Introduction
Fatigue is a widely known phenomenon that is present in general and clinical populations. Its definition as a symptom refers to the subjective difficulty to initiate and complete voluntary physical or cognitive tasks (Li et al., 2020), and it manifests as an overwhelming feeling of tiredness, weakness or exhaustion, which does not disappear after resting Shahid et al., 2010; (Worm-Smeitink et al., 2017). Although there is no consensus on a universal definition of fatigue, research should be focused on its multidimensionality and continuum, which is experienced as a subjective and persistent internal feeling.
Numerous psychopathological manifestations present fatigue, such as sleep alterations, depression, anxiety and pain (Abrahams et al., 2018; Menting et al., 2018); in fact, it is a highlighted symptom in Major Depressive Disorder and Generalized Anxiety Disorder (McCallum et al., 2019). Fatigue understood as anergy, lack of energy or vitality, has been traditionally studied among the specific and general signs of initial schizophrenia (Häfner et al., 1992; Meehl, 1990). Specifically, fatigue is one of the main subdomains of negative symptoms established by the National Institute of Mental Health (Kirkpatrick et al., 2006). In another expression, if fatigue persists for six months or longer without an alternative explanation, it is diagnosed as chronic fatigue syndrome. Fatigue can be so severe that it may force the patient to significantly reduce his/her activities of daily living, and thus it is associated with poor quality of life and disability. Likewise, it manifests as one of the most common complaints among people infected with SARS-CoV-2, i.e., the virus that caused the recent COVID-19 pandemic. The prevalence of fatigue among the patients who recovered from COVID-19 ranges between 52 and 70 % (Carfì et al., 2020; Townsend et al., 2020).
In the face of this important public health problem, the adequate evaluation of fatigue in both clinical and non-clinical populations is especially relevant. Due to the lack of objective indicators of fatigue (Worm-Smeitink et al., 2017), its evaluation is based on self-reports. There are many instruments available to measure fatigue, such as the Fatigue Severity Scale, Multidimensional Assessment of Fatigue or Visual Analogue Scale, among others (Belza et al., 2018; Dittner et al., 2004; Whitehead, 2009). One of the most used self-reports is the Chalder Fatigue Scale (CFS) (Chalder et al., 1993).
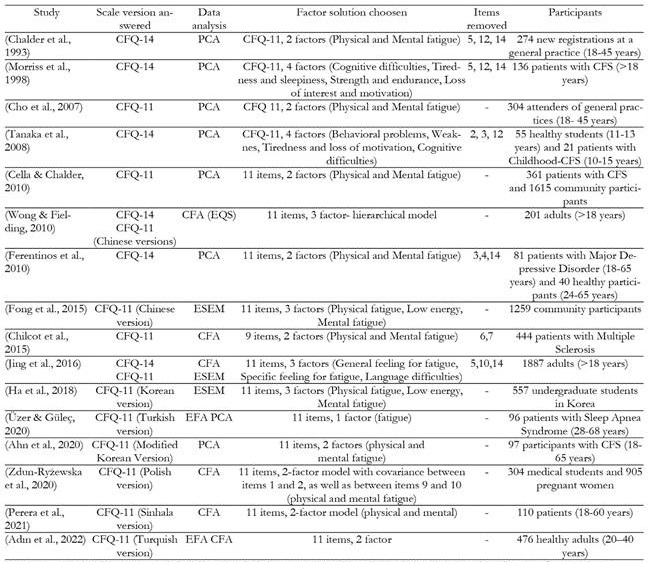
The original scale consists of 14 items, which measure the severity of fatigue in the last 3 months (Chalder et al., 1993). In the year 2010, the CFS was applied to a group of patients with chronic fatigue syndrome after removing three items (items 5, 12 and 14), obtaining a revised version with 11 items (Cella & Chalder, 2010) and two subscales: physical fatigue and mental fatigue. The scale has also been used in measuring fatigue in others clinical conditions such as multiple sclerosis (Chilcot et al., 2016) or major depression (Ferentinos et al., 2010). Its psychometric properties have been analyzed in different contexts (also non-clinical) and cultures, and it is currently validated in Brazil (Cho et al., 2007), Japan (Tanaka et al., 2008), England (Cella & Chalder, 2010), China (Fong et al., 2015), Turkey (Adın et al., 2022), Sri Lanka (Perera et al., 2021), Korea (Ahn et al., 2020) and Poland (Zdun-Ryżewska et al., 2020). However, different versions of the scale have been obtained each time (Chilcot et al., 2016; Ha et al., 2018; Tanaka et al., 2008; Wong & Fielding, 2010). See Appendix A for more details.
The CFS is used in Spain, although it has not been validated in the Spanish population. According to the sociological perspective of Marc Loriol, the meaning of fatigue is determined by each unique social environment (Loriol, 2017). It is worth highlighting that, in Spain, the word “fatigue” is polysemic. The Spanish dictionary of the Royal Academy (Real Academia Española, 2023) describes several definitions for fatigue, including: (1) Tiredness or weariness; (2) Discomfort caused by a more or less prolonged effort or by other causes, which sometimes generates physical alterations; (3) Urge to vomit; and (4) Suffering. In other words, the term fatigue encompasses different symptoms, thus using non-validated tools for the evaluation of the latter may lead to non-comparable results, which justifies the validation of the CFS in the Spanish population.
For the present study, we proposed the following objectives: a) to explore the factor structure of the Spanish version of the CFS (Sp-CFS); b) to find the invariance in measurement across sex and patient condition/control; c) to estimate reliability indicators (consistency and stability); d) to estimate signs of convergent validity with respect to negative emotional symptoms (anxiety, depression, and stress) and the negative and positive symptoms most closely related to psychosis; e) to compare the fatigue construct of the Sp-CFS in a general population and a clinical population through the scores obtained in the scale (differential validity).
Methods
Study design and sample
An observational, cross-sectional study was carried out to validate the Sp-CFS in a Spanish population. The initial sample was constituted by 3,680 participants (patients and general population), although the final sample consisted of 3671 participants after exclusion of 9 participants because they were over the age of 18, scored be-low five on the EPI (Eysenck & Eysenck, 1990) sincerity scale, or had not filled out the tests properly.
The age of the participants ranged between 18 and 86 years (M = 28.43; SD = 12.71), and 67.6% of them were women. Regarding marital status, 74.6% were single, 21.2% were married, 3.6% were divorced, and 0.6% were widowed. The sociodemographic characteristics of the sample and the clinical diagnoses of the patients are shown in Table 1. The general population was made up of the university and non-university population. The diagnoses were performed by clinical psychologists and psychiatrists with over twenty years of clinical experience, according to the DSM-5 classification (APA, 2013).
Table 1. Sociodemographic characteristics of the sample and clinical diagnoses.
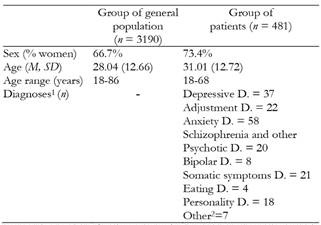
Notes: 1The number of patients shown in the table are those diagnosed in clinical interviews and used for the analyses considering the diagnosis. The rest of the patients were from two different studies and answered identify ing themselves as patients, but no breakdown by diagnosis is available for them.
2Other: Dissociative D. = 1; others applicable to Axis I = 3; Sexual D. = 1; ADHD = 1; Impulse control = 1.
Measures
The participants completed a questionnaire on previous and current psychopathology, psychotropic drug prescriptions, sex, age and marital status. They also answered the following questionnaires and scales:
Eysenck Personality Inventory (EPI), Sincerity Subscale (Eysenck & Eysenck, 1990). The EPI Sincerity Subscale comprises nine true/false items about daily life that identify dishonest answers. Participants who scored below five were excluded.
Chalder Fatigue Scale, CFS (Chalder et al., 1993). The translation by Hernández, et al. (2000) was used to validate the scale in a Spanish population. The CFS evaluates perceived fatigue as the set of subjective feelings of being tired, making a greater effort or finding it harder to start and keep up physical (physical fatigue/somatic) and mental (mental/cognitive fatigue) activities. The original scale consisted of 14 items, which were reduced to 11 in a later revision. Each item refers to the past 15 days before the test, and it is rated on a four-point Likert scale (1 = better than usual, 2 = no more than usual, 3 = worse than usual, 4 = much worse than usual). The internal consistency of the original scale obtained by Chalder was α = .89 for the total scale, α = .85 for the physical scale and α = .82 for the cognitive scale. The Spanish version of the scale may be seen in Appendix B in Supplementary Material.
Community Assessment of Psychic Experiences scale, CAPE (Stefanis et al., 2002; Spanish version by Fonseca-Pedrero et al., 2012) is a self-rated scale that assesses three basic dimensions of the psychosis spectrum: positive (20 items), negative (14 items) and depressive (8 items) to evaluate psychotic-like experiences and psychotic symptoms in the general population, and thus the potential risk of developing a psychotic disorder. It consists of 42 items with a four-choice Likert-type answer format. In this study, the internal consistency was α = .83 for the positive scale, α = .80 for the negative scale and α = .70 for the depression scale.
Hospital Anxiety and Depression Scale, HADS (Zigmond & Snaith, 1983). This scale consists of 14 items and evaluates anxiety and depressive symptoms in people with physical or mental illness and in the general population according to the symptoms during the past week. The total scale scores for anxiety (7 items) and depression (7 items) ranged from 0 to 21. In this study, the total internal consistency was α = .87, α = .80 for anxiety and α = .81 for depression, in the whole sample.
Referential Thinking Scale, REF (Lenzenweger et al., 1997; version by Rodríguez-Testal et al., 2019a). This scale evaluates the attribution of casual situations or events (looks, gestures, laughs) to oneself, thus it identifies cognitive processes related to the positive symptoms, specifically with reference ideas. It consists of 34 items with a true or false answer format. The total scale score was used in this study. The Cronbach’s α found for the total scale in this study was α = .95.
Depression Anxiety Stress, DASS-21 (Lovibond & Lovibond, 1995; Spanish version by Bados et al., 2005). This is a self-report measure of negative affect during one week, designed to measure the emotional states of depression, anxiety and stress. It consists of 21 items with a four-choice Likert-type answer format distributed across three subscales (with seven items each): depression, anxiety and stress. In this study, the internal consistency was α = .95 for the total scale, α = .92 for depression, α = .88 for anxiety, and α = .87 for stress.
Aberrant Salience Inventory, ASI (Cicero et al., 2010; version by Rodríguez-Testal et al., 2022) was used as a measure of proneness to psychosis, which evaluated the assignment of significance or importance to normally irrelevant internal and external stimuli. It consists of 29 items with a dichotomous (true or false) answer format. The total scale score was used in this study. For the sample of this study, the Cronbach’s alpha was .94.
Self-evaluation of Negative Symptoms, SNS (Dollfus et al., 2016; version by Rodríguez-Testal et al., 2019b). This scale consists of 20 items with three answer choices (0 = “strongly disagree”, 1= “somewhat agree”, 2 = “strongly agree”) that evaluates negative symptoms. It is comprised of five dimensions (avolition, alogia, anhedonia, asociality and diminished emotional range), although a total score can be used. The total scale score was used in this study. Internal consistency for this study had a Cronbach’s α = .90.
Procedure
To gather the data of the general population, we requested the students of the degree of psychology from two cities of Southern Spain (Andalusia) to complete the evaluation tests in the classroom during a voluntary activity, whereas the rest of the participants were recruited through the snowball sampling technique and completed the tests under supervision. The student's condition for participation was to get the participation of at least 4 more people who were not university students. The data of the clinical population were gathered by an accidental sampling of patients in different public hospitals and a private psychology clinic. The diagnoses were established by clinical psychiatrists and psychologists with over 30 years of clinical experience. To facilitate the subsequent statistical analysis, the primary diagnoses were grouped in types of diagnoses, following the DSM-5 (APA, 2013). All participants were informed about the objectives of the study, and they provided their written informed consent. The study complied with the precept of the Declaration of Helsinki and was approved by the Bioethics Committee of the Andalusian Government (code 2797-N-21).
Data analysis
We calculated the descriptive statistics of the items of the Sp-CFS. The normal distribution of the continuous variables was verified using visual (histogram) and analytical (Mardia’s test and Kolmogorov-Smirnov test) methods. Non-parametric tests (Spearman’s correlation coefficient) were used, since the variables did not present a normal distribution. The statistical significance level was set at p < .05 for all inferential analyses.
The construct validity was determined through exploratory factor analysis (EFA) and confirmatory factor analysis (CFA). The sample was randomly divided into two groups to carry out the cross-validation. First, exploratory factor analysis was conducted because the CFS was tested on a new population in which the factor structure of the scale had not yet been tested. With Sample 1, an EFA was conducted to analyze the internal structure of the scale using the ordinary least squares (OLS) method, given the ordinal character of the data, with promax oblique rotation and polychoric correlation matrix. The items with factor loadings < .40 were removed from the model, as suggested by Williams et al. (2010). Then, with Sample 2, several CFAs were performed: one CFA to verify the factor structure identified in the EFA, and another two CFAs to determine their suitability with the structure obtained in the original version (Chalder et al., 1993) and in the revised version of the scale (Cella & Chalder, 2010). All models were explored using CFA with robust diagonally weighted least squares (RDWLS), due to the nature of the ordinal data and the noncompliance with the assumption of multivariate normality. The goodness-of-fit indices of the CFA models were compared based on the following criteria: Goodness-of-Fit Index (GFI) ≥ 0.95, Tucker-Lewis Index (TLI) ≥ 0.95, standardized root mean square residual (SRMR) ≤ 0.08, root mean square error of approximation (RMSEA) ≤ 0.06, and confidence interval (CI) at 90% of RMSEA.
To analyze the invariance of the measure between sexes, the fit of the model was tested separately for men and women, and then a multigroup CFA was carried out. The same process was followed to determine the invariance between groups (clinical and non-clinical participants). The fit of the model was evaluated with ΔRMSEA and ΔCFI. Invariance was considered if Δ in CFI and RMSEA was < .01 (Chen, 2007).
The reliability of the scores in the SP-CFS was calculated though McDonald’s Omega, Cronbach’s Alpha, and Ordinal Alpha. The scale was administered to 411 participants after 30 days to find the retest reliability. Pearson’s correlations were used to calculate the time stability of both measures (test and re-test with 1-month interval) and the intraclass correlation index (> .50).
To determine signs of convergent validity, we analyzed the Spearman’s correlations of the total and subscale scores of the Sp-CFS with negative emotional symptoms (anxiety, depression and stress of the DASS-21, HADS and CAPE scales), positive symptoms (REF, ASI and CAPE scales) and negative symptoms (SNS and CAPE scales of the psychotic spectrum). The size of the correlations was interpreted using the method described by Cohen, in which the values of r ≥ .10, .30, and .50 are interpreted as small, medium and large, respectively (Cohen, 2013). Lastly, the differential validity evidence was evaluated by comparing the scores of the scale between patients and controls (Student’s t, ANOVA F). All statistical analyses were conducted using SPSS v21.0 and JASP v16.4.
Results
Sample characteristics and descriptive analysis
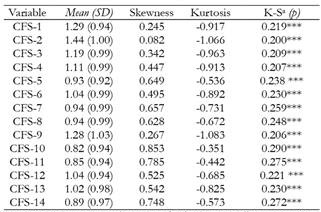
The total sample (N = 3671) was divided into two subsamples for cross-validation. The sociodemographic characteristics (sex and age) and general CFS measurements of both groups were equivalent (p > .05). Skewness was less than two points and kurtosis was less than three points for all items in the total sample. Mardia’s test showed a statistically significant result (skewness = 8.91; kurtosis = 275.03; p < .001). The Kolmogorov-Smirnov test indicated that the data did not follow a normal univariate distribution (p < .001). All the results are shown in Tables 2 and 3.
Table 2. Descriptive analysis of the two randomized groups.
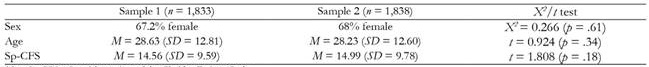
Note:Sp-CFS= Spanish version of the Chalder Fatigue Scale
Evidence of construct validity
Exploratory Factor Analysis (EFA)
An EFA was carried out with Sample 1 (n = 1833). The results of the Kaiser-Meyer-Olkin test were adequate (KMO = .93) and Bartlett’s sphericity test (χ²(91) = 20221.262, p < .001) was statistically significant, showing a good relationship between the items studied and, therefore, adequate for factor analysis.
The parallel analysis suggested a four-factor structure that explained 70.8% of the variance. Items 5-8 loaded on the first factor which was called low energy. The second factor was made up of items 1-3 and measured sleep problems. The third factor referred to concentration problems and was made up of items 4, 9 and 10. Items 11-13 loaded on the fourth factor that seemed to measure subjective cognitive dysfunction (brainfog) (Wolfe et al., 2021). Item 14 did not load in any factor, and its factor loading was < .40, thus it was removed from the model. The correlations between the factors ranged between .50 and .79. Table 4 shows the factor solution and factor loadings on each item.
Table 4. EFA structure matrix of the Sp-CFS scale.
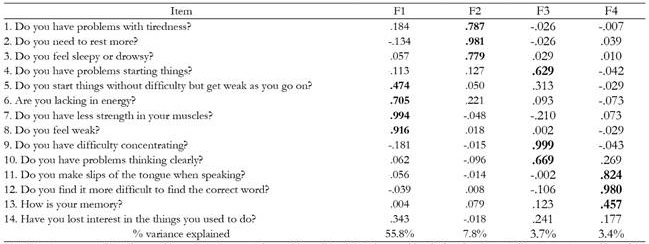
Note:F1 = Low energy; F2 = Sleep problems; F3 = Concentration problems; F4 = Subjective cognitive dysfunction; Item 14 did not saturate on either of the factors found in the model. (Uniqueness = .537). The factor loadings highlighted are significant > .40; The rotation method applied was promax.
Confirmatory Factor Analysis (CFA)
The obtained model (Model 1) was analysed through CFA along with the original version (Model 2, CFS-14, Chalder et al., 1993) and the revised version of the scale (Model 3, CFS-11, Cella & Chalder, 2010). All models were explored in Sample 2 (n = 1,838) using CFA with robust diagonally weighted least squares (RDWLS), due to the nature of the ordinal data and the noncompliance with the assumption of multivariate normality. Model 1 (4 factors) obtained better goodness-of-fit indices but was less parsimonious. (CFI ≥ 0.95; TLI ≥ 0.95; GFI ≥ 0.95; SRMR ≤ 0.08; RMSEA ≤ 0.06). Table 5 shows the goodness-of-fit indices of the models.
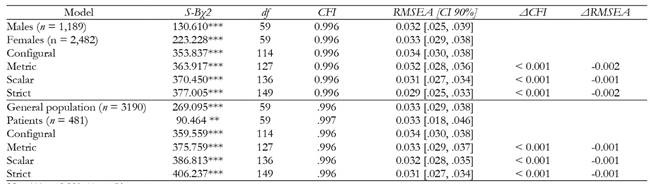
Invariance of measurement across sex and clinical condition
The invariance of the four-factor model (13 items) across sex and clinical condition was tested with multigroup CFA. As is shown in Table 6, the model was structurally invariant, as the ΔCFI and ΔRMSEA were under .01. Compliance of this invariance suggests that the intercepts of the regression that relate each item to its factor are the same among the analyzed samples (Chen, 2007). Therefore, these results provide evidence that the Sp-CFS is invariant across sex and clinical condition.
Evidence of reliability
Internal consistency for the Sp-CFS was assessed using McDonald’s Omega (ω = .923) and Cronbach’s Alpha (α = .922) scores for the total scale (13 items). Given the ordinal character of the data, Ordinal Alpha was also calculated for the total scale (α = .941) and the factors (α-F1 = .906; α-F2 = .910; α-F3 = .878; α-F4 = .807), showing that the items of the total scale and those of the factors have a high internal consistency.
Test reliability was evaluated using intraclass coefficients. Test-retest reliability (average 1-month interval) for the overall ICC was .93, 95% CI (0.92; 0.93) in the general population and ICC = .92 (0.91; 0.93) in the clinical population, ranging from .76 to .80 in the subgroups, thus showing excellent correlation.
Evidence of convergent validity
Criterion validity was calculated by correlating the Sp-CFS subscales with other scales measuring fatigue-related symptoms. Correlations from .30, .50 were considered moderate and those above .50 were considered high. The four factors were positively and moderately correlated with anxiety (r = .38-.47, p < .01), depression (r = .37-.49, p < .01), stress (r = .37-.47, p < .01), and the positive (r = .31-.41, p < .01) and negative symptoms (r = .30-.45, p < .01) of the psychosis spectrum. The results are shown in Table 7.
Table 7. Spearman’s correlations between the Sp-CFS and factors with the HADS (n = 474), DASS-21 (n = 2332), REF (n = 730); SNS (n = 1607), ASI (n = 2037); CAPE (n = 724).
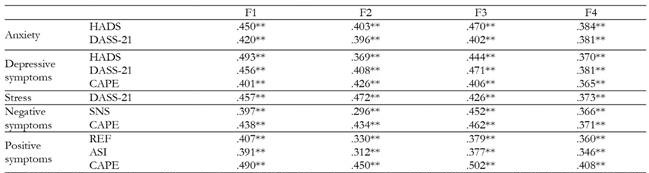
Note:HADS = Hospital Anxiety and Depression Scale, DASS-21 = Depression Anxiety Stress Scale, REF = Referential Thinking Scale, SNS = Self evaluation of Negative Symptoms, ASI = Aberrant Salience Inventory, CAPE = Community Assessment of Psychic Experiences Scale; F1 = Low energy; F2 = Sleep problems; F3 = Concentration problems; F4 = Subjective cognitive dysfunction;
**p < .01 (two-way).
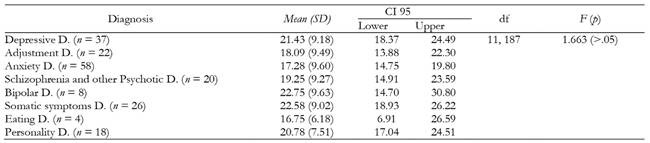
Analyses related to participant populations
The means obtained in the total score of the SP-CFS were compared between the two conditions of the participants (patients and general population). The results, t (3669) = 13.795, p < .001, show significant evidence with a medium effect size (d = .675) in the total scores of the SP-CFS between the general population (M = 13.10, SD = 8.76) and the patients (M = 19.08, SD = 9.46), with the latter obtaining significantly higher scores. Subsequently, an ANOVA was performed between the diagnoses grouped in categories over the Sp-CFS score. No statistically significant differences were found between the means of the groups according to the one-way ANOVA (F (11.187) = 1.663, p = .085), which indicates that homogeneity of variances was met between the groups (p > .05). The means of each group are shown in Table 8.
Discussion
The aim of this study was to validate and verify the psychometric properties of the Chalder Fatigue Scale in a Spanish population (Sp-CFS), with both healthy participants and patients. In the original scale (CFS-14) and its revised version (CFS-11), two factors were obtained (physical and mental fatigue) through a Principal Component Analysis (PCA) (Cella & Chalder, 2010; Chalder et al., 1993). However, although the two-factor model, which has also been obtained in other studies (Adın et al., 2022; Cho et al., 2007; Zdun-Ryżewska et al., 2020), fitted the data of the sample, the four-factor model extracted from the EFA obtained a better fit. Responding to the first objective, the results found in a Spanish population support a structure of 13 items and four factors: low energy; sleep problems; concentration problems; and subjective cognitive dysfunction, explaining 70.8% of the total variance. A satisfactory internal consistency and moderate-to-strong correlations were found among the factors of the Sp-CFS, thus showing evidence of convergent validity. The correlations between factors were significant, thereby supporting the use of geomin oblique rotation over orthogonal varimax rotation.
Previous studies have also obtained factor structures that differ from that of the original scale of Chalder. For instance, Morriss et al. (1998) and Tanaka et al. (2008) also found four factors of fatigue, although with structures different from those obtained in the present study. Nevertheless, other authors identified three-factor structures that differed among them (Fong et al., 2015; Jing et al., 2016; Wong & Fielding, 2010). Moreover, previous validations of the original scale (14 items) have generated different versions of the abbreviated scale (11 items), since they always discarded different sets of three items (Ferentinos et al., 2010; Tanaka et al., 2008). Other studies even obtained better results for a smaller scale (9 items) in people with Multiple Sclerosis (Chilcot et al., 2016). These differences may be due to the different analytical methods employed. In the present study, we followed the recommendations proposed from the theoretical framework of the Item Factor Analysis (IFA) (Ferrando et al., 2022). This reference framework advises against the use of PCA, since the conditions required for its application are rarely met (e.g., very high communality and a large number of items per factor).
In line with previous works, the present study supports the removal of item 14 (“Have you lost interest in the things you used to do?”), perhaps being more strongly associated with the construct of anhedonia (Cella & Chalder, 2010; Chalder et al., 1993; Ferentinos et al., 2010; Morriss et al., 1998). Furthermore, the characteristics of each study population and the cultural differences in the expression of fatigue may explain the discrepancies of structures of CFS obtained by the researchers. In contrast to the multiple meanings for the term "fatigue" in the Spanish language and culture (Real Academia Española, 2023), the main definition of "fatigue" as a symptom according to the Oxford English Dictionary (2023) is described as "Lassitude or weariness resulting from either bodily or mental exertion". Chalder's two-factor model adequately represents the English culture but is limiting for Spanish culture. However, although the data of the present study and those of the original scale are not methodologically in agreement, they are not so different at the conceptual level. Moreover, the four factors found after the EFA could be subscales of the two large factors found by Chalder: physical fatigue (low energy and sleep problems) and mental fatigue (concentration problems and subjective cognitive dysfunction). The present study highlights the dimensionality of the fatigue construct, showing that, at different levels, the measures of fatigue may indicate the potential presence of clinically relevant conditions.
The results of this study support the invariance of measure through the sex and clinical condition of the participant (second objective). This indicates that the mean scores in the factors of the Sp-CFS may be compared between men and women, as well as between patients and the general population without pathologies. Therefore, the latent dimensions underlying the instrument measure the same constructs and similarly between the mentioned populations.
Regarding the third objective, evidence of reliability was demonstrated for each of the factors extracted after the EFA. Adequate temporal stability and internal consistency were obtained, which implies that all items of the scale measure the same variable (in this case, fatigue). The evidence of convergent validity with respect to other measures emphasizes moderate and positive relationships with emotional symptoms (anxiety, depression, and stress for the factors of energy, sleep and concentration), and positive and negative symptoms of the psychosis spectrum (highlighting the concentration factor for the negative symptoms), thus complying with the fourth objective. This is in line with cross-sectional and longitudinal results obtained in previous studies (Doyle et al., 2010; ter Wolbeek et al., 2011), which found a clear association and covariance between fatigue and symptoms of depression or anxiety. Moreover, it was observed that depression and anxiety were risk factors for the development of fatigue itself. The relationship between fatigue and the negative and positive symptoms of the psychosis spectrum is not new. In fact, fatigue has been mentioned in specialized interviews on prodromal symptoms (Gross et al., 2012; Schultze-Lutter et al., 2007, 2012), and from the perspective of anomalous self-experience, such as diminished vitality (Parnas et al., 2005). Recent studies have found that the symptoms of chronic fatigue, along with the symptoms of anxiety, are the most important predictors of a poor health-related quality of life in schizophrenia (Kanchanatawan et al., 2018, 2019). It is worth mentioning the factor related to concentration, due to its relationship with the negative symptoms in this study, which must be further explored and specifies the importance of possible cognitive variables in these symptoms.
With regard to the last objective, the clinical population obtained significantly higher scores than the general population. However, the total scale did not adequately discriminate between the diagnoses established in clinical interviews, i.e., the differential validity of the test was limited. These results may be due to the high homogeneity observed in the group of patients, at least with respect to this transdiagnostic process. Future studies should validate the properties of the Sp-CFS in different and specific clinical populations with larger samples.
While one of the strengths of this study is the large sample size, one of its limitations in the generalization of the results is the sample selection, since a large proportion of the general population in this sample was constituted by university students. Nevertheless, fatigue is so normalized in the general population and in university students that it is eventually ignored, thereby generating consequences not only at the academic level (low performance and absenteeism), but also at the clinical level (Barone, 2017). It has been observed that students with comorbid fatigue and depressive symptoms suffer more from anxiety and functional deterioration, and are at greater risk of suicide (Nyer et al., 2015). Another limitation refers to the clinical sample (accidental sampling), as it represents a small sample size and a great variety of diagnoses. However, the result is interesting, as it demonstrates homogeneity in the clinical group with respect to the importance of fatigue. Future studies should include more specific diagnoses (e.g., chronic fatigue syndrome) and larger sample sizes. Another possible limitation is the development of the construct of fatigue in this instrument, as has been previously stated in different studies with CFS, which may suggest that fatigue must be specified according to the target population, with a more nuanced elaboration in order to demonstrate its usefulness.
In this study, the two-factor model also obtains an adequate and valid fit, however, we estimate that no statistical criteria have been crossed when stating that the model obtained by this study is superior at the level of goodness of fit indices as had been compared in Table 5. At the time we were faced with the decision of having to choose between the two-factor model (replicating the original structure and giving a more parsimonious description of fatigue) or taking a risk with the proposed structure. Choosing the bifactor structure was the most affordable with aseptic research criteria, but it was not familiar to us from clinical practice. We work with people with psychosis spectrum disorders and with people with emotional disorders. The fatigue expressed in psychosis is not the same as that expressed in a major depressive disorder, and yet, both would be framed within a generic mental fatigue, probably in a non-specific way. The dichotomous option physical fatigue vs. mental fatigue, consequently, was limiting when exploring what type of fatigue the person is experiencing. We consider that, conceptually, the multidimensional aspect of fatigue is better represented with our model without renouncing the bifactor division since, as we said previously, the factors raised can be understood as subfactors. We do not expect that the CFS will rule out the measurement of physical and mental fatigue in Spain; our intention is that its potential can be used to explore fatigue as a transdiagnostic indicator of other comorbid symptoms, and with the chosen structure, we consider that it enriched the result.
Conclusion
In conclusion, it can be asserted that the Chalder Fatigue Scale (Chalder et al., 1993) is a reliable and valid instrument to evaluate fatigue in the Spanish population, in both healthy and clinical populations. In addition to reflecting its multidimensionality through four well-differentiated factors, this scale confirms the transdiagnostic quality of fatigue. That is, it allows suggesting different clinical characteristics depending on whether the dominant symptoms are emotional (predominance of physical and cognitive manifestations of fatigue) or psychotic, either positive (majority of physical indicators of fatigue) or negative (mostly cognitive indicators of fatigue), which must be thoroughly analyzed in future studies.