Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
The European Journal of Psychiatry
versión impresa ISSN 0213-6163
Eur. J. Psychiat. vol.24 no.2 Zaragoza abr./jun. 2010
Insight in first episode psychosis. Conceptual and clinical considerations
Rafael Segarra Echebarría*,**,***; Natalia Ojeda del Pozo**,****; Arantzazu Zabala Rabadán**,***; Jon García Ormaza*; Javier Peña Lasa****; Iñaki Eguíluz Uruchurtu*,**,***; Miguel Gutiérrez Fraile**,***,*****
* Department of Psychiatry, Cruces Hospital, Osakidetza Mental Health System, Vizcaya
** Centro de Investigación Biomédica en Red de Salud Mental, CIBERSAM
*** Department of Neuroscience, Psychiatry Section, School of Medicine and Odontology, University of the Basque Country, Vizcaya
**** Department of Psychology, University of Deusto, Vizcaya
***** Department of Psychiatry, Santiago Apostol Hospital, Osakidetza Mental Health System, Alava. Spain
This study was supported by the Instituto de Salud Carlos III, Centro de Investigación Biomédica en Red de Salud Mental (CIBERSAM); by the Instituto de Salud Carlos III, FIS PI051508; by the Basque Government Department of Health (Healthcare Research Fund), 2008111010; and by the University of the Basque Country (UPV- EHU).
ABSTRACT
Background and Objectives: Poor insight or impaired awareness of illness is a very common feature in psychosis. The purpose of this study is to review critically the conceptual approximations from different perspectives to insight in psychosis and address its relations to other clinical and psychopathological variables.
Methods: We reviewed the principal factors that have been proposed to contribute to deficient insight in first episode psychosis patients from different conceptual frameworks, defence mechanisms or coping styles, structural or volumetric brain associations, cognitive deficits, and severity of clinical symptoms.
Results: This review of literature suggests that insight is a complex mental faculty heavily influenced by additional factors, such as social and cultural aspects, among others. Results also show the correlates of insight in first episode psychosis and treatment adherence in the course of the illness, although it is not stable over time. In fact, adequate level of insight is a necessary, but not sufficient condition for an adequate adherence.
Conclusions: Insight is a complex and multidimensional mental faculty that is a key factor in the prognosis of the illness. The link between both is probably mediated by the interaction of additional variables such as DUP, affective symptoms, sociodemographics, and drug abuse. Due to the complex relationships among insight, cognition and psychopathology in psychosis, these three factors could be considered as semi-independent phenomena. Finally, the neuroscience perspective about insight in psychosis is an especially productive research line that has contributed to a better understanding of the complex picture.
Key words: Insight; First episode psychosis; Review.
Insight: a complex and multidimensional concept
The delimitation of the concept
"Self" is a complex notion that brings together more than 25 centuries of reflections from different authors and areas of knowledge: philosophy, theology, sociology, psychology and psychopathology among others. The modern conceptualization of "insight" is built on the combined contributions of different areas of the neuroscience, that since the late-20th century have been derived from the study of that global notion of "Self". This more recent concept of insight has received an increased interest from clinicians, forensics and researchers. Insight is also referred into psychiatric literature as awareness of illness, adherence to treatment and denial.
Insight is defined as a phenomenon encompassing not only awareness of illness, but also awareness of illness consequences in the relation of the patient with the world1. It is widely recognized that when considering insight from a clinical approach, we are facing a complex mental faculty, that may be continuous (although there may be the possibility of a partial insight), multidimensional, and heavily influenced by social and cultural factors.
Among the primary dimensions of insight, the following are included1:
1. The awareness of having an illness, its signs and symptoms.
2. The awareness and attribution of recognizable symptoms to that illness.
3. The temporal projection of the insight, distinguishing between actual or retrospective insight, and assuming that insight may vary in extend across different stages of the psychotic process.
Additional factors related to insight
The presence of an adequate degree of insight has been associated with a better clinical and functional outcome in patients with psychosis2. Whereas low levels of insight are frequent (50-80%) among patients with schizophrenia3, studies on first episode psychosis (including schizophrenia spectrum disorders) have shown comparable higher levels of insight at baseline (60%) with significant improvements up to 80% at one-year follow-ups, with long term stabilization at 2-3 years follow-ups (78.6% and 82.8%, respectively)4. For bipolar disorder, deficits in insight are comparable to the schizophrenia described ones5.
Poor insight and coping styles. Post-psychotic depression and suicide risk
The psychodynamic approach to insight
The psychodynamic formulation of insight holds that poor insight represents an unconscious and adaptive defence mechanism that helps the patient to cope with the threatening and distressing diagnosis of psychosis and its consequences.
Melanie Klein maintained that denial and scission are basic and common defence mechanisms in psychosis, adding in a second term the mechanism of projective identification. Denial of the psychotic symptoms has been one of the most studied coping styles in psychosis related to poor insight, considering present and future time. Some authors have suggested that this mechanism may protect patients from depression, and that reduction of the intensity of denial over time may be a possible etiopathological factor for post-psychotic depression or "depressive realism"6.
Insight and prognosis in psychosis
Different studies have associated higher degrees of insight in first episode psychosis patients with a poorer initial prognosis. This poorer prognosis is explained by the elevated frequencies of post-psychotic depression among these patients with an adequate insight, and by the additional increased suicide risk in this group during the early course of the illness. For a more critical consideration of this association, the following results from literature should be noted:
1. A higher insight during the baseline assessment in a first episode psychosis patient is positively correlated with a higher prevalence of depressive symptoms at this time3.
2. A higher degree of insight predicts a higher risk for a subsequent post-psychotic depression, and a higher risk of suicide during the first four years after receiving the diagnosis of psychosis4.
3. Approximately 11% of the first episo-de psychosis patients, present self-harm episodes prior to their first diagnosis with an increased risk associated to male gender, low social class, depression, a longer DUP and increased insight7.
4. Finally, a recent systematic review has not found any definitive association between insight and violence, expressed as physical hetero-aggressive behaviours8.
Poor insight and neuroscience correlates
Brain volume findings and insight
The main clinical symptoms of the denominated "frontal lobe syndrome" are: perseveration, impulsivity, lack of inhibition, stereotypic behaviour, executive dysfunction, attentional deficits, lack of initiation, apathy, personality disturbances, "local-error monitoring" and lack of awareness on deficits. Research aimed to associate deficits of insight with brain abnormalities and deficits in specific cognitive domains, has been focused on the study of prefrontal cortex (dorsolateral, prefrontal and orbitofrontal regions).
Consistent findings show an association between poor insight in first episode psychosis patients (schizophrenia spectrum disorders) and decreased grey matter volumes in the dorsolateral prefrontal cortex, region that mediates cognitive processes such as executive functioning. Nonetheless, positive findings have been also referred to the right inferoparietal region, thalamus, supramarginal gyrus or the temporal lobes9. A recent study has concluded that patients with poor insight also present lower grey matter volumes in the temporal and parietal regions implicated in self-monitoring, working memory and access to internal mental states10.
Brain volume, insight, and cognitive deficits
The relevance of these findings is underlined when neuropsychological findings of insight are considered. Some recent studies have supported the hypothesis of memory deficits as underpinning lack of insight, since present experiences must be sustained by the previous ones11. According to this literature, patients with psychosis may be unable to maintain in the working memory current information on psychotic symptoms while comparing it with past experiences. This may interfere in the successful categorization of the current symptoms as aberrant, which might be manifested as an apparent lack of insight12.
Poor insight, cognitive domains and psychopathological dimensions
The neuropsychological approach to insight
The neuropsychological approach to the understanding of the deficits of insight is partially based on the experimental models proposed by Babinsky for the anosognosia and anosodiaphoria (1914), by Fredericks (1985) for the verbal anosognosia13, and more recently by Prigatano for the lack of awareness in the brain injury framework14.
Lewis, in a seminal report published in 193415 argues that defectual insight may be secondary to a specific brain injury affecting the normal integration of high cognitive processes. Based on this assumption, the neuropsychological hypothesis argues that poor insight arise form a cognitive deficit that has been experimentally validated from different theoretical models.
Relations between specific cognitive deficits and defective insight
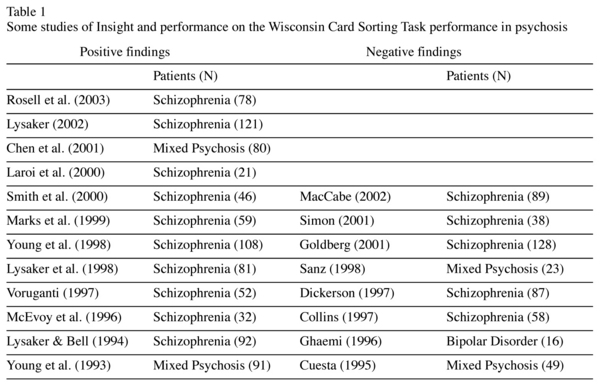
A review of the literature published on insight and cognition clearly reveals a focus of interest on the examination of prefrontal related cognitive tasks, through performance on the Wisconsin Card Sorting Test (WCST) (Table 1). A recent meta-analysis concludes that there is a significant relationship between perseverative errors on the WCST and poor insight, overcoming the relationship between IQ and insight16.
Additional evidences for the relationship between insight and cognition come from studies on people at an Ultra High Risk State for psychosis. Two different studies have revealed that this population presents greater insight and less impaired working memory performance than first episode patients6,17.
Insight, cognition, and psychopathology
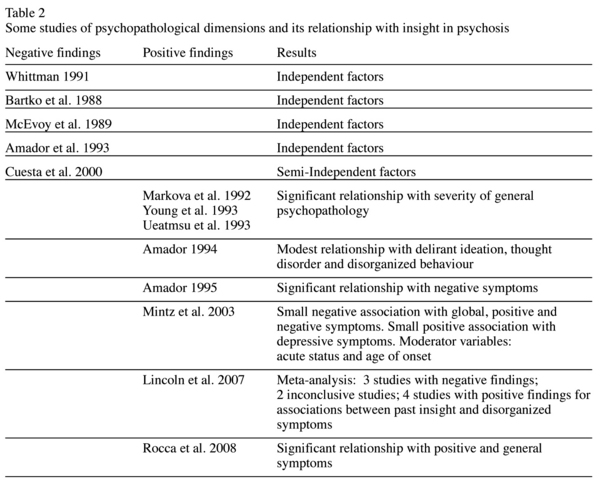
Poor insight has been also related with severity of psychotic symptoms (predominantly with the positive and disorganized dimensions, and to a lesser degree with the negative dimension), with later age of onset, and with a worse attitude toward medication (Table 2). On the contrary, higher and more stable degrees of insight have been related with less severe symptoms at long term follow-ups, and with lower rates of re-admissions2,6.
Furthermore direct associations are not always found and results are controversial11,18. Considering insight as a complex clinical symptom, influenced by other multiple variables (such as sociocultural factors, language or internal mental processes among others), some authors have proposed that the relationships between insight, neurocognition and psychopathology is too complex, and can not be reduced to simple associations. And therefore, these three factors could be considered as semi-independent phenomena in psychosis2.
The conceptual background behind this idea is that psychopathology or cognitive symptoms could represent concrete domains involving specific brain regions, which act as moderators of global brain functioning and higher mental processing. This framework may also request a continuous reformulation of psychopathology as a science, with an updated integration of novel findings and neurobiological techniques, and may be represented by an epistemological review of the field with contributions from philosophy and neuroscience19.
Getting into the specific interactions among variables
Findings depend on the measure used to assess insight
Several authors support that there are me-dium to high inter-correlations among several scales measuring insight (ITAQ, SAI, SUMD, item G12 PANSS, IS, item insight PSE e Insight Scale), suggesting that they seem to be assessing the same clinical target. However, this inter-correlation appears to be lower when past aspects of insight, or cognitive dimensions of insight, are being assessed8.
A study on first episode patients (schizophrenia spectrum disorders) concludes that the measure with a greater correlation with insight from the PANSS is item G9 ("unusual thoughts"), assuming that conceptual disorganization (rather than hallucinations and/or delusions) may lead to reasoning difficulties, and consequently to poorer insight (denial, misattributions)20.
Insight and treatment adherence
Special attention has been paid to the relationship between insight and treatment adherence in first episode psychosis. Adherence and compliance to treatment is a determinant prognostic factor for the clinical and functional outcome of psychotic patients21. Further considerations should include the following:
1. Among the main causes of treatment non-adherence some variables are patient-related (such as lack of insight), but other ones are external characteristic linked to socio-cultural context, therapeutical processes and treatment prescribed.
2. Lack of insight explains less than 30% of the variance for treatment non-adherence in first episode patients (schizophrenia spectrum disorders)22. Other variables such as psychotic symptoms, syndromic diagnosis, medication adverse effects and drug consumption, are also involved23.
3. The relationship between insight and treatment adherence is again complex, and not clearly supported24.
A recent meta-analysis concludes that the relationship between insight and treatment adherence is not stable over time. An adequate level of insight is a necessary, but not sufficient condition for an adequate adherence, and lack of insight does not necessarily leads to a poor adherence. Indeed, poor adherence could be addressed with specific therapeutic intervention (long-acting injectable antipsychotic medication, motivation-enhancing therapy, assertive community treatment). Once treatment compliance is ensured, the clinical and functional prognosis of first episode psychosis patients might be relatively independent of their level of insight24.
Discussion
Independently of the conceptual perspective, insight is a complex and multidimensional mental faculty influenced by other multiple variables. The relationships among insight, cognition and psychopathology in psychosis are complex and therefore cannot be reduced to simple associations.
From a clinical point of view, lack of insight is determined to be a key factor in the prognosis of the illness. As described, the link between both is probably mediated by the interaction of additional variables such as DUP, affective symptoms, sociodemographics, and drug abuse. The neuroscience perspective about insight in psychosis is an specially productive research line. Associations among insight, cognitive performance and possible neuroanatomic basis have contributed to a better understanding of the complex picture.
Despite of methodological limitations derived from the instrument employed to assess insight, findings have replicated a linkage between lack of insight and treatment adherence. Far from postulating a stable interaction, a critical review of literature leads to conclude that an adequate level of insight is a necessary, but not sufficient condition for an adequate treatment adherence. Furthermore, lack of insight does not necessarily leads to a poor adherence, and should be addressed as a specific therapeutic target with additional resources (long-acting injectable atypical antipsychotic medication, motivation-enhancing therapy, assertive community treatment). Once treatment compliance is ensured, the clinical and functional prognosis of first episode psychosis patients might be relatively independent of their level of insight.
References
1. Amador XF, Kronengold H. Understanding an assessing insight. In: Amador XF, David A, editors. Insight and Psychosis: awareness of illness in schizophrenia and related disorders, 2nd Ed. New York: Oxford University Press Inc.; 2004. p. 3-30. [ Links ]
2. Mintz AR, Dobson KS, Romney DM. Insight in schizophrenia: a meta-analysis. Schizophr Res 2003; 61: 75-88. [ Links ]
3. Crumlish N, Whitty P, Kamali M, Clarke M, Browne S, McTigue O, et al. Early insight predicts depression and attemped suicide after 4 years in first-episode schizophrenia and schizophreniform disorder. Acta Psychiatr Scand 2005; 112: 449-455. [ Links ]
4. Saeedi H, Addington J, Addington D. The association of insight with psychotic symptoms, depression, and cognition in early psychosis: a 3-year follow-up. Schizophr Res 2007; 89: 123-128. [ Links ]
5. Yen C-F, Cheng C-P, Huang C-F, Yen Y-K, Ko C-H, Chen C-S. Quality of life and its association with insight, adverse effects of medication and use of atypical antipsychotics in patients with bipolar disorder and schizophrenia in remission. Bipol Disord 2008; 10: 617-624. [ Links ]
6. Mutsatsa SH, Joyce EM, Hutton SB, Barnes TRE. Relationship between insight, cognitive function, social function and symptomatology in schizophrenia. Eur Arch Psychiatry Clin Neurosci 2006; 256: 356-363. [ Links ]
7. Harvey SK, Dean K, Morgan C, Walsh E, Demjaha A, Dazzan P, et al. Self-harm in first-episode psychosis. Br J Psychiatry 2008; 192: 178-184. [ Links ]
8. Lincoln TM, Lüllmanna E, Rief W. Correlates and long-term consequences of poor insight in patients with schizophrenia. A systematic review. Schizophr Bull 2007; 33(6): 1324-1342. [ Links ]
9. Nakamura M, Nestor PG, Levitt JJ, Cohen AS, Kawashima T, Shenton ME, et al. Orbitofrontal volume deficit in schizophrenia and thought disorder. Brain 2008; 131(1): 180-195. [ Links ]
10. Cooke MA, Fannon D, Kuipers E, Peters E, Williams SC, Kumari V. Neurological basis of poor insight in psychosis: a voxel-based MRI study. Schizophr Res 2008; 103: 40-51. [ Links ]
11. Lepage M, Buchy L, Bodnar M, Bertrand MC, Malla A. Cognitive insight and verbal memory in First Episode Psychosis. Eur Psychiatry 2008; 23: 368-374. [ Links ]
12. Flashman LA, McAllister TW, Johnson SC, Rick JH, Green RL, Saykin AJ. Specific Frontal Lobe Subregions Correlated With Unawareness of Illness in Schizophrenia: a preliminary study. J Neuropsychiatry Clin Neurosci 2001; 13: 255-257. [ Links ]
13. Laroi F, Barr WB, Keefe RSE. The neuropsychology of insight in psychiatric and neurological disorders. In: Amador XF, David A, editors. Insight and Psychosis: awareness of illness in schizophrenia and related disorders. 2nd Ed. New York: Oxford University Press Inc.; 2004. p. 119-156. [ Links ]
14. Prigatano GP. Disturbances of self-awareness and rehabilitation of patients with traumatic brain injury: a 20-year perspective. J Head Trauma Rehabil 2005; 20(1): 19-29. [ Links ]
15. Lewis A. The psychopathology of insight. J Med Psychol 1934; 14: 332-348. [ Links ]
16. Aleman A, Agrawal N, Morgan KD, David AS. Insight in psychosis and neuropsychological function. Br J Psychiatry 2006; 189: 204-212. [ Links ]
17. Lappin JM, Morgan KD, Valmaggia LR, Brooe MR, Woolley JB, Johns LC, et al. Insight in individuals with an At Risk Mental State. Schizophr Res 2007; 90: 238-244. [ Links ]
18. Cuesta MJ, Peralta V, Zarzuela A, Zandio M. Insight dimensions and cognitive function in psychosis: a longitudinal study. BMC Psychiatry 2006, 6:26. [ Links ]
19. Kircher T, David AS. Self-consciousness: an integrative approach from philosophy, psychopathology and the neurosciences. In: Kircher T, David A, editors. The self in neuroscience and psychiatry. Cambridge: Cambridge University Press; 2003. p. 445-473. [ Links ]
20. Keshavan MS, Rabinowitz J, DeSmedt G, Harvey PD, Schooler N. Correlates of insight in First Episode Psychoses. Schizophr Res 2004; 70: 187-194. [ Links ]
21. Robinson DG, Woerner MG, McMeniman M, Mendelowitz A, Bilder RM. Symptomatic and functional recovery from a first episode of schizophrenia or schizoaffective disorder. Am J Psychiatr 2004; 161: 473-479. [ Links ]
22. Novak-Grubic V, Tavcar R. Predictions of non-compliance in males with first-episode schizophrenia, schizophreniform and schizoaffective disorder. Eur Psychiatry 2002; 17: 148-54. [ Links ]
23. Sim K, Chang YH, Chua TH, Mahendran R, Chong SN, McGorry P. Physical comorbidity, insight, quality of life and global functioning in FEP schizophrenia: a 24-month, longitudinal, outcome study. Schizophr Res 2006, 88: 82-89. [ Links ]
24. Lincoln TM, Lüllmanna E, Rief W. Correlates and long-term consequences of poor insight in patients with schizophrenia. A systematic review. Schizophr Bull 2007; 33(6): 1324-1342. [ Links ]
![]() Correspondence:
Correspondence:
Rafael Segarra MD.
Department of Psychiatry, Cruces Hospital
Osakidetza Mental Health System
Plaza de Cruces s/n
48903 Vizcaya, Spain.
Tel.: (+34) 946006004
Fax: (+34) 946006294
E-mail: rafael.segarraechevarria@osakidetza.net
Received: 19 December 2008
Revised: 10 September 2009
Accepted: 15 September 2009