Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista Española de Enfermedades Digestivas
versión impresa ISSN 1130-0108
Rev. esp. enferm. dig. vol.108 no.4 Madrid abr. 2016
Health-related quality of life and determinant factors in celiac disease. A population-based analysis of adult patients in Spain
Julián Rodríguez-Almagro1, Antonio Hernández-Martínez2, Alfredo J. Lucendo3, Francesc Casellas4, María Carmen Solano-Ruiz5 and José Siles-González5
1 Emergency Department. Hospital General Universitario de Ciudad Real. Ciudad Real, Spain.
2 Nursing Midwife Teaching Unit. Hospital General La Mancha-Centro. Alcázar de San Juan, Ciudad Real. Spain.
3 Department of Gastroenterology. Hospital General de Tomelloso. Tomelloso, Ciudad Real. Spain.
4 Crohn-Colitis Care Unit. Hospital Universitari Vall d'Hebron - CIBERehd. Barcelona, Spain.
5 Nursing Department, School of Health Sciences. Universidad de Alicante. Alicante, Spain
ABSTRACT
Background: Celiac disease (CD) has a negative impact on the health-related quality of life (HRQL) of affected patients. Although HRQL and its determinants have been examined in Spanish CD patients specifically recruited in hospital settings, these aspects of CD have not been assessed among the general Spanish population.
Methods: An observational, cross-sectional study of a non-randomized, representative sample of adult celiac patients throughout all of Spain's Autonomous Regions. Subjects were recruited through celiac patient associations. A Spanish version of the self-administered Celiac Disease-Quality of Life (CD-QOL) questionnaire was used. Determinant factors of HRQL were assessed with the aid of multivariate analysis to control for confounding factors.
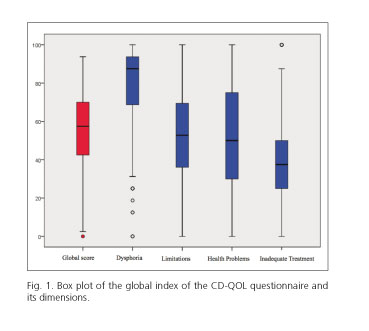
Results: We analyzed the responses provided by 1,230 patients, 1,092 (89.2%) of whom were women. The overall mean value for the CD-QOL index was 56.3 ± 18.27 points. The dimension that obtained the most points was dysphoria, with 81.3 ± 19.56 points, followed by limitations with 52.3 ± 23.43 points; health problems, with 51.6 ± 26.08 points, and inadequate treatment, with 36.1 ± 21.18 points. Patient age and sex, along with time to diagnosis, and length of time on a gluten-free diet were all independent determinant factors of certain dimensions of HRQL: women aged 31 to 40 expressed poorer HRQL while time to diagnosis and length of time on a gluten-free diet were determinant factors for better HRQL scores.
Conclusions: The HRQL level of adult Spanish celiac subjects is moderate, improving with the length of time patients remain on a gluten-free diet.
Key words: Celiac disease. Gluten-free diet. Quality of life. Population-based study. Spain.
Introduction
Celiac disease (CD) is a systemic autoimmune disorder, primarily digestive in nature, which is characterized by chronic inflammation of the small intestine and due to an immune response triggered and maintained by exposure to gluten in the diet (1). CD affects both children and adults with a genetic predisposition (2,3), but it seems to affect women more than men. The overall global prevalence of CD is estimated to be 1%, but it varies depending on age and country of origin of the study population (4-6). Moreover, the prevalence of the disease is increasing, with much higher incidence rates now than 20 years ago (7,8). Furthermore, many researchers acknowledge that the current prevalence of the disease may be underestimated due to underdiagnosis, especially in adults.
The prevalence of CD in Spain was calculated in a population-based study which was based on positive blood tests (9): this study found that the overall prevalence of CD across all age groups was 1:204 subjects, but it was more prevalent among children (1:71) than in adults (1:357). These numbers have shown no significant variations over the past decade (10). The median annual incidence of CD among Spanish children was recently estimated to be 7.9 cases per 1,000 live births and 54 cases per 100,000 people/year (11). However, the available population-based studies are limited to cases that resulted positive in blood tests, which represents only a small proportion of the total number of adult celiac patients. Researchers thus emphasize that Spain may actually have up to 450,000 celiac patients, with only 45,000 diagnosed to date (12).
Patient-reported outcomes (PROs) are increasingly important variables in the evaluation of the impact of chronic disease. To this end, the most commonly used PROs are the subjective constructs based on symptoms and patient perception of health-related quality of life (HRQL). The impact of PROs on the treatment of chronic disease, particularly those related to HRQL, constitutes a topic that has generated a high level of interest in the past few decades, with improvements to HRQL now comprising a specific treatment objective.
HRQL is a complex, multidimensional construct assessed with the aid of various instruments, usually in the form of questionnaires. The generic instruments originally used have given way to more specific types of questionnaires for different chronic conditions. In the case of CD, Drossman, et al. validated the specific CD-QOL questionnaire in 2010 in order to measure HRQL in celiac patients (13). This instrument was later adapted and validated for use in a Spanish context by Casellas, et al. in 2013 (14).
Several factors contribute to the negative impact that CD has on the HRQL of affected patients. The chronic nature of CD and the fact that treatment entails a demanding, permanent, restrictive diet (15,16) with periodic checkups are foremost among them, but other factors include the possibility of finding other affected family members (17), the limitations that a gluten-free diet imposes on family and social activities, and the psychological distress that all these factors generate. Indeed, celiac patients present an altered sense of well-being (18) due to the symptoms of the disease, the associated conditions, and a sense of fatigue (19), among other causes. Commencing and following a gluten-free diet has repeatedly been demonstrated to improve both the symptoms of the disease and HRQL, despite the restrictions this type of diet imposes (20,21). The degree of adherence to a gluten-free diet has been shown to be an essential factor in the HRQL of celiac patients, with better results in patients with total adherence (22).
The application of instruments to measure HRQL has allowed researchers to make comparisons between different stages in the evolution of disease, degrees of affectation, and temporal moments in the evolution of patients suffering chronic disease. Changes in HRQL are now considered as an integral part in the assessment of therapeutic interventions for chronic or prolonged pathologies (23,24). Merely having access to health care providers constitutes a factor that influences the perception of HRQL reported by patients. The majority of studies assessing HRQL in celiac patients have been developed within a clinical context and have included mostly patients who were recruited in a hospital setting. However, the high level of control of CD achieved through a strict and permanent gluten-free diet may lead patients to lose the perception that they are ill and thus attend fewer clinical follow-ups. Moreover, one review has noted that long-term follow-up guidelines for celiac patients vary widely in their recommendations, many of which are not evidence-based (25). For this reason, evaluations of HRQL as indicated in the available regulated studies, while accurately reflecting the perception of the level of well-being of the subjects to whom they are administered, may not adequately reflect the perception of HRQL among the general population of celiac patients, which includes subjects with various ranges of adherence to regular follow-up and various degrees of access to health care systems.
The goal of this study is to determine the health-related quality of life in a representative sample of Spanish adults with celiac disease along with its determinant factors.
Methods
Study design and area
A cross-sectional, descriptive, observational study of an intentionally non-probabilistic sample of Spanish adults with CD which was representative of the national adult celiac population (comprising patients between 16 and 75 years of age) was carried out between May and July 2015.
The criteria used to define CD were that the patient had been diagnosed by a medical specialist and was affiliated with a regional celiac association that was part of the Federation of Celiac Associations in Spain (FACE, in its Spanish abbreviation). The need to document the diagnosis and to pay association dues was considered to indicate a low risk of selection bias. All celiac patients who correctly filled out the self-administered questionnaire forming the basis of this study were included. Subjects under 16 or over 75 years of age were excluded from the study.
Study variables
We designed a data collection notebook that included an explanation of the aims and goals of our study and which guaranteed anonymity and confidentiality for all study subjects, along with other common ethical concerns. The questionnaire was given to the director of every celiac association in each of the 17 autonomous communities of Spain. The questionnaire was then forwarded to various celiac associations via social media networks, which published the questionnaire and requested members to fill it out voluntarily.
The anonymous questionnaire compiled demographic information such as age (in completed years) and sex of the study subject along with the time from symptoms onset to diagnosis of CD (in years), self-reported compliance with a gluten-free diet (yes/no), and time living with gluten in the diet (in years).
HRQL was assessed with the aid of a specific CD-QOL questionnaire, translated into Spanish and validated for use in a Spanish setting (14) with adult patients. The CD-QOL consists of 20 items examining four dimensions: dysphoria, limitations, health concern, and inadequate treatment. The questions are answered by the patient, who scores them on a Likert scale from 1 (total disagreement) to 5 (total agreement). The CD-QOL questionnaire produces an overall rating between 0 (worst quality of life) and 100 (best quality of life) points. Each of the four dimensions is expressed with the same scale of 0-100.
Calculation of the sample size
The number of patients necessary to form an adequate representation of the Spanish population was calculated taking into consideration the following: the total number of people between 16 and 75 years of age living in Spain in January 1, 2014 (n = 35, 0111,922) (26), an estimated prevalence of CD of 1%, a confidence level of 95%, and an absolute error of 0.6%. Thus, a minimum of 1,022 study subjects were needed to develop this study with statistical adequacy.
Statistical analysis
Absolute frequencies were used to express descriptive statistics whereas relative frequencies were used for qualitative variables. Average values (standard deviation) were used for quantitative variables if they presented a normal distribution. Otherwise, median values (interquartile range) were employed. For the bivariate analysis, Pearson's chi-square test was used when the independent and dependent variables were qualitative; if the responding variable was quantitative, the Student-Fisher t-test and Analysis of Variance (ANOVA) were used.
Finally, to control for any confounding bias, multivariate analyses were carried out with multiple linear regression, where the dependent variable was the rating for the overall quality of life index and that of the four dimensions that comprise it, while the independent variables were patient sex and age, time to diagnosis, and duration of treatment. The SPSS v. 20.0 program was used for all statistical analyses.
Ethical aspects
This observational study was developed based on anonymous data and was designed in accordance with the Declaration of Helsinki, as promoted by the World Medical Association (WMA).
Results
Participants
We included a total of 1,230 celiac patients who filled out the questionnaire correctly, including 1,092 ± 89.2% women and 138 ± 10.8% men, with an average age of 32.7 ± 10.0 years (range: 16 to 75 years). No significant differences were observed in the distribution of the sample by age, time to diagnosis of CD, and time to the start of dietary treatment (imposition of a gluten-free diet) between men and women. Table I summarizes the principal demographic characteristics of the sample population, globally and by sex.
HRQL levels in celiac patients
The average HRQL level in our sample, as assessed with the CD-QOL, was 56.3 ± 18.27. Levels were slightly higher for men than for women (58.0 vs 56.1, respectively; p = 0.276). No differences in the overall HRQL ratings were observed among the various age groups that comprised our sample (Table II).
HRQL levels varied significantly between the different dimensions making up the CD-QOL scale, with dysphoria being the dimension that obtained the highest mean score of 81.3 ± 19.56. This was followed by limitations caused by the illness, which had an average rating of 52.3 ± 23.43; health problems, with a score of 51.6 ± 26.08; and lastly, inadequate treatment, which had the lowest rating, namely 36.1 ± 21.18 points. The distribution of each dimension is represented in figure 1.
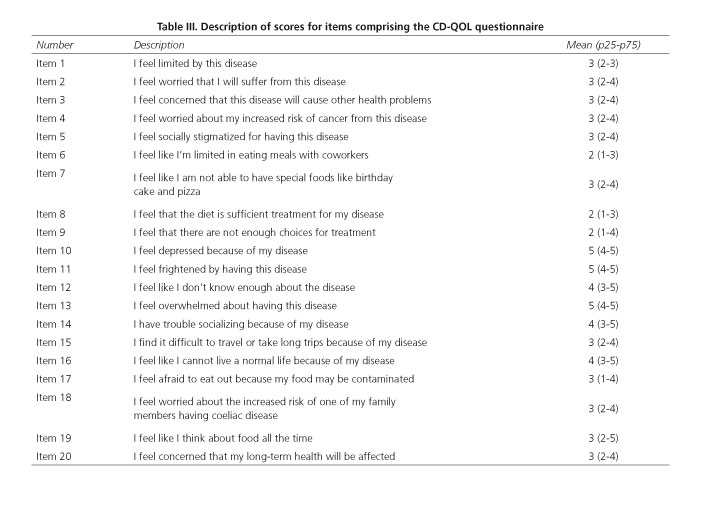
With regard to individual items, numbers 6, 8, and 9 (the latter two relating to the perception of having received inadequate treatment) obtained the lowest mean scores, as shown in table III.
HRQL determinants in celiac patients
Patient age and sex, along with time to diagnosis and the length of time following a gluten-free diet, were found to be the independent factors that determined the HRQL of adult patients with CD, as assessed with both univariate and multivariate analyses. However, each of these factors had a differential influence on the various dimensions included in the CD-QOL questionnaire (Table IV).
Women rated the dimension health problems lower than men (50.8 vs. 57.9, respectively; p = 0.03), while they gave the dimension of inadequate treatment a higher score than men did (36.7 vs. 30.9; p = 0.003) (Table II); this latter association was likewise documented in the multivariate analysis (Table IV). For the remaining dimensions, no gender differences were observed.
Age was associated with a lower score in the health problems dimension, which was rated significantly lower by patients between 31 and 40 years of age, as determined through univariate analysis (Table II). The multivariate analysis revealed an association between an advanced patient age and a lower rating for this dimension (Table IV).
The amount of time it took until an accurate diagnosis of CD was made significantly affected the ratings of all dimensions of the CD-QOL index (Table II); however, the multivariate analysis only showed a significant association for the inadequate treatment dimension, in the sense that the greater the amount of time to diagnosis, the worse the subjects rated this dimension (Table IV).
Lastly, a significant association was observed between the length of time patients had followed a gluten-free diet and the mean rating for HRQL on the CD-QOL scale overall and in each of its four dimensions (Table II). This significant association was maintained after the multivariate analysis, both for the overall index as well as in three of the four dimensions (Table IV). A longer period on a gluten-free diet was associated with a higher overall rating on the CD-QOL scale and in the dysphoria and limitations dimensions. The inadequate treatment dimension showed a significant inverse relation.
Discussion
This study evaluates the HRQL of a representative sample of Spanish adults with CD, both globally and among its various dimensions, in order to determine the factors that are determinant or associated with it. What differentiates this study from previous research is that it is the first study conducted using a CD-QOL questionnaire (14) that had been linguistically and culturally adapted and validated for use in a Spanish context, specifically for adults with CD. The main result of this study is that our series of adult Spanish celiac subjects, representative of the general celiac population, expressed a mean HRQL of 56.3 (out of a maximum of 100 points), notably lower than the ratings observed in the scant number of prior studies which used the same instrument (the CD-QOL questionnaire) in a Spanish setting. Thus, the quality of life levels reported by patients recruited in Spanish hospitals ranged from 80 points for patients who strictly followed a gluten-free diet to 70 points for patients who did not follow a gluten-free diet (either unknowingly or intentionally) (22), while newly diagnosed cases and patients who had followed a gluten-free diet for longer than a year showed overall mean HRQL ratings of 72-73 points (14). Studies based on the same instrument but used in other sociocultural contexts are rare, mostly because the original CD-QOL questionnaire was only validated in 2010. One study conducted on celiac patients in an area of New York (USA) which used the CD-QOL questionnaire found quality of life levels higher than those documented in our study (27), but other studies based on more generic instruments (e. g., the EuroQOL) (28) found lower HRQL levels in celiac patients than those observed in the New York series (29,30). Our results suggest that the HRQL found in the general population of adult celiac subjects may be lower than that observed in patients recruited in a hospital setting, giving rise to the hypothesis that periodic medical check-ups improve the quality in life for these patients by encouraging a stricter compliance with a gluten-free diet. In fact, the correct maintenance of a gluten-free diet has repeatedly been shown to be an independent factor associated with a better quality of life among celiac patients, both in children (31) and adults (19,20,22,32,33). Our study did not examine the adherence to medical follow-up among the study subjects; therefore, further studies must be made to provide solid data to support this hypothesis.
In our study, patient gender was shown to be an independent factor associated with the perception of HRQL in CD, one that has a significant effect on both the health problems and inadequate treatment dimensions of the CD-QOL questionnaire, with women giving an average rating 6.69 points lower than men in the former dimension and 5.64 points higher in the latter. One speculative explanation for this may be the greater difficulty perceived by the Spanish men in our series in finding substitutions or alternatives for foods when following a gluten-free diet in comparison to women, or the greater value placed on the act of eating on the part of men. In the Spanish context, women generally bear greater responsibility for buying and preparing food, perhaps conditioning a greater dependence on the part of men in this respect. We feel that the ratio of men to women in our series (1:9) does not affect this result, as it was controlled for by univariate and multivariate analyses. At any rate, it should be noted that the disproportionate numbers of men and women in our sample do not in any way reflect the distribution of men and women in the adult celiac population in Spain, but rather a different rate of response to a voluntary questionnaire among the sexes. In fact, all the epidemiological studies carried out to date have repeatedly documented the overall predominance of CD among women, with a female:male ratio varying from 2.5:1 to 3:1 (34). In cases of adult onset CD, the frequency among women may be even greater; prior studies of CD in Spain with somewhat different data have estimated the proportional frequency to be between 3:1 and 4:1 (35,36) and up to 9:1 among adult patients newly diagnosed with CD (37).
The lowest scores on the CD-QOL questionnaire were for items directly related to diet, namely items 6, 8, and 9. The first of these, item 6 ("It affects me that I'm limited as to what I can eat with my friends"), refers directly to the negative social repercussions arising from a gluten-free diet whereas the other two items with low scores denote concepts which appear to contradict each other, namely item 8 ("I feel that dietary treatment is sufficient for my illness") and item 9 ("I feel like there are not enough treatment options available"). While dietary treatment is considered to be a sufficient therapeutic intervention for curing CD, patients simultaneously recognize that it is difficult to comply with a strict, gluten-free diet and they would like to have more treatment options, perhaps including a broader variety of dietetic options directed at greater standardization towards a non-restricted diet.
The celiac patients in our series also expressed anxiety about the possibility of developing cancer (item 4: "I am worried about having a higher risk of cancer due to my illness"), with an average score of 3 out of 5 points, in direct contrast with the fact that CD is not specifically associated with a higher risk of cancer (38). Indeed, the type of tumor for which CD patients present an increased risk, intestinal lymphoma (39), is not only quite rare, but also becomes less likely in patients following a gluten-free diet to the point that they present no higher risk for this type of cancer than the general population. In contrast, CD actually represents a protective factor against several other types of neoplasms, such as breast and endometrial tumors (39). The perceived risk of certain comorbidities commonly associated with CD, such as osteoporosis and its clinical manifestation as bone fractures (40,41), was not observed in our sample.
Of the four dimensions that make up the CD-QOL, dysphoria received the highest scores in our series of CD patients, followed by health problems. Inadequate treatment was the dimension which received the lowest mean score. This is in agreement with previous studies conducted with Spanish celiac subjects (14,22). One new finding from our study is that HRQL (expressed as the overall CD-QOL index as well as in two of its dimensions, dysphoria and limitations) increased in accordance with the length of time that patients followed a gluten-free diet. Only the dimension inadequate treatment showed an inverse relationship between duration of treatment and HRQL. This result is in agreement with that found in a previous Spanish study conducted by Casellas, et al. (22), the results of which complement our findings, namely that in addition to the degree of compliance (patients who strictly complied with a gluten-free diet expressed a better quality of life than those that did not fully comply, either knowingly or inadvertently), the longer celiac patients followed a gluten-free diet, the higher they rated their quality of life.
The strength of our study comes from its ample sample size (1,230 subjects), the representative nature of the sample with regard to celiac population in Spain as a whole, and the controlling for possible confounders by means of multivariate analysis. Together, these aspects make our study an accurate assessment of HRQL of adult celiac patients in Spain.
However, our study has several limitations due to the absence of a non-randomized sampling protocol. The way in which we collected the data, due to the study design and the process of working through celiac patient associations, hindered us from knowing the exact response rates and profiles of the patients, who may have received the questionnaire and chosen not to respond. The high proportion of females who responded to the survey also may affect the representativeness of our research. The attitudes of patients who responded voluntarily to treatment may be more favorable than those of patients who did not respond; thus, participation in this study could reflect either a greater involvement on the part of the patient in controlling his or her illness (most likely with a stricter compliance with a gluten-free diet), or, in contrast, the involvement of the most affected patients.
In conclusion, our study explores for the first time the levels of HRQL in a broad sample of Spanish adults with celiac disease, recruited from the general population throughout Spain and thus potentially representative of the general celiac population on a national level. Overall, the perceived HRQL levels were within an average range, influenced by patient sex and age along with the time to diagnosis and the duration of treatment with a gluten-free diet. It is important to note that HRQL increased significantly as the longer the patients followed a gluten-free diet. Future research should focus on additional determinant factors for the lower overall HRQL of celiac patients recruited from the general population with regard to their counterparts recruited in a hospital setting.
Acknowledgements
This study would not have been possible without the collaboration of the associations and groups of celiac patients throughout Spain, through which we were able to reach the greatest number of CD patients.
References
1. Schuppan D, Junker Y, Barisani D. Celiac disease: From pathogenesis to novel therapies. Gastroenterology 2009;137:1912-33. DOI: 10.1053/j.gastro.2009.09.008. [ Links ]
2. Sapone A, Bai JC, Ciacci C, et al. Spectrum of gluten-related disorders: Consensus on new nomenclature and classification. BMC Med 2012; 10:13. DOI: 10.1186/1741-7015-10-13. [ Links ]
3. Ludvigsson JF, Leffler DA, Bai JC, et al. The Oslo definitions for coeliac disease and related terms. Gut 2013;62:43-52. DOI: 10.1136/gutjnl-2011-301346. [ Links ]
4. Mustalahti K, Catassi C, Reunanen A, et al. The prevalence of celiac disease in Europe: Results of a centralized, international mass screening project. Ann Med 2010;42:587-95. DOI: 10.3109/07853890.2010.505931. [ Links ]
5. Enfermedad Celiaca (online). World Gastroenterology Organisation; 2012. Cited 2015 May 1st. Available from: http://www.worldgastroenterology.org/UserFiles/file/guidelines/celiac-disease-spanish-2013.pdf. [ Links ]
6. Rewers M. Epidemiology of celiac disease: What are the prevalence, incidence, and progression of celiac disease? Gastroenterology 2005;128(4 Suppl. 1):S47-51. DOI: 10.1053/j.gastro.2005.02.030. [ Links ]
7. Catassi C, Kryszak D, Bhatti B, et al. Natural history of celiac disease autoimmunity in a USA cohort followed since 1974. Ann Med 2010;42:530-8. DOI: 10.3109/07853890.2010.514285. [ Links ]
8. Lohi S, Mustalahti K, Kaukinen K, et al. Increasing prevalence of coeliac disease over time. Aliment Pharmacol Ther 2007;26:1217-25. DOI: 10.1111/j.1365-2036.2007.03502.x. [ Links ]
9. Marine M, Farre C, Alsina M, et al. The prevalence of coeliac disease is significantly higher in children compared with adults. Aliment Pharmacol Ther 2011;33:477-86. DOI: 10.1111/j.1365-2036.2010.04543.x. [ Links ]
10. Riestra S, Fernández E, Rodrigo L, et al. Prevalence of coeliac disease in the general population of northern Spain. Strategies of serologic screening. Scand J Gastroenterol 2000;35:398-402. DOI: 10.1080/003655200750023967. [ Links ]
11. Cilleruelo ML, Roman-Riechmann E, Sánchez-Valverde F, et al. Spanish national registry of celiac disease: Incidence and clinical presentation. J Pediatr Gastroenterol Nutr 2014;59:522-6. DOI: 10.1097/MPG.0000000000000446. [ Links ]
12. Rodrigo Sáez L. Celiac disease in the adult. Rev Esp Enferm Dig 2006;98:397-407. DOI: 10.4321/S1130-01082006000600001. [ Links ]
13. Dorn SD, Hernández L, Minaya MT, et al. The development and validation of a new coeliac disease quality of life survey (CD-QOL). Aliment Pharmacol Ther 2010;31:666-75. DOI: 10.1111/j.1365-2036. 2009.04220.x. [ Links ]
14. Casellas F, Rodrigo L, Molina-Infante J, et al. Transcultural adaptation and validation of the Celiac Disease Quality of Life (CD-QOL) Survey, a specific questionnaire to measure quality of life in patients with celiac disease. Rev Esp Enferm Dig 2013;105:585-93. DOI: 10.4321/S1130-01082013001000003. [ Links ]
15. Cranney A, Zarkadas M, Graham ID, et al. The Canadian Celiac Health Survey. Dig Dis Sci 2007;52:1087-95. DOI: 10.1007/s10620-006-9258-2. [ Links ]
16. Black JL, Orfila C. Impact of coeliac disease on dietary habits and quality of life. J Hum Nutr Diet 2011;24:582-7. DOI: 10.1111/j.1365-277X.2011.01170.x. [ Links ]
17. Santolaria S, Montoro M. Enfermedad celiaca, dieta sin gluten y calidad de vida relacionada con la salud. Rev Esp Enferm Dig 2015;107: 193-5. [ Links ]
18. Casellas F, López Vivancos J, Malagelada JR. Percepción del estado de salud en la enfermedad celiaca. Rev Esp Enferm Dig 2005;97:794-804. [ Links ]
19. Casellas Jorda FC, López Vivancos J. Fatigue as a determinant of health in patients with celiac disease. J Clin Gastroenterol 2010;44:423-7. [ Links ]
20. Johnston SD, Rodgers C, Watson RG. Quality of life in screen-detected and typical coeliac disease and the effect of excluding dietary gluten. Eur J Gastroenterol Hepatol 2004;16:1281-6. DOI: 10.1097/00042737-200412000-00008. [ Links ]
21. Dorn SD, Hernández L, Minaya MT, et al. The development and validation of a new coeliac disease quality of life survey (CD-QOL). Aliment Pharmacol Ther 2010;31:666-75. DOI: 10.1111/j.1365-2036.2009.04220.x. [ Links ]
22. Casellas F, Rodrigo L, Lucendo AJ, et al. Benefit on health-related quality of life of adherence to gluten-free diet in adult patients with celiac disease. Rev Esp Enferm Dig 2015;107:196-201. [ Links ]
23. Szende A, Leidy NK, Revicki D. Health-related quality of life and other patient-reported outcomes in the European centralized drug regulatory process: A review of guidance documents and performed authorizations of medicinal products 1995 to 2003. Value Heal J Int Soc Pharmacoeconomics Outcomes Res 2005;8:534-48. DOI: 10.1111/j.1524-4733.2005.00051.x. [ Links ]
24. Williet N, Sandborn WJ, Peyrin-Biroulet L. Patient-reported outcomes as primary end points in clinical trials of inflammatory bowel disease. Clin Gastroenterol Hepatol 2014;12:1246-56. DOI: 10.1016/j.cgh.2014.02.016. [ Links ]
25. Silvester JA, Rashid M. Long-term follow-up of individuals with celiac disease: an evaluation of current practice guidelines. Can J Gastroenterol 2007;21:557-64. [ Links ]
26. Instituto Nacional de Estadística (Internet). Madrid. 2014 (cited 2015 May 1). Available from: www.ine.es. [ Links ]
27. Lee AR, Wolf R, Contento I, et al. Coeliac disease: the association between quality of life and social support network participation. J Hum Nutr Diet2015. DOI: 10.1111/jhn.12319. [ Links ]
28. Badia X, Roset M, Montserrat S, et al. The Spanish version of EuroQol: a description and its applications. European Quality of Life scale. Med Clin (Barc) 1999; (112 Supl):79-85. [ Links ]
29. Barratt SM, Leeds JS, Sanders DS. Quality of life in Coeliac Disease is determined by perceived degree of difficulty adhering to a gluten-free diet, not the level of dietary adherence ultimately achieved. J Gastrointestin Liver Dis 2011;20:241-5. [ Links ]
30. Ramirez-Cervantes KL, Remes-Troche JM, Del Pilar Milke-Garcia M, et al. Characteristics and factors related to quality of life in Mexican Mestizo patients with celiac disease. BMC Gastroenterol 2015;15:4. DOI: 10.1186/s12876-015-0229-y. [ Links ]
31. Wagner G, Berger G, Sinnreich U, et al. Quality of life in adolescents with treated coeliac disease: influence of compliance and age at diagnosis. J Pediatr Gastroenterol Nutr 2008;47:555-61. DOI: 10.1097/MPG.0b013e31817fcb56. [ Links ]
32. Casellas F, Rodrigo L, Vivancos JL, et al. Factors that impact health-related quality of life in adults with celiac disease: a multicenter study. World J Gastroenterol 2008;14:46-52. DOI: 10.3748/wjg.14.46. [ Links ]
33. Sainsbury K, Mullan B. Measuring beliefs about gluten free diet adherence in adult coeliac disease using the theory of planned behaviour. Appetite 2011;56:476-83. DOI: 10.1016/j.appet.2011.01.026. [ Links ]
34. Zingone F, West J, Auricchio R, et al. Incidence and distribution of coeliac disease in Campania (Italy): 2011-2013. United Eur Gastroenterol J 2015;3:182-9. DOI: 10.1177/2050640615571021. [ Links ]
35. Fernandez A, Gonzalez L, de-la-Fuente J. Coeliac disease: clinical features in adult populations. Rev Esp Enferm Dig 2010;102:466-71. DOI: 10.4321/S1130-01082010000800002. [ Links ]
36. Llorente-Alonso MJ, Fernandez-Acenero MJ, Sebastian M. Gluten intolerance: sex and age-related features. Can J Gastroenterol 2006;20:719-22. [ Links ]
37. Lucendo AJ, García-Manzanares A, Arias Á, et al. Coeliac disease in the 21st century: no longer "kids' stuff." Gastroenterol Res 2011; 4:268-76. DOI: 10.4021/gr376e. [ Links ]
38. Lucendo AJ, Rodrigo L, Peña AS. Extraintestinal Manifestations of Celiac Disease and Associated Disorders. In: In Arranz E, Fernández-Bañares F, Rosell C, Rodrigo L, Peña A, editors. Advances in the Understanding of Gluten related Pathology and the Evolution of Gluten-Free Foods. Barcelona: OmniaScience; 2015. p. 341-407. [ Links ]
39. Rostom A, Murray JA, Kagnoff MF. Medical Position Statement on Celiac Disease. Gastroenterology 2006;131:1977-80. DOI: 10.1053/j.gastro.2006.10.003. [ Links ]
40. Lucendo AJ, Garcia-Manzanares A. Bone mineral density in adult coeliac disease: an updated review. Rev Esp Enferm Dig 2013;105:154-62. DOI: 10.4321/S1130-01082013000300006. [ Links ]
41. Hjelle AM, Apalset E, Mielnik P, et al. Celiac disease and risk of fracture in adults - a review. Osteoporos Int 2014;25:1667-76. DOI: 10.1007/s00198-014-2683-8. [ Links ]
![]() Correspondence:
Correspondence:
Julián Rodríguez-Almagro.
Emergency Department.
Hospital General Universitario Ciudad Real.
C/ Obispo Rafael Torija, s/n.
13005 Ciudad Real, Spain
e-mail: jupij79@gmail.com
Received: 11-11-2015
Accepted: 19-01-2016