Introduction
Loneliness is a subjective, unpleasant experience that implies a discrepancy between the desired and actual social relationships experienced by a person (Yanguas et al., 2018). For some years now, it has been recognized as one of the psychosocial risk factors for physical and psychological health (Giné-Garriga et al., 2021). Some authors have concluded that loneliness can worsen quality of life, cause suffering and be considered a risk factor for health or negative health outcomes including mortality (Courtin & Knapp, 2017), affecting well-being and cognitive functioning of older adults (Ayalon, 2018). The same phenomenon has been contemplated within the screening criteria for the detection of frail older adults in primary care (Lesende et al., 2010). It has been highlighted its two-dimensional character, understanding the existence of emotional loneliness (lack of close emotional ties) and social loneliness (deficient social network, lack of relevance to a group). The latter has also been defined from a humanistic and social perspective as social isolation derived from the absence of a relationship with family or friends on whom to rely in case of need (Machielse, 2015).
The feeling of loneliness can appear at any stage of old age, related with various losses that can occur, such as moving into a Nursing Home (NH) (Gardiner et al., 2020a). In Spain, according to data from the Spanish Government portal "Envejecimiento en red", in 2019 322,180 people aged 65 years or over were living in NHs, accounting for 85% of the total number of places (Abellán, A. et al., 2019.). This highlights the possibility of finding an over-aged population in this setting with the presence of physical limitations, chronic conditions, and cognitive and psychological impairments is common and the likely presence of unwanted loneliness might be highly prevalent (Jaul & Barron, 2017; Semra et al., 2019).
The risk factors associated with loneliness during the aging process are diverse. The sociodemographic factors of greatest risk include being a woman, advanced age, low educational level, not having a partner or being widowed, not having children (Cotterell et al., 2018; Luchetti, M et al., 2020) and the environment of the NH (Chen & Shea, 2004). Regarding physical and psychological health conditions, the presence of comorbidity, loss of mobility, functional decline, as well as depression (Cohen-Mansfield et al., 2016; Gale et al., 2018) represent health and psychological factors associated with higher levels of loneliness. A longitudinal study on aging in the Canadian population suggested that dementia could be developed 1.6 times more in people with high levels of loneliness compared to individuals with a preserved social network (Gilmour & Ramage-Morin, 2020). The same phenomenon has also been associated with impaired cognitive status, alterations in the immune system, increased blood pressure and mortality (Chamberlain et al., 2018; Muntsant & Giménez-Llort, 2020). Furthermore, a meta-analysis showed that the risk of mortality due to alcohol use disorder and smoking is comparable to the risk of death associated with loneliness, and with more harmful effects on health than the factors associated with obesity (Leigh-Hunt et al., 2017)
Living in NHs was associated with higher degrees of loneliness and that loneliness may increase the risk of admission to a NH (Hanratty et al., 2018). It has also been considered that changes in the social networks (family and/or friends) of older people who move into a NH may also be involved in loneliness (Cohen-Mansfield et al., 2016). The residents of these institutions are often female, with low socioeconomic status and have diminished cognitive status, which coincide with some of the risk factors associated with loneliness (Penninkilampi et al., 2018; von Soest et al., 2020). On the other hand, evidence indicates that frailty may be a risk factor for loneliness and social isolation, due to low social connections (Cohen-Mansfield et al., 2016). Even though it is known that loneliness is associated with an increased risk of mortality a (Cohen-Mansfield et al., 2016; Andreasen J. et al., 2015) interventions aimed at its prevention or reduction of loneliness in NHs are remarkably scarce.
Although the phenomenon of loneliness in aging has received attention in the scientific literature, most studies have focused on older people living in the community; and research in the context of NHs is scarce (Gardiner et al., 2020a). There are few studies considering the risk factors associated with loneliness in older NH residents and far fewer studies analyzing resident's emotional and social loneliness, and possible associated physical, psychological, and social factors. Therefore, the main aim of this study was to verify the associated factors (psychological, social, and physical health) with overall, social, and emotional loneliness and as a specific objective to verify the prevalence of this phenomenon among older adults living in NHs of the Osona region (Barcelona, Spain).
Materials and Methods
Design
This is a multicenter cross-sectional study, which was conducted in 5 NHs in the Osona region (Central Catalonia region, Barcelona province, Spain), of which three had state subsidized places and two were totally private. It is a sub-study of the OsoNaH project (Farrés-Godayol et al., 2021) registered in Clinical Trials (CNT04297904). The study followed the standards of STROBE (Strengthening Reporting of Observational studies in Epidemiology) guidelines for cross-sectional studies (von Elm et al., 2008) and met the criteria required in the Helsinki Declaration, as well as the Spanish Organic Law 3/2018 (December 5) on the Protection of Personal Data and Guarantee of Digital Rights. The project was approved by the Ethics Committee and Research (CER) of University of Vic-Central University of Catalonia (UVic-UCC) (registration number 92/2019 and 109/2020) and Clinical Research Ethics Committee of the Osona Foundation for Health research and Education (FORES) (code 2020118/PR249).
Participants
All the residents aged 65 years or over with who were living permanently in NHS were included, and those in palliative care and who refused to participate in the study were excluded. In addition, for the present loneliness sub study, participants were excluded if they had severe cognitive impairment, which prevented them from understanding and responding to the assessment questionnaires. All NHs were contacted by e-mail and telephone offering them the possibility of collaborating in the study. A document explaining the project was sent together with a formal consent document, which was signed by the director of each NH if they accepted to participate in the study. The participants were selected according to the inclusion criteria, from a list of the residents which was obtained by the NH's Directors; and a simple randomization was done with the IBM SPSS Statistics software (IBM Corp. Released 2021. IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp). Residents were informed that their data would be treated anonymously and that they could withdraw from the study at any time without giving any explanation. Both the residents and the NHs professionals received detailed information about the project and provided informed consent of acceptance. The research team received training through standard operating procedures to ensure the reliability of the data.
Variables and measurement instruments
The dependent variable of the study was the presence of loneliness (yes/no), collected using the 6-item De Jong Gierveld Loneliness Scale (DJGLS-6, Spanish version) (Gierveld & Van Tilburg, 2006). This reduced version consists of 3 items for each of the two subscales: for social loneliness, referring to the feeling of missing a wider social network, and for emotional loneliness, referring to missing a "more intimate relationship". There are negatively worded items, in which the neutral and positive responses (plus or minus and yes) and the "no" response with 0; and in the positively worded items, the neutral and negative responses (plus or minus and no) are scored with 1 and the yes response with a 0. This gives a total score range of 0 to 6, which can be interpreted from the lowest to the highest levels as "less alone or more alone". However, in the present study, to define the presence of loneliness levels, scores between 0 and 2 were considered normal, and scores above 2 were considered as a cut-off point, in line with authors of previous studies on older adults living in NHs (Jongenelis et al., 2004; Lubben et al., 2006; M. E. Prieto-Flores et al., 2011; Victor, 2012).
Several psychosocial factors were also collected from the residents, such as the number of visits they received monthly from family and/or friends, and the following variables described below: the reduced version of the Lubben Social Network Scale (LSNS-6) was used to measure the presence and degree of social isolation, which presents 3 items regarding family ties and 3 regarding friendly relationships (Lubben et al., 2006). The maximum score of the scale is 30 and 12 can be used as a cut-off point to consider the presence of risk of social isolation of the participants. The lower the perceived social support from family and/or friends, the higher the risk of social isolation for the person (Lubben et al., 2006). The EuroQoL-5D (EQ-5D-5L), consists of a self-description of current health-related quality of life (QoL) on five domains: mobility, self-care, usual activities, pain/discomfort, and anxiety/depression (Ramos-Goñi et al., 2018). Each dimension has five response levels: no problems, slight, moderate, severe problems, unable to/extreme problems. Total of 245 combinations representing health states, which are from 11111 (the best health state) to 55555 (the worst health state), or it can also be converted into a single index “utility” score using a scoring algorithm based on public preferences (Rabin & De Charro, 2001), of a country or region. These weights lie in a range in which full health has a value of 1 and death a value of 0. The cross-index values for the scores of each dimension can be calculated with the "EQ-5D-5L" crossover tool (available on the EuroQol website) (Ramos-Goñi et al., 2018); which are shown as the set of standard values for Spain divided by the value 0.5, corresponding to the mean of the range of possible values. The reduced and Spanish version of the Yesavage Geriatric Depression Scale (GDS) was used to measure the presence or absence of depressive symptoms, with scores above 5 being considered as an indicator of possible depression (Ortega Orcos, R. et al., 2007). The anxiety subscale of the Anxiety and Depression Scale (HADS), which considers scores above 8 as possible cases of anxiety and scores above 11 as cases of anxiety, was used to collect the presence of anxious symptomatology (Herrero et al., 2003). The cognitive capacity of the participants was verified using the Pfeiffer SPMSQ Scale (Short portable Mental State Questionnaire) which briefly evaluates functions such as orientation, memory, concentration, and arithmetic, and by which the inclusion of participants was decided (people with severe cognitive impairment were excluded according to the questionnaire). The instrument allows classification of older adults (≥ 65 years) according to their preserved mental function, mild, moderate, or severe cognitive impairment, considering the educational level of the person being evaluated (Martínez de la Iglesia et al., 2001).
To record the presence of UI (yes/no), section H of the minimum data set (MDS) version 3.0 was applied according to the answers given by the proxy (Klusch, 2012) and the international consultation on incontinence questionnaire urinary incontinence-short form (ICIQ-SF) (Espuña Pons et al., 2004) which assesses the quantity and frequency of urine leakage and the impact on the individual's QoL. The responses provided by the residents were compared with those of the proxy using the MDS. Functional independence was measured using the Barthel Index modified by Shah et al., 1989, excluding the continence items, as covered by MDS 3/5/2024 5:48:00 PMes (Espuña Pons et al., 2004; Shah et al., 1989). The frailty status of the participants was assessed using the clinical frailty scale (CFS), which places the person in one grade or another, depending on the information provided by the caregiver about mobility, functionality, and cognition (Rockwood et al., 2005). Physical performance was recorded using the brief physical performance battery (SPPB), measuring hand grip strength with the JAMAR Plus Digital Hand dynamometer (Sipers et al., 2016) positioning the elbow at 90° of flexion (Guralnik et al., 1994). The result was adjusted for gender and body mass index and was the highest value recorded with the dominant hand after 3 repetitions with both hands. To quantify mobility, the Rivermead Mobility Index (RMI) was used, which presents self-reported and directly observed elements (Collen et al., 1991). To measure the risk of sarcopenia, the SARC-F screening questionnaire was used, based on 5 components: strength, assistance with walking, rise from a chair, climb stairs, and falls (Sánchez-Rodríguez et al., 2019). The body mass index (BMI) was measured with a Seca 213 measuring device (Seca Medizinische Messsysteme und Waagen, Hamburg, Deutschland), the Tanita TBF-300 bioimpedance device (Tanita Institute. Tokyo, Japan). Using the Mini Nutritional Assessment (MNA) screening tool, participants' nutritional status was assessed by classifying them into different categories within a maximum score of 30 points: (score < 17) malnourished, (17 - 23.5) at risk of malnutrition and normal (≥ 24) nutritional status (Vellas et al., 1999). Sedentary behavior was assessed by the gold standard activPAL3 activity monitor (Grant et al., 2008) (PAL Technologies Ltd., Glasgow, UK) device worn by participants on the thigh, which distinguishes, and records time spent sitting, standing, and walking during 7 consecutive days (Lyden et al., 2017).
For each participant, information was collected on sociodemographic (age, gender, educational level, marital status, number of children, type of NH and time of institutionalization), on health conditions (medication intake, presence of chronic diseases, tobacco and alcohol, functional and cognitive capacities) - and the collection of diagnosed diseases for residents: urinary incontinence (UI), fecal incontinence, depression, renal insufficiency, chronic pain, hypertension, hypothyroidism, dyslipemia, mental illness). This information was collected through the clinical history of the residents and checked with a NH professional (auxiliary, nursing technician or physiotherapist).
Procedure
Data collection began in January 2020 and stopped due to the onset of the COVID-19 pandemic in March 2020. The final sample consisted of 65 individuals. Considering a significance level of 0.05 and power of 0.80, this sample size can detect at least 6.2 points of difference of proportions between cases of loneliness among independent variables (e.g., 76.2% and 70.0% cases of overall loneliness in non-private and private NHs, respectively) (Lwanga et al., 1991).
Statistical analysis
The statistical analysis was carried out with the IBM SPSS Statistics software program (IBC Corp. Released 2021.IBM SPSS Statistics for Windows, Version 28.0. Armonk, NY: IBM Corp). First, data were presented through descriptive statistics; categorical variables were shown as absolute frequency and percentages. Continuous variables were presented as means and standard deviations or as medians and interquartile range. To contrast the normality of the data set, the Shapiro-Wilk test was used; for parametric variables the student's t-test and for nonparametric variables the U-Mann Whitney test were used. We calculated the absolute frequency and percentage of the different types of loneliness variables: overall, emotional, and social loneliness, unadjusted odds ratio (OR) and their 95% confidence interval (CI) according to potential variables to verify the magnitude of the association. Categorical data were compared using Chi Square test or Fisher's exact test. Finally, logistic regression was used to test potential associations between residents reporting loneliness and independent variables, controlled by principal confounders: sex and age. All variables with p-values under .20 were tested in the multivariate analysis using the forward method. A value of p ≤ .05 was considered statistically significant and CIs were at 95%.
Results
The final sample consisted of 65 residents from the 5 including NHs. (See Figure 1).
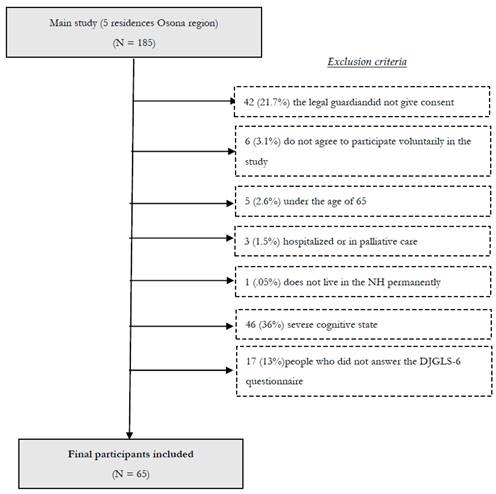
Figure 1. Flowchart of the cross-sectional study with the final sample according to exclusion criteria.
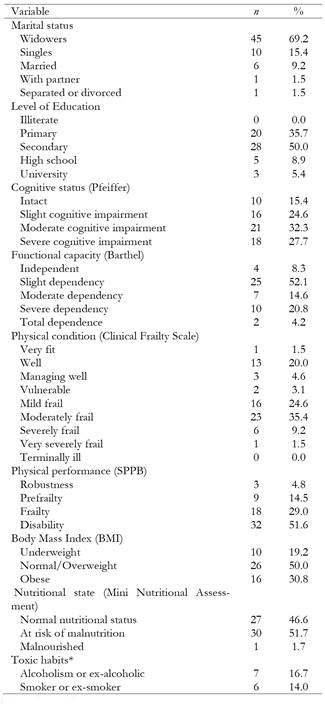
Of the final sample of 65 residents, 53 (81.5%) were women, with a mean age of 83.9 (SD: 7.45) and mean number of children of 1.6 (SD: 1.54); 50 (76.9%) lived in private with state-subsidized places NHs and 15 (23.1%) in private NHs. (See Table 1).
Table 1. Descriptive analysis including sociodemographic and health-related information of institutionalized older people in Osona region (Barcelona, Spain), 2020.
Concerning the psychosocial variables, 46 participants (70.8%) suffered from overall loneliness, scored on the loneliness dimension, 17 (26.2%) of social loneliness, and 12 (18.3%) of emotional loneliness according to the De Jong Gierveld Loneliness Scale (DGLS-6). Regarding the participants' risk of social isolation, 25 (40.3%) were at high risk of social isolation, 13 (21%) at low risk, and 24 (38.7%) not at risk of isolation. Regarding the number of visits received per month from family and/or friends (median) was 8 (Range: 3-16). According to the GDSVE-6 questionnaire for rapid screening of depressive symptoms, 55 (84.6%) of the residents had symptoms, and 15 (23.8%) were probable cases of anxiety according to the subscale of the HADS questionnaire for assessment of anxious symptoms. In addition, the results of the EQ-5D-5L showed that the percentages of residents who did have problems or difficulties for each of the dimensions were: problems with mobility (71%), self-care (63%), usual activities (46%), pain/discomfort (58.5%) and anxiety/depression (46%).
Residents had significant co-morbidities, presenting with a mean of 5.2 (SD: 2.34) diagnosed conditions, with 41 (63.1%) having five or more. Specifically: 44 (67.7%) arterial hypertension, 28 (43.1%) heart disease, 26 (40%) dementia, 22 (33.8%) both dyslipidemia and diabetes, 16 (24.6%) delirium, 14 (21.5%) lung disease, 13 (20%) strokes, 11 (16. 9%) digestive, circulatory, and mental illnesses, 10 (15.4%) Parkinson's and cancer, 9 (13.8%) osteoporosis, 7 (10.8%) arthrosis and anemia, 5 (7.7%) anxiety, chronic pain, and visual deficit and 2 (3.1%) ulcers and epilepsy. In addition, 41 (65%) had UI and 11 (17%) fecal incontinence. The presence of obesity (BMI > 23) was observed in 45 (69%) participants and risk of malnutrition or in malnutrition in 26 (4%) individuals of them and 8 (12.3%) presented weight loss in the last year.
With respect to the medication, the use of one or more drugs from the following groups was observed: analgesics and psycholeptics in 45 (70%), psychoanaleptics in 40 (63%), antiepileptics in 11 (17%) and antiparkinsonians in 10 (15.6%) participants. There was a mean of 8.82 (SD: 1.6) and 79.4 (SD: 15.8) for the hours and total percentage of sedentary behavior respectively. 49 (84.5%) residents were at risk of sarcopenia and 23 (45%) of them had fallen in the previous year.
Associated factors and prevalence of the main study variables (overall, emotional, and social loneliness)
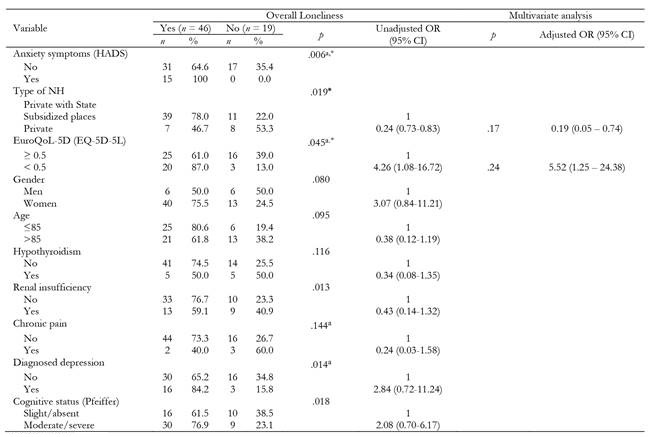
Overall loneliness
The prevalence of perceived loneliness was 70.7% (95% CI: 58.2-81.4). There was a significant difference according to the type of NH: the prevalence in private NHs was 46.6% vs. 78.0% in those with State subsidized places. The other variables that were significantly associated with loneliness were lower levels of perceived health related QoL, and anxiety, with 100% of residents with anxious symptoms presenting feelings of loneliness. There was no significant association with the rest of the variables. (See Table 2). The relevant factors from the previous bivariate analysis were selected to adjust the multiple logistic regression, also adjusting for the confounding variables sex and age. The results showed that the type of NH and perceived QoL remained factors associated with overall loneliness. The goodness of fit of the logistic regression model was p = .861 for the Hosmer-Lemeshow test.
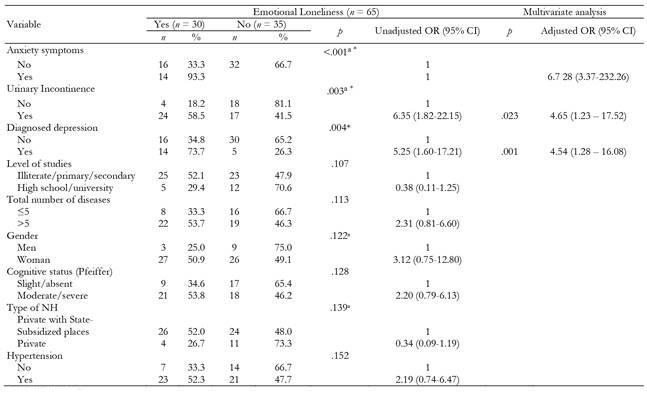
Emotional loneliness
For emotional loneliness, the diagnosis of depression was statically significant; with a prevalence of emotional loneliness of 73.6% in residents diagnosed with depression, compared to 34.7% in those without the disorder. Other conditions that were significant were: anxiety symptoms and UI, with 58.5% of residents with anxiety compared to 18.18% in those without anxiety. There was no significant association with the remaining variables. (See Table 3). Depression and UI were significantly associated with emotional loneliness in the final model, with a p = .721 in the Hosmer-Lemeshow test.
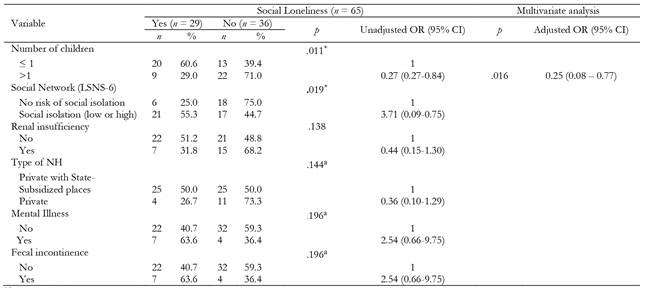
Social loneliness
The prevalence of social loneliness was 44.6% (95% (CI): 33.1 - 56.6). The bivariate analysis showed that having no children or only one child was an associated factor for social loneliness, with a prevalence in residents without children or with only one child of 60.6%. The other variable that was significant was being at risk of social isolation. (See Table 4). The logistic regression showed that the condition of having only one child or not having one was an associated factor in the final model (Hosmer-Lemeshow test p = .959).
The present study showed a significant association between the presence of loneliness and the presence of poor self-reported QoL. This association has been shown before (Jansson, A.H. et al., 2017) QoL is often reported as better in older people living in the community compared to those living in NHs (M.-E. Prieto-Flores et al., 2011.). Other recent studies postulated that the QoL of older NH residents was lower, the greater the sense of loneliness (Gerino et al., 2017; Trybusińska & Saracen, 2019). QoL can be impacted by the quality of the care received in a NH, for example, the degree of dependency of older adults, combined with the staffing level, the facilities, and the typology of the center (private or NH with state subsidized places) (Gardiner et al., 2020a). In addition, poorly qualified staff and many occupied beds can diminish both the care received and the quality of care and QoL (Harris-Kojetin et al., 2016).
Discussion
The objective of this study was to determine the associated factors with loneliness in older adults institutionalized in NHs and, in turn, to identify the prevalence of this phenomenon. The results found that the factors associated with the presence of feelings of loneliness were the type of residence and the poor perception of health-related quality of life. In addition, a diagnosis of depression and UI were associated with emotional loneliness and having a child or not having a child and being at risk of isolation were associated with social loneliness. Data collected showed high prevalence of global loneliness, as well as emotional and social loneliness (70.7%, 46.2% and 44.6% respectively).
Over the years, several investigations from different geographical areas of the world found higher rates of loneliness among older adults residing in NH (Aung et al., 2019.; Drageset et al., 2013; Herman, A. et al., 2018). A prevalence of loneliness like ours (71.6%) was found in in people over 60 years old living in Spanish NHs (M. E. Prieto-Flores et al., 2011). A qualitative systematic review with 10 studies examining the social relationships of institutionalized older adults in NH noted a high prevalence of loneliness, specifically, emotional loneliness (Mikkelsen et al., 2019). Another recent systematic review, considering 13 studies on the prevalence of loneliness in NH's residents, showed slightly lower rates compared to those in our study (61% and 35% of severe loneliness and moderate loneliness respectively) (Gardiner et al., 2020b). There are, however, very few studies specifically on the prevalence of emotional and/or social loneliness in NHs (Amzat & Jayawardena, 2015; Drageset et al., 2012; M. E. Prieto-Flores et al., 2011) compared to research of overall loneliness among older adults in the community (Ausín et al., 2017).
Some of these factors can differentiate a private NH from a public NH, or one with many States subsidized places. Of course, even with the risk of loneliness in some state subsidized NHs, the wide range of health care, personal care, and long-term support services they offer may also prove to be protective factors for the maintenance of the health of their residents (Harris-Kojetin et al., 2016). Some institutions prioritize person-centered care by attending to psychosocial aspects and by ensuring their NH facilities, as much as possible, are a home which may help improve QoL and reduce loneliness (Andrew & Meeks, 2018). Encouraging this person-centered care and social relationships in institutionalized older adults are fundamental from the perspective of healthy aging, because they can contribute to well-being and (Tran et al., 2019) to combat emotional and social loneliness during the stay in NH by increasing their QoL (Bowling & Iliffe, 2011).
One recent study showed a significant correlation between loneliness and mental health, especially with depressive symptoms. The results of our study also postulate a significant association between the perception of emotional loneliness and the presence of mental health problems; specifically, with the diagnosis of depression. These findings are consistent with the conclusions of previous studies (Drageset et al., 2013; Peerenboom et al., 2015), which showed a relationship between depression in older adults and the presence of emotional loneliness, but not social loneliness. Unlike our study, one study also showed an association between loneliness and depressive symptomatology collected by the GDSVE-6 screening, which we also used in our study (M. E. Prieto-Flores et al., 2011). Other recent research in depressed older adults showed loneliness as a risk factor, associated with both cognitive impairment and elevated mortality (Holwerda et al., 2016).
Ausín et al. (2017) identified several variables as predictive of loneliness in Spanish adults over sixty-five years of age, including functional deterioration and low satisfaction with QoL and social contacts, and the presence of mental disorders, especially anxiety (Ausín et al., 2017). In our study sample, all residents with anxious symptomatology also presented feelings of loneliness. These results are consistent with those found in NHs in Egypt; where it was observed that recurrent feelings of loneliness could be a cause for the presence of anxiety in older adults, along with other psychosocial and health factors (Barakat et al., 2019). Overall, the risk of developing loneliness in old age has been seen to increase with diagnoses of major depressive disorder, generalized anxiety disorder and social anxiety (Domènech-Abella et al., 2019; Lim et al., 2016; Power et al., 2018).
One of the physical health issues collected in our study sample was the presence of UI, which presented a statistically significant association with emotional loneliness. In an Irish macro study, higher odds of loneliness were found among older adults with UI, although the sample focused on community-dwelling older adults (Stickley et al., 2017). Currently, scientific evidence linking UI to loneliness is scarce, although much earlier studies already confirmed the increased risk of feeling lonely in middle-aged and older incontinent adults, with respect to continent people (Fultz & Regula Herzog, 2001; Yip et al., 2013). In contrast, the association of UI with anxiety disorders and depression is known which, in turn, may be reciprocally associated (Felde et al., 2017; Kwak et al., 2015) to loneliness in older adults and, therefore, it might be interesting to further investigate (Stickley et al., 2017).
However, recent studies have also suggested that the very act of becoming institutionalized and entering a NH has an impact on loneliness (Simard & Volicer, 2020). Entering to live in a long-term care facility can affect older adults due to the changes in their daily habits and customs, causing feelings of loneliness, as well as depressive and/or anxiety symptoms (Vasilopoulos, A. et al., 2020). For example, decreased frequency of contact with loved ones and friends and the discomfort of sharing a room with others may alter their intimacy and increase the perception of feeling lonely (Trybusińska & Saracen, 2019). Although it may appear that older adults residing in NHs exhibit less social isolation due to daily contact with staff and other residents (Theurer et al., 2015), the reality is that moving to a NH does not exempt them from continuing to need family and friendship support. But unfortunately, not all older adults can count on external social support, and this can have effects on their QoL and health (Barken et al., 2017; Chamberlain et al., 2018).
In terms of social loneliness, the results of our study could suggest that a poor social network and support may be a risk factor for people living in NHs. We observed that 61.3% were at risk of social isolation and a diminished social network (0 to 12 monthly family and/or friend visits). One systematic review proposed that social networks and social support are associated and may influence health during aging (Santini et al., 2015). More recently, one study showed how the size of the social network could influence the relationship between loneliness and depression (Domènech-Abella et al., 2017), where 60.6% of residents without children, or with only one child, presented with social loneliness. A study in twelve European countries revealed that in several countries, especially in the most traditionalist ones, childlessness was strongly associated with loneliness in old age (Zoutewelle-Terovan & Liefbroer, 2018). This is reinforced by another study in China which suggested family support is a protective factor for loneliness, both for people with and without children (Cheng et al., 2015).
Our study has some limitations. The relatively small size was due to the appearance of the Covid-19 pandemic and the successive waves, leading to very restrictive measures regarding social contact. This meant we could not continue collecting data and ceased in March 2020. Despite the small sample size, it was sufficient to detect statistical differences in the different variables considered significant in other scientific literature, as discussed above. Since loneliness is considered a subjective construct, we had to exclude 36% of the participants from the initial sample due to the presence of severe cognitive impairment, and 13% did not accept or could not answer the questionnaires for the evaluation of psychosocial variables. Dementia is more common in NHs in Catalonia, (70% of cases), compared with the population residing in the community (Amblàs-Novellas et al., 2020). If we had been able to examine loneliness in these excluded participants, the rates of loneliness could have been higher.
The cross-sectional nature of our research could be another limiting factor, as it does not allow us to draw conclusions about causal relationships between associated factors and loneliness. Furthermore, as this was a descriptive study, it was not possible to collect in-depth data and valuable information such as the opinion and experience of the residents themselves, which would require a qualitative methodological approach. Such an approach would provide quality knowledge to rethink intervention strategies for the reduction of loneliness rates in NHs.
Because of the high levels of depression and depressive symptomatology in our study, some findings could be influenced by cognitive distortions (Hitchcott et al., 2017). The sample consisted of a greater number of women than men, and this prevents generalizing conclusions about the existence of the difference between gender and the perception of loneliness among the older men living in NHs.
The strengths of this study were the assessment of loneliness, social and emotional, at the same time as QoL and other health and sociodemographic data within 5 NHs. More specifically, there is no evidence collected on the prevalence rates of loneliness among NH's residents before the Covid-19 pandemic, and before the confinements were imposed. Thus, the present research on loneliness in NH residents is interesting, especially at the present time, when NHs have been forced to impose restrictive measures on social contact and even social isolation in some of the waves of the pandemic and the need to address unwanted loneliness has become more visible for institutionalized older adults, and to health professionals working to improve their daily care. The wide diversity in the type of variables collected in the study (physical, psychological, social and health variables) contributes to the knowledge of the general health status of the group studied. Our study highlights the importance of person-centered care, considering the psychological and social dimension, which may be changed with the process of institutionalization in a NH. Finally, the information gathered in this study can contribute to the better planning of prevention and treatment and to improve the well-being and QoL of NH residents.
Regarding practical implications, this study has revealed that the quality of life of people living in NHs may be worsened by the perception of loneliness experienced by a high number of them. This suggests a comprehensive geriatric assessment in NHs that contemplates psychosocial aspects, such as associated depressive symptomatology and the social networks of institutionalized elderly people, reviewing daily practices related specially to visits from family and/or friends and outings, which contribute to diminishing the effect of perceived social isolation and loneliness.
At the scientific level, health professionals caring for institutionalized elderly people have the task of contemplating the social support networks and the family situation and structure, to detect aspects related to the risk of suffering from unwanted loneliness. To properly analyze perceived loneliness, it is important to disseminate disciplinary knowledge with the aim of improving attention and care, as well as research on the subject with the aim of redesigning intervention protocols aimed at detecting particularly fragile elderly people in the process of institutionalization and preventing the negative effects of unwanted loneliness and its consequences in the possible worsening of quality of life.
According to the results of the present study, interesting lines of intervention may consist of including intergenerational exchange practices with the aim of actively energizing NHs and fostering interpersonal relationships, especially in residents who do not have a family, to receive signs of affection and support. These experiences can also be a great source for promoting the integration of NHs into society. Another line of action would be to bring the institutionalized elderly closer to the community during their stay. Through recreational, cultural and social activities and popular festivities, we could promote the sense of competence, illusion, gratitude and the feeling of relevance of the group; in addition to bringing older adults closer to acquaintances and/or younger relatives, strengthening their emotional ties and increasing the constancy of visits, as well as improving relations between residents and staff working in the residences by enhancing the self-concept of the elderly, and consequently strengthen their self-esteem and improve the perception of loneliness, social isolation and increase the mood.
Conclusions
Loneliness can be a health risk factor and worsen the overall quality of life among older adults living in NHs. With the recent experiences of social isolation due to the Covid-19 pandemic, loneliness has been very present among institutionalized older adults. This study shows the high prevalence rate of loneliness (approximately 71%) in people over 65 years old living in 5 NHs in the Osona region (Barcelona, Spain), and the association of this phenomenon with a worse perception of health related QoL. Diagnosis of UI and depression were associated with emotional loneliness and a poor social network and having no or only one child associated with social loneliness. These findings suggest the importance of addressing the psychosocial needs of NH residents to prevent loneliness and improve their well-being and QoL. Furthermore, on the one hand, more studies on factors associated with social and emotional loneliness would be desirable to develop appropriate loneliness prevention strategies and improve the quality of life of NHs residents. And on the other hand, studies with larger and more representative samples, as well as longitudinal studies, would allow us to infer the causality of the associations between loneliness and associated psychosocial factors, in addition to physical and health conditions.