an outlier in the correlation between WCmiddle and TG levels. Cook's evaluation showed that none of the studies could be considered influential on any of the variables studied. Egge's regression analysis and Begg's rank correlation tests did not indicate asymmetry in the components of MetS evaluated; therefore, the construction of the funnel graph (Fig. 3) with a few studies generated the possibility of bias.
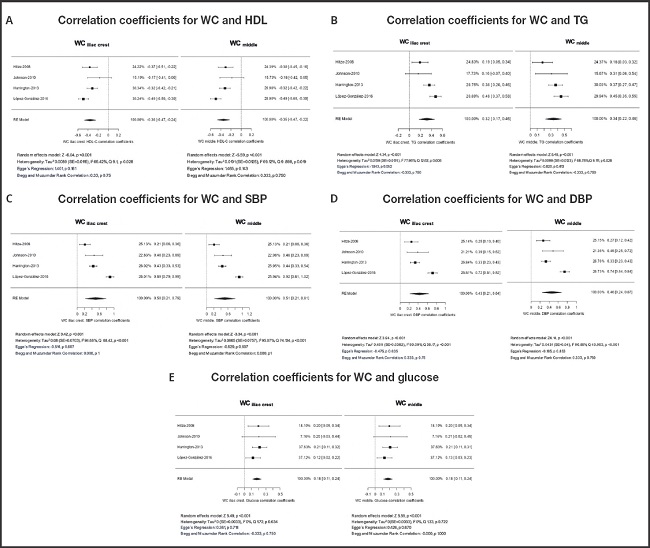
Figure 3. Meta-analysis of correlation coefficients for WCiliac-crest, WCmiddle, and MetS components (WC: waist circumference; WCiliac-crest: waist circumference measured above the iliac crest; WCmiddle: waist circumference measured between the floating rib and the iliac crest; MetS: metabolic syndrome; HDL: high-density lipoprotein cholesterol; TG: triglycerides; SBP: systolic blood pressure; DBP: diastolic blood pressure) (Supplementary material:https://www.nutricionhospitalaria.org/anexos/05144-01.pdf).
DISCUSSION
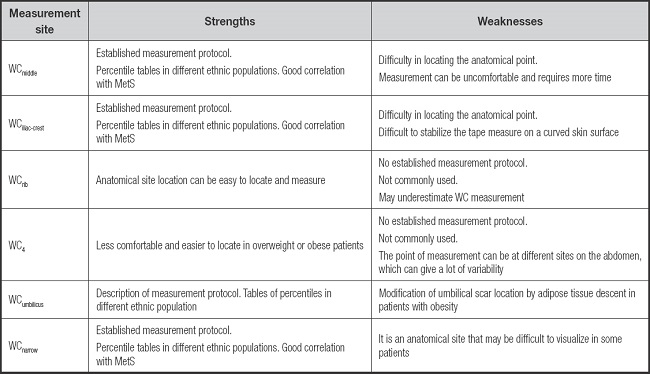
This review shows that the studies included had adecuate comparative correlation between all WC measurement sites and other MetS components except glucose which shows a low correlation. It provides an advantage because measurements are easier at certain anatomical points depending on the characteristics of each patient.
The correlation coefficient evaluation in this meta-analysis shows no difference in the correlation between WCmiddle or WCiliac-crest and other MetS components. Studies carried out in different countries have shown that measuring WCmiddle can predict the presence of MetS in pediatric patients (27,28). WC is considered a good predictor of MetS because it is positively correlated with MetS (29). A review in adult patients reported that there was no substantial difference in the WC measurement site protocols in terms of cardiovascular morbidity, and mortality (30).
We were not able to perform stratified analyses by sex, age, pubertal stage or ethnicity, because data were insufficient. Children are in constant development: this modifies the correlation between WC measurements at different anatomical sites and other MetS components. Fat distribution is very similar between girls and boys in their first childhood years, and then changes at puberty, the beginning of sexual development (31,32). Other studies have already shown these differences by sex in abdominal fat distribution, and some indicate that the presence of obesity does not seem to modify this distribution; that is, the WCnarrow is the smallest and the WCumbilicus is the largest (33). Furthermore, it is possible that the fat deposits distribution by ethnic group may contribute to different cardio-metabolic risk (34).
Some studies included in this review defined the overwaist at all anatomical sites using percentiles created for WCmiddle. This may have modified their results because each WC anatomical measurement site should have specific percentile value. This is important when evaluating a clinical measurement that constitutes a diagnostic tool for MetS, and to avoid bias. We did not find percentile values for WCrib in the literature, and there are only few population studies for the WCumbilicus (14) and WCnarrow (35,36).
In children and adolescents, all definitions of MetS (IDF, Cook, and ATP III) consider the same components, but there is great variability due to lack of standardization of the cut-off points. Similary, the frecuency of WC ≥ 90th percentile varies according to the WC measurement site and the MetS definition used, modifying therapeutic decisions. The lack of consensus on the WC measurement site in children underestimates or overestimates the CVD risk, as reported in research studies on MetS.
All studies reviewed followed appropriate measurement techniques and standardization, although each author differed in the arms position. The subject's position standing upright with arms relaxed on both sides was described by Lohman et al. (9) to measure WCnarrow and by the WHO to measure WCmiddle (37,38). Patients standing with arms crossed over their chest and hands on their shoulders were described by NHANES (12) to measure the WCiliac-crest and by ISAK (10) to measure WCnarrow (20-22). Thus, Lennie et al. (39) found significant differences in WC measurements performed at different positions in adults. There have been no studies on this topic in the pediatric population. In the smallest or very restless children, arms crossed on the chest and hands on the shoulders are more comfortable and provide more stability.
Technical difficulties in locating bony anatomical references in children with obesity are uncomfortable for patients (15); therefore, WCnarrow and WCumbilicus facilitate waist measurement. Some children with significant abdominal subcutaneous tissue have a hanging position at the umbilicus, which modifies the umbilical scar position.
However, this measurement may still be significant due to the prominence of the abdomen. In daily pediatric practice, WC is measured by physicians, nutritionists, pediatricians, and nurses. Work team training is essential to ensure precision in the technique and the anatomical site of measurement.
Intable III, we summarize the strengths and weaknesses of each WC measurement site in children that can be better adapted to daily clinical practice according to training in measurement techniques and the characteristics of children.
A major limitation of our results is related to the fact that only few studies have assessed the correlation between different anatomical WC measurement sites and MetS in children and adolescents. This draws attention, considering that WC is the most relevant point for CVD risk exploration in clinical practice. Therefore, this systematic review should be the starting point for future studies on the specific characteristics of CVD risk according to age and sex at different measurement sites. It is essential to create specific percentiles for each WC measurement site for each ethnic group or population.