Introduction
The term emotional disorders (here in after, EDs) has been used to denote the group consisting of anxiety, depressive, trauma- and stressor-related, obsessive-compulsive, dissociative, somatic symptom and related disorders (Bullis et al., 2019). Currently, EDs are the most prevalent psychological disorders worldwide (World Health Organization (WHO), 2017).
In Spain, it is estimated that 4.1% of the population has at least one anxiety disorder, accounting for almost 2 million people, and 5.2% of the population has a mood disorder, accounting for almost 2.5 million people (WHO, 2017). Understanding comorbidity as the presence of one or more disorders in addition to the primary disorder (Feinstein, 1970), a study conducted by Roca et al. (2009) showed comorbidity rates of mental disorders reaching 30.3%. In more detail, 13.8% with 2 diagnoses, 8.2% with 3 diagnoses, 5.6% when there are 4 diagnoses and 2.7% with 5 or more. In the case of EDs, there is a 19.1% comorbidity between anxiety disorders and mood disorders.
The high prevalence of EDs and their high comorbidity cause an increase in the demand for psychological care and, consequently, the collapse of the public health system (Ruiz-Rodríguez et al., 2017), which is observed in long waiting lists (Viberg et al., 2013), the long time between appointments (Martín-Jurado et al., 2012), and also because of the high public expenditure (economic, material and human resources) (WHO, 2011). This situation causes a large number of people to choose to seek psychological care in the private context, where General Health Psychologists (GHPs) provide their professional services. Specifically, 87% (28.923) of psychologists who are members of a Professional College of Psychology and have clinical and health psychology training in Spain (33.209), are GHPs (Instituto Nacional de Estadística (INE), 2019).
In addition to the high prevalence and comorbidity of EDs, it is important to highlight, also, that different studies suggest that patients do not receive evidence-based psychological treatments (hereinafter, EBPTs) to address their psychological problems (Dozois, 2013). An example of this would be the data obtained by WHO (2013), where it is observed that, in low- and middle-income countries, between 76 and 86% of people with mental disorders do not receive EBPTs; the percentage is also high in countries with higher incomes: between 30 and 50%. In addition to this situation, EBPTs are sometimes not applied faithfully or are used inconsistently, i.e., without including all the recommended components (Stobie et al., 2007). As a result of this situation, patients do not benefit from the knowledge accumulated in decades of research (Tasca et al., 2015), even having a negative impact on their well-being and recovery (Constantino et al., 2017).
In relation to EBPTs, in recent years, there is increasing interest in psychological interventions based on the transdiagnostic approach. This perspective is characterized by the design of single treatments targeting etiological and maintenance processes common to different disorders or groups of disorders, as opposed to different specific diagnostic categories (Castro, 2011). Furthermore, it is argued that the development of treatments aimed at addressing etiological factors common to different mental disorders could increase the efficacy rates of interventions (Tortella-Feliu et al., 2016). In relation to EDs, the transdiagnostic approach suggests that this group of disorders share etiological and maintenance factors (e.g., high neuroticism), which could also explain their high comorbidity (Brown & Barlow, 2009). Based on these assumptions, David H. Barlow and his team have developed the Unified Protocol for the Transdiagnostic Treatment of Emotional Disorders (hereafter UP; Barlow et al., 2018).
The UP is an intervention based on emotional regulation strategies organized in different modules, in each of which a specific strategy is trained (Barlow et al., 2004). It proposes that therapists learn a single form of intervention, in order to provide a single EBPT for the most prevalent disorders. It is a protocolized treatment (i.e., it has a manual for the therapist and another for the patient) thus facilitating training and subsequent implementation (Bullis et al., 2015).
The UP has recently demonstrated its efficacy in several controlled studies in individual format, obtaining effect sizes that are at least comparable to those obtained in disorder-specific cognitive-behavioral therapies (i.e., Barlow et al., 2017). The effects are promising, reflecting significant clinical improvements in most of the patients to whom it is applied, even in long-term follow-ups (between 6 and 12 months) (Bullis et al., 2014). Furthermore, it has demonstrated its efficacy for the treatment of EDs, including those cases presenting comorbidity and those with depressive or anxiety symptoms, both in systematic review (Cassiello-Robbins et al., 2020) and meta-analysis studies (Carlucci et al., 2021; Sakiris & Berle, 2019).
In addition to the availability of EBPTs, it is necessary to train and educate psychology professionals (dissemination) as well as to study the degree of acceptability of the treatments and their intention to use them in the future. According to Mira et al. (1999), acceptability is the degree of user satisfaction with the care received. Based on this, a theoretical framework, based on a systematic review, has recently emerged that assesses the acceptability and unifies the approaches into a single theoretical framework, Theoretical Framework of Acceptability (TFA), developed by Sekhon et al. (2017). This model is composed of seven constructs: (1) Affective Attitude (how an individual feels about the intervention); (2) Burden (the amount of perceived effort required to participate in the intervention); (3) Ethicality (the extent to which the intervention fits an individual's value system); (4) Intervention coherence (the extent to which the participant understands the intervention and how it works); (5) Opportunity Costs (the extent to which benefits, gains, or values must be given up to participate in the intervention); (6) Perceived Effectiveness (the extent to which the intervention is perceived to be likely to achieve its purpose); (7) Self-efficacy (the participant's confidence that he or she can perform the behavior required to participate in the intervention). In sum, it is important to assess the efficacy and acceptability of EBPTs by the patients who receive them and the psychologists who implement them, as it contributes to improving their quality and facilitates treatment engagement and adherence to treatment (Geers et al., 2013).
Regarding patients, different studies on the acceptability of the UP in clinical samples have found high levels of acceptance and satisfaction (Bentley et al., 2018; Osma et al., 2019; Sauer-Zavala et al., 2019). In relation to acceptability on the part of the therapists, the only study that has been found in relation to the UP is the one carried out by Peris-Baquero et al. (2021), with a sample of Psychologists Specialists in Clinical Psychology working in the Spanish Public Mental Health System. This study utilized the TFA and results showed high scores in all dimensions of acceptability, as well as a high intention to use in the future.
Despite the good results of this study, to date, the degree of acceptability and intention to use the UP by psychologists working in the private sector in our country has not been explored. Therefore, the present study sets out as objectives: (1) To analyze the degree of knowledge that General Health Psychologists (GHPs) have about transdiagnostic treatments and, specifically, the degree of knowledge of the UP; (2) to evaluate the degree of acceptability and intention to use in the future the UP in a sample of GHPs, after receiving specialized training in this protocol. We hypothesize an average degree of knowledge about transdiagnostic treatments and the UP and that after the training, participants will present high levels of acceptance and intention to use the UP in the future; (3) to analyze in an exploratory manner whether there are sociodemographic factors or the different constructs that form the TFA that could be related to the intention to use UP in the future in their clinical practice. By analyzing acceptability and intention to use in detail, we hope to gain a better understanding of the real possibilities of UP dissemination and implementation among GHPs working in the private health care context in Spain.
Method
Participants
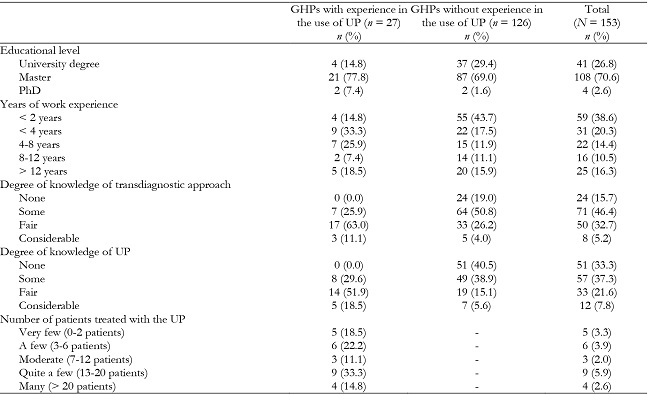
The sample consisted of 244 participants who agreed to complete a survey after a UP training course offered in the Professional College of Psychology of Aragon. Of these, 68 were excluded because they worked in fields other than health psychology (i.e., social and/or educational psychology) and 23 because they had missing values. The final sample consisted of 153 GHPs working in the private health care setting, with a mean age of 36.92 years (SD = 10.98, range 22 - 67) and 76.5% were female (n = 117). The participants were grouped according to the experience they had with the use of the UP, creating two subgroups, one formed by participants with experience in the use of the UP (n = 27), with a mean age of 35.42 years (SD = 10.28, range 24 - 58) and 74.1% were women (n = 20) and the other without any experience in the use of the UP (n = 126), with a mean age of 37.25 years (SD = 11.15, range 22 - 67) and 77.0% were women (n = 97). The remaining sociodemographic information can be found in Table 1.
Measures
Sociodemographic data questionnaire: The information collected, in addition to sex and age, included questions on: completed studies, area of work, type of clinical specialty, years of work experience in the context of psychotherapy, degree of knowledge about the characteristics of the transdiagnostic approach in psychotherapy before taking the UP training course, degree of knowledge about the characteristics of UP as a treatment for EDs before taking the UP training course, experience in the use of UP with patients, and, if they answered affirmatively, degree of experience in its use (number of patients attended with UP).
Acceptability Questionnaire based on the TFA model (Sekhon et al., 2017). This ad hoc created questionnaire consists of 7 items with a Likert-type response scale ranging from 1 (completely disagree, no effort, unsure or unacceptable) to 5 (Strongly agree, great effort, very sure or completely acceptable). This questionnaire was adapted according to whether the participants had used the UP previously:
Acceptability Questionnaire in GHPs with experience in UP use: (1) Affective attitude: To what extent did you like or dislike using it?; (2) Burden: How much effort did it cost you to apply the UP?; (3) Ethicality: Were there any negative ethical or moral consequences of applying the UP?; (4) Intervention coherence: Did the way in which the UP tried to achieve improvements in your patients' emotional regulation make sense to you? (5) Opportunity Costs: Did the application of the UP interfere with your other priorities in psychotherapy?; (6) Perceived Effectiveness: To what extent do you think the UP helped your patients regulate their emotions?; and (7) Self-efficacy: To what extent did you feel competent in applying the UP?
Acceptability Questionnaire in GHPs without experience in using the UP: (1) Affective attitude: Do you think you will like or dislike applying the UP?; (2) Burden: How much effort do you think it will cost you to apply the UP?; (3) Ethicality: Do you think there are negative ethical or moral consequences for applying the UP?; (4) Intervention coherence: Do you think it makes sense to you how the UP is intended to achieve improvements in patients' emotional regulation?; (5) Opportunity Costs: Do you think it makes sense to you how the UP is intended to achieve improvements in patients' emotional regulation? (5) Opportunity Costs: Do you think the application of the UP will interfere with your other priorities in psychotherapy?; (6) Perceived Effectiveness: Do you think the UP will help patients achieve emotion regulation?; and, (7) Self-efficacy: Do you think you will feel competent to apply the UP?
Questionnaire on intention to use the UP in the future. The ad hoc question was posed: “To what extent would you accept to apply it again?”, in the case of GHPs with experience in the application of the UP, and “To what extent would you accept to use the UP?”, in the case of participants with no experience in the use of the UP. The response format was a 5-point Likert-type, ranging from 1 (never) to 5 (always).
Procedure
The sample composing the study was obtained through the Professional College of Psychology of Aragon, more specifically, from among those participants who signed up to take a 22-hour online training course on the UP. Data collection was carried out by means of an on-line questionnaire through the Qualtrics platform. Once the professionals had completed the UP training course, a link appeared where they were invited to participate in the completion of a brief questionnaire; once they accessed it, the information and informed consent form appeared, and, once accepted, the questionnaires included in this study appeared. The questionnaires were programmed to appear successively according to the answers given by the professionals; thus, those professionals who answered "Health Psychology" to the question "area of work" were allowed to continue advancing in the questionnaire. All those who did not mark the option "Health Psychology" ended the survey. Similarly, the questionnaire of acceptability and intention to use it in the future was adapted according to the option "experience in the application of the UP with patients".
The survey took approximately 5 to 10 minutes to complete. The anonymity, confidentiality and data protection of all participants were guaranteed. Finally, it was noted that participation was completely voluntary, and participants could leave the study at any time. The study was approved by the ethics committee of Aragon (Nº 07/2021).
Statistical analysis
First, analyses of normality (through the Kolmogorov Smirnov test) were carried out to analyze whether the participants' data followed a normal distribution.
Next, the sociodemographic characteristics of the participants were analyzed through descriptive analyses of the degree of knowledge of the transdiagnostic approach and the UP, both overall and in each of the subgroups. In addition, the Mann-Whitney U-test was performed to analyze whether there were statistically significant differences in the scores between professionals with experience in the use of the UP and those without experience in the use of the UP.
Following this procedure, the means and standard deviations obtained in each of the acceptability and intention to use constructs were analyzed and, again, the Mann-Whitney U-test was performed to analyze whether there were statistically significant differences in the acceptability and intention to use scores between the two subgroups.
Finally, using Spearman's rho test, the relationships between sociodemographic variables, acceptability constructs and intention to use the UP in the future were analyzed. These analyses were carried out in general and in both subgroups of professionals, experienced and inexperienced in the use of the UP, with the aim of seeing which variables were most related to acceptability and intention to use the UP in future with the objective of promoting the implementation of the UP in this profile of professionals.
All statistical analyses were carried out using the IBM SPSS Statistics version 23 statistical package (Corp, 2013).
Results
Normality test results
The results of the Kolmogorov Smirnov normality test showed that the data did not follow a normal distribution (p < .05) so nonparametric statistical analyses were performed.
Knowledge of transdiagnostic treatments and UP treatment
In general, the mean score obtained by the GHPs on the degree of knowledge of transdiagnostic treatments was 2.27 out of 4 (SD = 0.78, range 1 - 4) and 2.04 out of 4 (SD = 0.78, range 1 - 4) on the degree of knowledge of the UP. If we compare between groups, the subgroup formed by professionals with experience in the use of the UP presented a degree of knowledge of transdiagnostic treatments of 2.85 out of 4 (SD = 0.60, range 2 - 4) and 2.89 out of 4 (SD = 0.70, range 2 - 4) in the degree of knowledge of the UP. On the other hand, the group of professionals with no experience in the use of the UP reported a degree of knowledge in the transdiagnostic approach of 2.15 out of 4 (SD = 0.77, range 1 - 4) and 1.86 out of 4 (SD = 0.87, range 1 - 4) in terms of the UP. The Mann-Whitney U-test showed statistically significant differences in both the degree of knowledge of the transdiagnostic approach (Z = 863.00, p < .001) and knowledge of the UP (Z = 652.50, p < .001) in favor of the group with experience in the application of the UP. No statistically significant differences were found in age, sex or in the rest of the sociodemographic variables (p > .05).
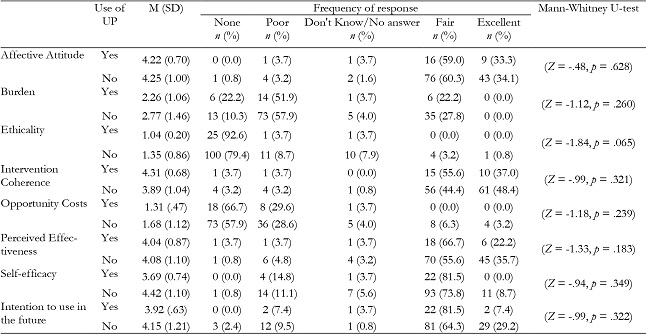
Acceptability results and intention to use in the future
The means, standard deviations and response frequencies of the acceptability and intention to use the UP in the future constructs by the two subsamples can be seen in Table 2. Overall, the mean scores obtained were: Affective attitude (M = 4.29, SD = 0.61); Burden (M = 2.44, SD = 1.03); Ethicality: (M = 1.24, SD = 0.63); Intervention coherence (M = 4.40, SD = 0.68); Opportunity Costs (M = 1.53, SD = 0.80); Perceived Effectiveness (M = 4.21, SD = 0.78); Self-efficacy (M = 3.79, SD = 0.77) and Intention to use in the future (M = 3.96, SD = 0.87). No statistically significant differences (p > .05) were found in the scores between the subgroups of GHPs with and without experience in the use of UP.
Relationship between sociodemographic variables, acceptability, and intention to use in the future
The results of the Spearman's rho test in general can be seen in Table 3. If we analyze the results according to the subgroup, we find, with respect to the sociodemographic variables, a positive and statistically significant mean relationship between the transdiagnostic knowledge variable and Perceived Effectiveness (rs = .44, p = .025) in the GHPs with experience in the use of the UP. On the other hand, in those GHPs without experience, we found a statistically significant negative low relationship between the variable age and the variables: Affective Attitude (rs = -.21, p = .023) and Ethicality (rs = -.19, p = .042). A low positive relationship was also found between transdiagnostic knowledge and Affective Attitude (rs = .18, p = .046) and Intention to use in the future (rs = .29, p = .001). Finally, there was a low positive relationship between knowledge of the UP with Affective Attitude (rs = .23, p = .012), Ethicality (rs = .19, p = .037) and Self-efficacy (rs = .18, p = .046).
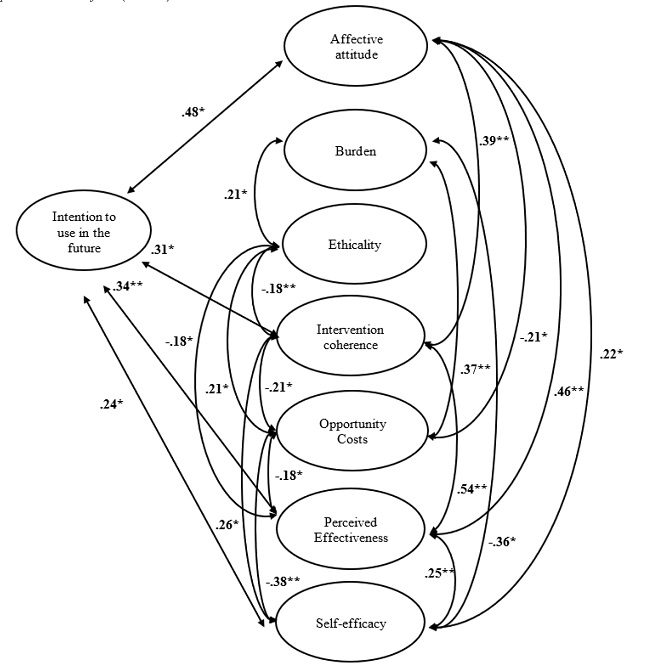
The relationship between different TFA constructs and intention to use in the future in the subgroups of GHPs with and without experience in the use of the UP were considered, as can be seen in Figures 1 and 2. For the group of GHPs with experience in the use of the UP, the results of the Spearman's rho test showed a low-moderate positive relationship between Affective Attitude and the variables Burden (rs = .39, p = .042) moderate-high positive with Intervention Coherence and Perceived Effectiveness (rs = .63, p = .001 and rs = .74, p < .001, respectively) and moderate positive with Intention to use in the future (rs = .48, p = .014). A moderate positive relationship between Burden and Perceived Effectiveness (rs = .39, p = .048). A high positive relationship between Intervention Coherence and Perceived Effectiveness (rs = .73, p < .001) and Intention to use in the future (rs = .50, p = .010). A moderate negative relationship was also found between the variables Opportunity Costs and Perceived Effectiveness (rs = -.41, p = .038). Finally, a moderate positive relationship was found between Perceived Effectiveness and Intention to use in the future (rs = .56, p = .003).
Table 3: Spearman's rho test results showing the relationship between the study variables (N = 153).
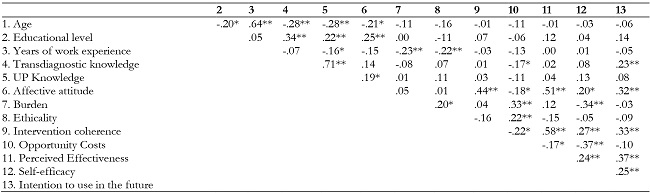
Note:** p < .001;
*p < .05.
UP: Unified Protocol
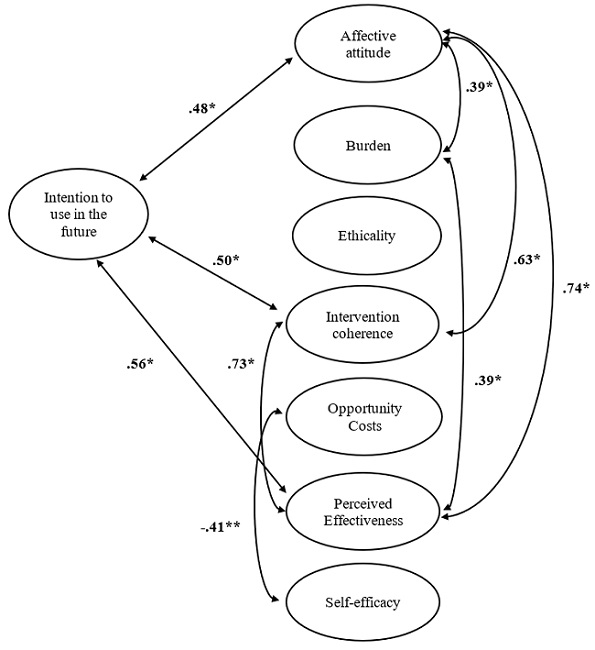
Figure 1. Relationship between the intention to use the UP in future and the different constructs that form the Theoretical Framework of Acceptability (TFA) in the sample of GHPs with experience in the use of UP (n = 27).
Regarding the subgroup of GHPs with no experience in the use of the UP, the results of Spearman's rho test showed a low-moderate positive relationship between Affective attitude and the variables: Intervention Coherence (rs = .39, p < .001), Perceived Effectiveness (rs = .46, p < .001), Self-efficacy (rs = .25, p = .013) and Intention to use in the future (rs = .30, p = .001) and a low negative relationship with Opportunity Costs (rs = -.21, p = .019). A low-moderate positive relationship was found between the variables Burden and Ethicality (rs = .21, p = .018), Opportunity Costs (rs = .37, p < .001) and low-moderate negative relationship with Self-efficacy (rs = -.36, p < .001). A statistically significant low negative relationship was also found between the variables Ethicality and the variables Intervention Coherence (rs = -.18, p = .046) and Perceived Effectiveness (rs = -.18, p = .050) and low positive with Opportunity Costs (rs = .21, p = .022). The variable Intervention Coherence was low-moderately positively related to the variables Perceived Effectiveness (rs = .54, p < .001), Self-efficacy (rs = .26, p = .004) and Intention to use in the future (rs = .31, p = .001) and low negatively related to Opportunity Costs (rs = -.21, p = .018). Opportunity Costs correlated low negatively with Perceived Effectiveness (rs = -.18, p = .042) and Self-efficacy (rs = -.38, p < .001). Finally, the variable Perceived Effectiveness correlated low positively with the variables Self-efficacy (rs = .25, p = .005) and Intention to use in the future (rs = .34, p < .001) and there was a low positive correlation between the variables Self-efficacy and Intention to use in the future (rs = .25, p = .006).
Discussion
The objectives of this study were, firstly, to determine the degree of knowledge that the GHPs had about transdiagnostic treatments and, specifically, the degree of knowledge about the UP. The results indicated a low-medium knowledge of transdiagnostic treatments and specifically of the UP. In fact, the results showed that 15.7% had no knowledge of the transdiagnostic approach and 33.3% had no knowledge of UP at all. Moreover, despite the fact that the UP is a EBPTs, its use is not yet widely established, in fact, only a small part of the sample (n = 27) had put it into practice in therapy. One explanation to clarify these results could be the importance of the theoretical orientation of each psychologist, as this is a determining factor when using EBPTs (Gyani et al., 2014). Another explanation could be the still recent publication of the UP manuals in Spanish, with the first edition being published in 2015, so it may still be an unknown intervention for a large part of the GHPs.
Regarding the second objective, to evaluate the degree of acceptability and intention to use the UP, the results showed high scores in most of the constructs that make up the TFA model. Likewise, high scores were found in the intention to use the UP in the future in GHPs who had previously used the UP and those who had not used it. These results were also obtained in the study by Peris-Baquero et al. (2021), where a high acceptance was found, in all its constructs, by Psychologists Specialized in Clinical Psychology working in the public context. Similarly to that study, the present study also found high scores in intention to use it in future both in GHPs who had used the UP (i.e., to continue using it) and also in those who had never used it before. It should be noted that no statistically significant differences were observed between the two groups. This suggests that perhaps practical experience is not a determining factor when evaluating a treatment as acceptable or when clinicians agree to use it in future. In this sense, results seem to highlight the importance of carrying out adequate training with the aim of making EBPTs known among professionals so that they are accepted and used in future, to achieve their implementation in the routine practice of professionals.
Finally, in relation to the third objective, to analyze the relationship between sociodemographic factors and the different constructs of the TFA with the intention to use the UP in future. The results showed that, in general terms, older people had a lower knowledge of the transdiagnostic approach and showed a lower affective attitude towards it. These results were observed in those GHPs with no experience in the application of the UP but not in those with experience in its application. These results are in line with previous work indicating that younger professionals have a more positive attitude towards the adoption of EBPTs (Aarons & Sawitzky, 2006) but are contrary to those obtained by Peris-Baquero et al. (2021), where age correlated positively and statistically significantly with the intention of future use in those Psychologists Specialized in Clinical Psychology with experience in the use of the UP. It seems that age has different associations with intention to use the UP in future or some aspects regarding the TFA when professionals are working in the public or private sector in Spain. Psychologists Specialized in Clinical Psychology working in public settings are incentivized economically and with days-off work if they increase their training and participate in research in the clinical psychology field. This is not happening in the private sector.
Regarding the level of education achieved, the results of this study found that a higher level of education is associated with a greater knowledge of transdiagnostic treatments, a greater knowledge of UP and a greater affective attitude towards UP. These results are similar to those found by Aarons (2004) and by Beidas & Kendall (2010), which indicate that educational level is positively related to the use of this type of treatments.
Similar to age, it has been found that the higher work experience is associated with lower knowledge of the UP. This could be due to the newness of the first UP manual published in Spain in 2015, which would be reflected in the fact that those with more work experience apply another type of therapy protocols compared to those professionals who are beginning and who could make use of more recent therapies that they have received training in. Another aspect to highlight is that the greater the work experience the less ethical consequences and effort the GHPs perceive they will need to apply it, so those more experienced professionals consider the UP as an easier intervention to apply and with fewer ethical consequences in its application than those professionals with less experience.
We also analyzed the relationship between intention to use the UP in the future and the constructs that make up acceptability in GHPs who had and had not previously used the UP. On the one hand, intention to use (in GHPs who had used the UP) correlated with the constructs: Affective Atittude, Intervention Coherence and Perceived Effectiveness. On the other hand, intention to use (in GHPs who had not used the UP) correlated with Affective Atittude, Intervention Coherence, Perceived Effectiveness and Self-efficacy. This indicates the importance of the affective attitude towards the treatment, regardless of the experience in its application, the treatment being perceived as pleasant is related to the intention to use it in the future (Joosten et al., 2008). Similarly, consistency with the Intervention Coherence and Perceived Efficacy are also present in both subsamples. This indicates that for all participants, the theoretical approach by which the UP achieves improvements in patients' emotional regulation and the efficacy of the UP in helping patients to regulate their emotions are associated with their intention to use the UP in the future. These results are also found in the research conducted by Peris-Baquero et al. (2021), specifically the relationship between intention to use in the future with Affective Atittude and Intervention Coherence. Finally, in the group of inexperienced GHPs a relationship was also found between Self-Efficacy and intention to use in the future. This result suggests that professionals need to feel competent in the application of the treatment in order to use it in the future, which raises the need to carry out adequate training that allows professionals to acquire the necessary skills to be able to apply it with solvency. The fact that GHPs who had not previously used the UP responded in acceptability and intention to use it in a very similar way to those who had already used it, reflects the idea that the UP is a very accepted intervention. Moreover, once it is put into practice, most GHPs claim that they would use it again in the future, therefore, these constructs have to be taken into account for a good implementation in the future.
Finally, the way in which the TFA constructs are related is different depending on the experience in the use of the UP, although there were no statistically significant differences in the TFA scores between groups. For those GHPs without experience, the results indicated that some considerations must be implemented in the training such as: (1) placing special emphasis on increasing the Affective Attitude towards the UP, for example, explaining in detail the coherence of the intervention and the efficacy of the treatment, explaining each of the techniques and getting them involved through examples with their own patients or by means of role playing techniques so that the professionals feel effective when applying the treatment. (2) In addition, UP trainers should consider explaining in their workshops the effort involved in applying it or the consequences or loss of opportunities associated with its election.
Despite the interesting findings obtained in this study, it also presents a set of limitations. Firstly, the results obtained should be interpreted with caution given that they correspond to a sample of GHPs and, consequently, the results obtained cannot be generalized to other health professionals. Secondly, as previously mentioned, the UP has recently been translated into Spanish so, until relatively recently, it was not an accessible or known treatment in Spain for non-English speakers. Thirdly, the training course was offered in the Professional College of Psychology of Aragon, and, although some participants were GHPs from other autonomous communities, most GHPs belonged to the to the Autonomous Community of Aragon, which also influences the representativeness of the results. Fourthly, the theoretical orientation of the psychologists who participated in the study was not registered, and this factor can be determinant in the use of the EPTBS. Fifthly, the sample size in both subsamples was not equal, nor was the distribution of women and men. Finally, social desirability must be considered, as it may have influenced the answers given by participants.
Considering these limitations, future studies should be implemented in this field. On the one hand, future studies should be aimed at finding out the use/knowledge of the UP by adding, also, the methods used by psychologists to keep themselves informed about updates in EBPTs (i.e., training courses, congresses, scientific journals, articles, etc.). On the other hand, the same study should be carried out in other Autonomous Communities, in order to be able to compare results with a larger sample and, therefore, be more representative of the GHPs in Spain. Also, there should be additional research on the acceptability and intention to use the UP, since, as has been mentioned, there are hardly any studies on this subject. Once the UP has been more widely disseminated and used, it will be necessary to study the GHPs’ opinion regarding advantages and disadvantages/barriers to using the UP in their workplaces (private offices, community services, private hospitals, etc.). Finally, future studies should analyze in detail what sociodemographic factors influence the use of the UP, in order to direct and adapt future training.
In summary, this study has evaluated the use, acceptability and degree of implementation of the UP in clinical practice in a sample of GHPs in Spain. The main results have shown a high acceptability and intention to use the UP in the future by GHPs. This is important, as high scores on these constructs would reinforce the idea of continuing with UP training courses for GHPs. In addition, the use/knowledge of EBPTs, such as UP, is very limited. Finally, although there is a high acceptability and high percentage of intention to use UP in the future, it is still necessary to know in depth those factors that may influence its implementation and take them into account in future UP trainings and thus ensure the correct dissemination of this EBPT.