Introduction
The university stage is considered a highly stressful lifetime, associated with important changes in lifestyle, transitioning roles and the appearance of new responsibilities that can affect quality of life, decrease academic achievement and increase interpersonal difficulties (Auerbach et al., 2019; Ribeiro et al., 2018). These factors can enlarge the risk of psychological distress and mental disorders (Bayram & Bilgel, 2008), being mood and anxiety disorders, also called emotional disorders (EDs; Bullis et al., 2019), the most prevalent disorders among university students in Spain (Labrador et al., 2016; Miranda‐Mendizabal et al., 2019). In fact, evidence has shown that most of EDs usually appear between the ages of 15 and 24 (Auerbach et al., 2019).
Despite the high prevalence rates in university students of EDs, very few students receive mental health attention, as shown by the results of the study carried out by Auerbach et al. (2016), where they found that of the students who presented an EDs in the last 12 months, only 16.4% had received some type of intervention. Furthermore, the treatment usually starts after several years of the beginning of the symptomatology, making it harder to treat (Bienvenu & Ginsburg, 2007). In fact, EDs tend to become chronic, with low spontaneous remission rates between 17% and 30% (Craske & Zucker, 2002).
Knowing that the onset of EDs is usually in youth, and that its chronification makes treatment difficult, the development of brief preventive interventions in university contexts is especially important. In this line, research suggests that current prevention programs can reduce subclinical symptoms or vulnerability factors and decrease incidence of disorder onset (Brent et al., 2015, Stockings et al., 2016). However, these programs are generally aimed at children and adolescents, and have a prevention-oriented approach to specific disorders, as happens with specific treatment protocols for specific disorders (Bentley et al., 2018). The validity of these discrete conceptualizations is questioned by the presence of overlap disorders in clinical populations (Brown et al., 2001), which are closely related, with odds ratio (OR) of simultaneous prevalence between 3.9 and 21.3 for mood and anxiety disorders (Saha et al., 2021).
Thus, prevention strategies based on transdiagnostic approaches for psychological intervention could present several advantages. Current evidence has identified common underlying factors shared between the EDs, such as neuroticism, negative affectivity, perfectionism or rumination (Barlow et al., 2014; Bullis et al., 2019), so prevention strategies could focus on enhancing quality of life and emotional management, rather than emphasizing treatment of specific disorder symptoms (Sauer-Zavala et al., 2017b). In addition, some specific skills, such as problem solving or assertiveness training, have been shown to be useful for improving life satisfaction and well-being in students (De Sousa & da Costa Padovani, 2021; Gál et al., 2022) and could be incorporated in transdiagnostic preventive programs.
In this line, the Unified Protocol for Transdiagnostic Treatment of Emotional Disorders (UP) is a transdiagnostic cognitive-behavioural evidence-based psychological treatment (Barlow et al., 2018). Its goals focus on improving emotional regulation strategies through 8 different modules: setting goals and staying motivated, understanding your emotions, emotional awareness, cognitive flexibility, opposing emotional behaviours, coping with unpleasant physical sensations, emotional exposure and recognizing your achievements and looking to the future (Barlow et al., 2018).
Only four studies have developed prevention programs based on the UP in university students. Two of them were carried out by Barlow's team at Boston University, and both consisted of a single preventive session. In the first study, with a sample of 115 students (n = 45 in the experimental group), a face-to-face 2-hour workshop was carried out in group format. After the session, statistically significant improvements were found in neuroticism, quality of life, and experiential avoidance in the experimental group, compared to the control group (Bentley et al., 2018). The second study included 223 participants (n = 120 in the experimental group), which participated in a two-hour in-person transdiagnostic prevention workshop based on the UP. No significant differences were obtained in the emotional variables (stress, negative affectivity, and quality of life) compared to the waitlist control group (Sauer-Zavala et al., 2021). The third study, which had a sample of 128 students (n = 56 participants in the experimental condition), was carried out at the public University of Bogotá. A brief UP-based program (6 group sessions, one each week, lasting 2 hours). Significant decreases in neuroticism, stress, anxiety, depression and improvements in mindfulness, perceived anxiety control, and emotional dysregulation were found at the end of the program (Castro-Camacho et al., 2021). The fourth study consisted on the online and group application of the eight UP treatment modules to 9 students attended at the psychological attention service of the University of Cadiz, Spain. The intervention was applied weekly and had a total of 12 sessions. After the intervention, significant differences were found between pre and post scores on negative affect and perception of autolytic and aggression to others risk (Arrigoni et al., 2021).
Considering all the above mentioned and due to the high prevalence of EDs in university students, it would be essential to keep designing and developing programs focused on prevention of EDs in this population. For all these reasons, the objective of the present study is to determine the preliminary feasibility and effectiveness of a brief program based on the UP for the prevention of emotional symptomatology and EDs in the university population in Spain, focusing specifically on improving participants' emotional regulation skills and improving symptoms of anxiety and depression.
Method
Design
Due to the small number of participants, a multiple baseline design was used, since it has great advantages for preliminary studies or studies with a limited sample. The design uses the participants as its own control because it presents the same participants in all conditions and, to improve its internal validity, it makes multiple observations for the same participant (Sauer-Zavala et al., 2017a).
Participants
Nine university students (two men and seven women) aged between 19 and 27 years (M = 22.33; SD = 2.50) participated in this study. Regarding the level of the studies cursed by participants, five were students of college degree, one participant was a postgraduate student, and three participants were PhD students. Of the nine participants, 7 were single and 2 had a partner. Four of the participants worked while they were studying.
Initially, 14 people contacted to participate in the study and all of them carried out the pre-program evaluation. All of them met the inclusion criteria, but of the 14 initial participants, only nine answered the contact emails to start the baseline. The remaining five participants did not reply to the contact emails and did not provide information about their abandonment. The nine participants who completed the baseline started the program and all finished it.
Measures
Primary outcomes
Overall Anxiety Severity and Impairment Scale (OASIS;Norman et al., 2006,Osma et al., 2019). Instrument used to assess the frequency, intensity, severity and deterioration of anxiety-related symptoms. The OASIS is a five-item rating scale scored on a scale of 0 to 4, where higher scores indicate higher levels of severity and impairment. The internal consistency of the Spanish validation was 0.87.
Overall Depression Severity and Impairment Scale (ODSIS;Bentley et al., 2014,Osma et al., 2019). Instrument used to assess the frequency, intensity, severity and deterioration of depressive-related symptoms. As the OASIS scale, the ODSIS is a five-item rating scale scored on a scale of 0 to 4, where higher scores indicate higher levels of severity and impairment. The internal consistency of the Spanish validation was .94.
The Multidimensional Emotional Disorder Inventory (MEDI;Rosellini & Brown, 2019,Osma et al., 2021). Evaluation through 49 items of the transdiagnostic profile of EDs, which is made up of nine dimensions: neurotic temperament, positive temperament, depressed mood, somatic anxiety, autonomic arousal, social worries, intrusive cognitions, traumatic re-experiencing, and avoidance. The items have a Likert format with scales from 0 (it is not characteristic of me) to 8 (totally characteristic of me). The Cronbach’s alphas of the Spanish validation were between .74 and .92.
Difficulties in Emotion Regulation Scale (DERS;Gratz & Roemer, 2008;Hervás & Jódar, 2008). This measure evaluates difficulties in emotional regulation through 28 items, scored on a scale of 1 (Hardly ever) to 5 (Almost always), with five different subscales: lack of control, rejection, interference, inattention, and emotional confusion. A Cronbach’s alpha of .93 was found for the global scale in the Spanish validation.
Baseline evaluation questionnaire. To make easier the daily evaluation of the baseline, we summarized the variable we wanted to evaluate in one item. To do this, we chose the item with the highest factorial load for each variable (Suso-Ribera et al., 2018). Specifically, the participants answered two questions of The Emotion Regulation Questionnaire (ERQ; Gross & John, 2003; Spanish adaptation by Cabello et al., 2013) to evaluate cognitive reappraisal and expressive suppression. Both dimensions shown a good internal consistency for its adaptation into Spanish, with Cronbach’s α coefficients of .79 and .75, respectively.
Secondary outcomes
Brief Symptoms Inventory-18 (BSI-18;Derogatis, 2001;Andreu et al, 2008). Evaluation through 18 items ranged 0-4 (0 = none, 4 = Al lot) of psychopathology in 4 subscales: somatization, depression, anxiety and panic. The Spanish version has shown a good reliability, with a range of .71 for the anxiety factor to .88 depression factor, reaching the total BSI score a Cronbach’s alpha of .89.
The Multidimensional Scale of Perceived Social Support (EMASP;Zimet et al., 1988;Landeta & Zumalde, 2002). This measured evaluates perceived social support in relation to three dimensions of the social structure: family, friends and relevant people. Items follow a Likert format, with a scale ranged 1-7 (1 = totally disagree, 7 = totally agree). The EMASP has a good reliability, with Cronbach’s alpha ranged between .87 to .91 for the subscales, and .88 for the total scale.
EuroQol (Brooks, 1996;Badía et al., 1999). Assessment of self-perceived health status. First, it assesses self-perceived health status in severity levels (three levels: no problems, some problems or moderate problems, and unable or extreme problems) for each of the following five dimensions: mobility, self-care, daily activities, pain/discomfort, and anxiety /depression. Second, it assesses the self-perceived global health status today on a vertical visual analogy scale (VAS), ranging from 0 (worst imaginable health state) to 100 (best imaginable health state). Lastly, it includes an index of social values that is obtained for each state of health generated by the instrument, which ranges between a value of 1 (better state of health) and 0 (death). Both formats showed good test-retest reliability, with scores ranged .81- .92 on the intraclass correlation coefficient (ICC).
Treatment Satisfaction Questionnaire (STQ; an adaptation of Client Satisfaction Questionnaire (CSQ-8) ofLarsen et al., 1979). Our adaptation includes 6 of the 8 items of the CSQ-8 (perceived quality, adaptation to previous expectations, recommendation of treatment to friends or relatives, usefulness of the techniques learned, general satisfaction with the intervention, and probability that they will choose an intervention again of this type) and an item related to the discomfort generated by the intervention. Likewise, a change has been made in the Likert response scale, going from 4 points in the original (0 = “Bad / Nothing” to 4 = “Excellent/Very much”) to 11 in the current one (0 = “Bad / Nothing to 10 = "Excellent/Very").
Evaluation questionnaire of trained emotional regulation skills. Ad hoc questionnaire made up of 9 questions; one of a general nature that evaluates the usefulness of the program to improve emotional regulation and eight specific ones that separately evaluate the usefulness of each of the techniques that are worked on in the different modules to better regulate emotions. The response scale is Likert-type and ranges from 0 (not at all) to 10 (very much). It also includes five open-response questions to assess the opinion on the number and duration of the sessions, the contents and length of the manuals and the opinion of the application format used.
Procedure
Recruitment was done through the social networks (Instagram, Facebook, and twitter) of the University of Zaragoza and the research group of Research Health Institute of Aragon. Emails were also sent through the list-server of each degree and PhD programs of the University. Posters were also distributed throughout the different centers of the university. All ways of communication included the aim of the study “to learn how to regulate their own emotions” and a QR with a link to the Google Form of the study.
Once the participants entered the form, they found a more detailed description of the study and its objectives. To participate, they had to fill the informed consent and the General Data Protection Regulation (GDPR), sociodemographic data and the pre-program assessment. The Eligibility criteria were: (1) Be a student of the University of Zaragoza (Degree, Postgraduate studies or PhD); (2) Be at least 18 years old; (3) Good written and spoken understanding of Spanish; (4) Reside during the academic year in Aragon; (5) Have Internet access; (6) Not currently receiving psychological or pharmacological treatment for a mental disorder; (7) Signature of the informed consent.
Students who did not meet the inclusion criteria because they were currently receiving psychological or pharmacological treatment for a mental disorder were notified of the reason for exclusion from the study. Thus, they were informed about the preventive nature of the program, from which they could not benefit as the specialized treatment they were receiving was more recommended. If participants had clinical symptoms, they were referred to the public mental health system or to the official college of psychologists, so that they can find a specialist according to their needs.
After the initial evaluation, the students were randomly assigned to one of the three conditions: 1) start of the program after 5 days of evaluation; 2) after 8 days of evaluation; 3) or after 10 days of evaluation. Randomization was performed using randomization software (www.rando-mizer.org). Once participants were randomized to one of the three conditions, the researchers contacted them by email to organize the prevention program groups and to send the corresponding baseline evaluation forms (Google Form). The participants were divided into two groups based on the time preference of the participants. One of the groups had five participants and the other had four. Once the baseline assessment was completed, the groups started the program.
The intervention consisted on the online application of a preventive group program based on the UP (Barlow et al., 2018) during 5 sessions of 2 hours each. The program involves learning and training one UP skill per session. In some modules, other useful techniques were added, such as assertiveness training and problem solving. The skills worked on in each module were: 1) psychoeducation on emotions and functional analysis; 2) Emotional awareness; 3) Thought's flexibility and problem solving; 4) Countering emotional behaviours; 5) Emotional copying and assertiveness training. The participants received a brief manual summarizing the important contents of each session and also the exercises to be carried out, with their corresponding records for practice between sessions.
All treatment sessions were carried out by the same therapists. One group program was carried out by a UP Level I trained therapist, and the other group program was carried out by an expert therapist with an UP-Level II training.
During the program, participants also completed weekly baseline evaluations. Once the program was over, the patients filled out the post-program protocol. Likewise, follow-up was carried out after the end of the program at one month and at 3 months, following the same procedure as the post-program and with the management of email reminders.
Data analysis
Statistical analyses were performed with the SPSS 21.0 (SPSS 21.0; IBM, 2012). First, descriptive statistical analyses were carried out to analyse the sociodemographic data of the sample.
Second, to determine if there were statistical differences depending on the assigned baseline, nonparametric analyses were performed at the different moments of evaluation of the baseline and of the evaluation prior to program through the Kruskal-Wallis test. To calculate differences between responder and non-responder participants we used the Mann-Whitney U test.
Next, data analysis was performed using the full sample. Due to the number of participants, a non-parametric comparison of means was performed using the Wilcoxon signed-rank test to analyse the effectiveness of the program and determine if there were statistically differences between the different pre-post program and follow-up conditions. The correction of Cohen's r test (Cohen, 1988) was used to calculate the effect size, where values from .30- .50 are considered medium-moderate effect sizes.
Results
Differences in the evolution on the use of emotional regulation strategies between the three baseline conditions
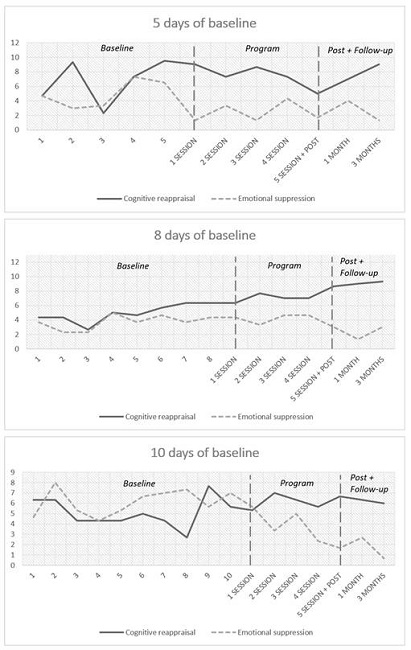
A visual analysis of the evolution of the emotion regulation strategies of cognitive reappraisal and emotional suppression throughout the different moments of evaluation in each of the baseline conditions was carried out. As can be seen on Figure 1, while the cognitive reassessment strategy tended to improve over time, emotional suppression decreased across assessments, regardless of whether participants were part of the 5, 8, or 10-day baseline condition.
Effectiveness of the program
Differences in scores between baseline conditions
Using the Kruskal-Wallis test, it was determined that there were no differences in the scores depending on the condition at any time during baseline data collection or in the pre-treatment evaluation for any of the variables (p < .05). Differences were only found on the somatic anxiety dimension of the MEDI (H(2) = 6.25, p =.04) at the pre-intervention assessment, showing the lowest scores in the group of 10 days baseline (means ranged 12.33-25.00). Differences by baseline group for the somatic anxiety dimension of the MEDI were not maintained on subsequent assessments. Because no other significant differences were found depending on the baseline condition, data analysis were performed using the full sample.
Pre-post treatment comparison
After the application of the program, significant differences (p < .05) were found in difficulties in emotion regulation (DERS) (W(8) = .00, p = .007, r = .59), perceived social support (EMASP) (W(8) = 5.00, p = .022, r = .49) and avoidance (MEDI’s dimension) (W(8) = .00, p = .007, r = .59), all three with moderate effect sizes. Although no more significant differences were found, we found medium effect sizes in other variables such as depressed mood (MEDI’s dimension) and depressive symptoms (ODSIS), neuroticism (MEDI’s dimension), intrusive cognitions (MEDI’s dimension) and somatic anxiety (MEDI’s dimension) (ranged .30- .37).
Table 1. Descriptive variables of the pre-program, post-program, 1 and 3-month follow-up conditions for the depressive and anxiety symptoms, difficulties in emotion regulation, general psychopathology, perceived social support, self-perceived health status and the nine dimensions of The Multidimensional Emotional Disorder Inventory (n = 9).
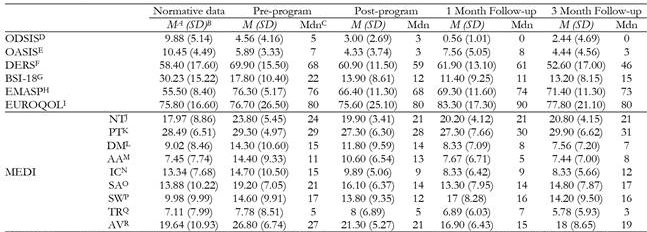
Note.MA = mean; SDB. = standard deviation; MdnC = median; ODSISD = Overall Anxiety Severity and Impairment Scale; OASISE = Overall Depression Severity and Impairment Scale; DERSF = Difficulties in Emotion Regulation Scale; BSI-18G = Global Severity Index of the Brief Symptoms Inventory-18; EMASPH = The Multidimensional Scale of Perceived Social Support; EUROQOLI = EuroQol’s thermometer; NTJ = neurotic temperament dimension; PTK = positive temperament dimension; DML = depressed mood dimension; AAM = autonomic arousal dimension; ICN = intrusive cognitions dimension; SAO = somatic anxiety dimension; SWP = social worries dimension; TRQ = traumatic re-experiencing dimension; AVR = avoidance dimension.
Table 2. Wilcoxon signed rank test for pre-post treatment comparison, pre-treatment and 1 Month Follow-up comparison, and pre-treatment and 3 Month Follow-up comparison of depressive and anxiety symptoms, difficulties in emotion regulation, general psychopathology, perceived social support, self-perceived health status and the nine dimensions of The Multidimensional Emotional Disorder Inventory (n = 9).
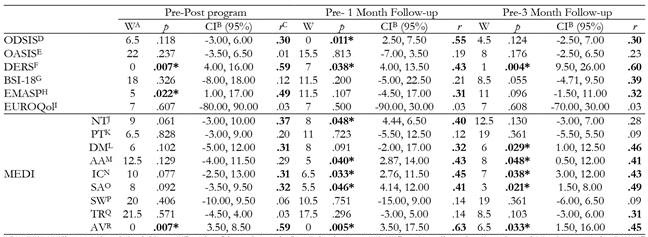
Note.WA = Wilcoxon Signed-Rank Test; CIB = Confidence interval; rC = Cohen's r test; ODSISD = Overall Anxiety Severity and Impairment Scale; OASISE = Overall Depression Severity and Impairment Scale; DERSF = Difficulties in Emotion Regulation Scale; BSI-18G = Global Severity Index of the Brief Symptoms Inventory-18; EMASPH = The Multidimensional Scale of Perceived Social Support; EUROQOLI = EuroQol’s thermometer; NTJ = neurotic temperament dimension; PTK = positive temperament dimension; DML = depressed mood dimension; AAM = autonomic arousal dimension; ICN = intru sive cognitions dimension; SAO = somatic anxiety dimension; SWP = social worries dimension; TRQ = traumatic re-experiencing dimension; AVR = avoid ance dimension;
*p < .05.
Pre-treatment and 1 month follow-up comparison
The significant differences found at the end of the treatment were maintained at one month of follow-up for difficulties in emotion regulation (W(8) = 7.00, p =.038, r = .43) and avoidance (W(8) = .00, p =.005, r = .63), also with moderate effect sizes. Other variables like depressive symptoms (W(8) = .00, p =.011, r = .55), neuroticism (W(8) = 8.00, p = .048, r = .40), intrusive cognitions (W(8) = 6.50, p =.033, r = .45) and somatic anxiety (W(8) = 5.50, p = .046, r = .41) had moderate-large effect sizes at the end of the program and presented significant differences at one month of follow-up, showing an improvement over time. The depressed mood variable kept moderate effect sizes (.32), and the perceived social support no longer present significant differences, but also kept moderate effect sizes over time (.31). In addition, the autonomic arousal (MEDI’s dimension) shown also an improvement on the month follow-up, presenting significant differences (W(8) = 5.00, p =.040, r = .43) with moderate effect size.
Pre-treatment and 3 months follow-up comparison
After three months, significant differences were maintained for the difficulties in emotion regulation (W(8) = 1.00, p = .004, r = .60), autonomic arousal (W(8) = 8.00, p = .048, r = .41), intrusive cognitions (W(8) = 7.00, p = .038, r = .43), somatic anxiety (W(8) = 3.00, p =.021, r = .49), and avoidance (W(8) = 6.50, p = .033, r = .45), all of them with moderate effect sizes. Depressive mood, which previously had shown considerable improvements, presented significant differences (W(8) = 6.00, p = .029, r = .46). Other variables, which had already shown improvement after the program or after one month's follow-up, continued to present moderate effect sizes, such as depressive symptoms and perceived social support (.30 - .32). In addition, new variables shown an improvement, such as general psychopathology (BSI-18) and traumatic re-experiencing (MEDI’s dimension), both with moderate affect sizes (ranged .31- .39).
Satisfaction with the program and application format and adherence
Satisfaction
As can be seen on Table 3, all participants shown a high satisfaction with the application format (online and group) (ranged 8-10), showing great acceptability and almost none discomfort caused. Regarding the contents of the program, all the modules were considered very useful for regulating emotions, with the first psychoeducation module being the best valued by the participants (ranged 5-10).
Table 3. Answers to our CSQ-8 adaptation and to the ad hoc questionnaire, including satisfaction with the program, contents and application format (n = 9).
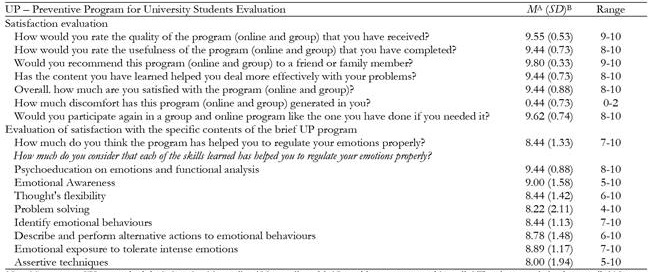
Note.MA = mean; SDB = standard deviation; 0 = No quality / Not at all useful / I would not recommend it at all / They have not helped me at all / Not sat isfied at all / Not at all uncomfortable / Not at all / Not at all; 10 = Maximum quality / Totally useful / I would highly recommend it / They have helped me a great deal / Totally satisfied / Maximum discomfort / Yes, without hesitation / Very much
Adherence
Of the 14 participants who carried out the pre-program evaluation, only 9 started the baseline forms and the preventive program. No differences were found (p > .05) between the pre-program scores in any instrument between the participants who dropped out and those who started the program, calculated by the Mann-Whitney U test. Despite the initial abandonment, all participants who started the program completed all the modules of the program along with all the evaluations established at the end of the program and in the corresponding follow-ups, counting the program with 100% adherence.
Discussion
In reference to the objectives of this study, we hypothesized that a brief program based on the UP for the prevention of emotional symptomatology would improve the emotional regulation strategies of the participants and improve symptoms of anxiety and depression. After the application of the program, results shown that it could be effective for the improvement of symptoms of anxiety and depression, as well as for the improvement of the emotion regulation strategies of the participants, which seem to be maintained and even getting better at three months follow-up assessment.
While variables such as perceived social support, avoidance and difficulties in emotional regulation already showed significant improvements after the preventive program, others, such as the dimensions of the MEDI, presented statistical differences during the follow-ups. This progressive improvement is also observable in Figure 1 for emotional suppression and cognitive reappraisal, evaluated in the baseline questionnaire, where an improvement in the expected direction of both strategies can be seen over time. This could be due to the fact that changes in some variables such as neuroticism, depressed mood or cognitive intrusions could require more practice and training in the skills learned during the program, therefore, the continuous practice of the skills could be the reason for the improvement during the follow-ups. Similar results were found by Sauer-Zavala et al. (2020), where the greatest changes in neuroticism occurred after 16 weeks.
This progressive improvement throughout the follow-ups could be related to the improvement of the emotional regulation strategies observed in the DERS scores, already observable after finishing the program, and in Figure 1 for cognitive reappraisal and emotional suppression. The application of preventive programs like this, capable of improving students' regulation strategies in a few sessions, could reduce the appearance of emotional problems and, consequently, reduce the personal and economic costs associated with EDs. The application of programs like this makes even more sense when vulnerability factors had achieved significant reductions after the application of the program, which also it’s maintained to a greater or lesser extent in the follow-ups, as is the case of avoidance and neuroticism.
Despite the methodology differences of the previous studies, these improvements in emotional regulation, avoidance, neuroticism, anxious symptomatology, and depressive mood are consistent with three of four previous studies on the implementation of UP-based preventive programs for EDs (Arrigoni et al., 2021; Bentley et al., 2018; Castro-Camacho, Díaz & Barbosa, 2021). To date, and considering the limitation of the sample of this pilot study, this is the shortest program that has obtained the best results. The exception is the intervention carried out in the pilot of Bentley et al. (2018), which consisted of a single two-hour session, and which obtained small effect sizes. When increasing the sample, no differences were found for a single session (Sauer-Zavala et al., 2021). In the case of the results obtain by Castro-Camacho, Díaz & Barbosa (2021), the effect sizes are similar but larger in our sample for the shared variables (DERS and neuroticism, positive affect and avoidance of the MEDI) except for neuroticism at 3-month follow-up, which is slightly lower in our study.
In terms of feasibility and acceptability, the patients showed a high predisposition and acceptance with the application format, which translated into 100% adherence to the program. All the participants positively valued the contents and quality of the program, as well as its usefulness to improve their emotional management. The training in problem solving and assertiveness, which is not generally included in other UP-based preventive programs for adults, were also positively valued by all participants. Regarding the open questions, all the participants thought that the duration of sessions and the contents explained in the manuals was adequate. Regarding the online format, the flexibility of the format was valued above all, being able to adapt the sessions more easily to their class schedules and internships at the university.
Despite the promising results, this study has some limitations to be considered. First, the small sample size. We decided to use a multiple baseline experimental design because this is the first study applying a brief online group UP based preventive program in a university context in Spain and because this methodology allow researchers to conduct pilot studies with small sample sizes maintaining some control standards (Sauer-Zavala et al., 2017a). Future studies must increase the sample size and use randomized control trials to test the long-term efficacy of this program. Second, a clinical interview was not conducted to detect whether any participant met criteria for any disorder. Instead, it was decided to ask participants about their past or current history of psychological or psychiatric treatment along with an assessment of general psychopathology using the BSI-18. The participants in our study had not received or were receiving treatment at the time of the program and showed non-clinical scores in general psychopathology. Third, as several participants commented, the number of instruments used was very large and could have been the reason for the initial abandonment. However, participants who completed the program were very satisfied with the format at the end of the program. The objective of the research team is to carry out a study where the sample is larger and where the changes or improvements produced by the prevention program can be better observed.
In summary, the results of this pilot study on the application of a brief transdiagnostic preventive program based on the UP have shown promising results, even achieving statistically significant improvements in this specific community population, university students. The transdiagnostic approach on group and online format allow greater flexibility and cost-efficiency than other intervention formats, making these brief prevention programs easier to be implemented in naturalistic community setting contexts such us primary prevention health services or in university psychological care services (Castro-Camacho et al., 2021; Ferreres-Galán, Quilez-Orden, & Osma, 2022; Martínez-Borba et al., 2022). However, it is necessary to continue investigating in this research line with a larger number of participants and long-term follow-up.