INTRODUCTION
The development of esophageal high-resolution manometry (HRM) has resulted in significant improvements in the identification and classification of esophageal motor disorders 1,2. Digital data acquisition with HRM has allowed the development of intuitive software tools that address resistance to flow across the esophagogastric junction (EGJ) during swallows (integrated relaxation pressure, IRP), the vigor (distal contractile integral, DCI) and timing of smooth muscle contraction (distal latency, DL) 3. However, HRM tools that assess the integrity of the EGJ barrier at baseline did not exist until recently. IRP assesses EGJ relaxation rather than resting barrier function and traditional lower esophageal sphincter pressure (LESP) is not measured using an HRM software tool. The most useful of these is the EGJ contractile integral (EGJ-CI), which combines EGJ length and vigor into a single metric that incorporates both end-expiratory LES pressure (LESP) and inspiratory augmentation 4,5,6. The EGJ-CI reflects predictable changes following surgery at the EGJ, i.e., a decrease in the value following Heller myotomy (HM) and augmentation following anti-reflux surgery (ARS) 7. Although conventional esophageal manometric values (mean basal LESP and end-expiratory LESP) continue to be used for meaningful basal EGJ assessment, the EGJ-CI can provide more intuitive and robust basal EGJ data. This technique has been endorsed by the international GERD consensus working group as a metric with the potential to improve the assessment of EGJ barrier function 8,9.
Although the IRP is extremely sensitive to define EGJ outflow obstruction in the native esophagus 10, it has now become evident that IRP is not reflective of EGJ bolus flow following disruption of the LES 11. Other techniques, including the timed upright barium swallow, high resolution impedance manometry (HRIM) and the newer intuitive HRM metrics may be needed to accurately define EGJ following achalasia treatment. The EGJ-CI has been demonstrated to reflect EGJ barrier decline following HM 7. As an extension of this EGJ-CI characteristic, we evaluated EGJ barrier function at rest, both before and after per-oral endoscopic myotomy (POEM) in patients with achalasia, using both conventional esophageal manometry metrics and EGJ-CI values. These metrics were compared to those obtained from normal controls. The aim was to assess whether the EGJ-CI was representative of EGJ barrier function and to verify whether changes in EGJ-CI values reflected EGJ disruption following POEM.
METHODS
Subjects
Adult patients (≥ 18 years) with achalasia treated with POEM, with both pre-and post-procedure HRM, were retrospectively identified at The First Hospital of JiLin University during a 3-year period between April 2013 and April 2016. The inclusion criteria included patients with a diagnosis of achalasia according to the criteria described by the Chicago Classification v 3.0 (CCv3.0) 3 that underwent POEM as part of primary management. Furthermore, all subjects underwent an esophageal HRM (Given Imaging/Sierra Scientific, Los Angeles, CA) both before and after POEM. Patients with esophageal HRM studies with artifacts precluding a definitive diagnosis of achalasia or incomplete clinical data were excluded. The control subjects included healthy volunteers with no history of gastrointestinal symptoms or upper gastrointestinal tract surgery, no significant medical conditions and who were not taking any regular medications. After informed consent, these control subjects underwent HRM as part of our institutional normative data assessment. The study protocol was approved by the Human Ethics Committee of The First Hospital of JiLin University, China.
Questionnaire
Each patient was asked to complete a questionnaire that included elements for the calculation of the Eckardt score at initial HRM assessment and following POEM. The Eckardt score 12,13 assesses dysphagia, regurgitation, retrosternal pain and weight loss. Each symptom is designated a score between 0 and 3 (0: not present; 1: occasionally; 2: daily; 3: several times a day after each meal). The degree of weight loss was also scored in a similar way (0: none; 1: < 5 kg; 2: 5-10 kg; 3: > 10 kg). The maximum possible score is 12 and higher values represent an increasing severity of symptoms.
Esophageal HRM criteria
HRM studies were performed after an overnight fast using a 36-channel solid-state catheter system (Given Imaging/Sierra Scientific, Los Angeles, CA). After calibration, the catheter was passed through an anesthetized nasal canal. A 20-second swallow-free period was obtained while the subject remained still and resting quietly in the recumbent position (landmark period), during which the basal LES pressures and EGJ-CI were calculated 14. Ten swallows were recorded using 4-5 ml of water at room temperature spaced > 20 seconds apart. HRM data were acquired, displayed and analyzed using dedicated computerized HRM software systems (ManoView; Given Imaging/Sierra Scientific, Los Angeles, CA).
Standard analysis of the motor pattern was performed using CCv3.0 3. A median IRP of > 15 mmHg was required for a diagnosis of achalasia. Esophageal body motor pattern further defined achalasia subtypes as follows: type 1, no panesophageal pressurization; type 2, ≥ 20% panesophageal pressurization; and type 3, ≥ 20% premature sequences.
EGJ metrics
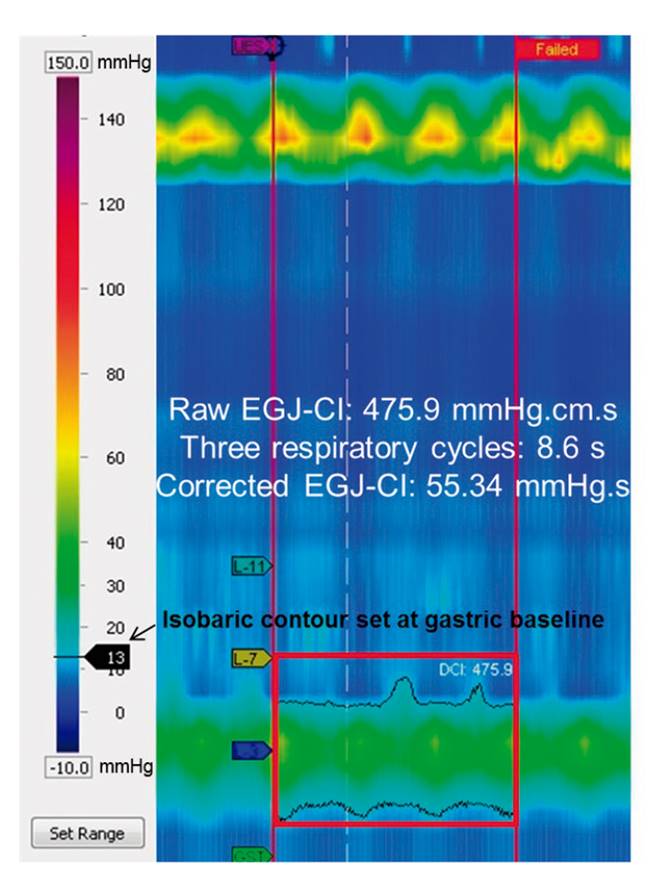
Baseline EGJ metrics were extracted during a period of quiet rest without swallows, after the patient was acclimatized to the presence of the esophageal manometry catheter, either at the beginning or the end of the study. From analysis of the entire landmark period, LESP were extracted, including mean basal LESP and end expiratory LESP, from both pre- and post-POEM HRM studies. Control HRM studies were similarly evaluated. In order to calculate the EGJ-CI, the landmark phase was used to identify three respiratory cycles, the duration of which was recorded. The EGJ-CI was calculated by forcing the distal contractile integral (DCI) measurement box across the EGJ for exactly three respiratory cycles. This DCI-like metric was recorded above the mean gastric baseline, which can be extracted using the smart mouse tool available in HRM interpretation software. After measuring the gastric baseline pressure, the isobaric contour tool was adjusted to the gastric baseline pressure to ensure that the EGJ-CI was recorded above the gastric baseline pressure. This value was subsequently corrected for respiration by dividing by the duration of the three respiratory cycles in order to yield the corrected EGJ-CI (mmHg.cm) 5 (Fig. 1).
Statistical analysis
Continuous variables are reported as mean ± standard error of the mean (SEM) or median and interquartile range (IQR), as appropriate. Categorical data are reported using frequencies and proportions. Normative values for EGJ-CI were determined from the analysis of data from normal controls. Age and gender were compared between the two groups with independent sample t-tests and Fisher's exact test, separately. The paired-samples t-test was used for the Eckardt score, EGJ-CI values and conventional LESP metrics were compared both pre- and post-POEM within the achalasia group. Pre- and post-POEM EGJ-CI values and conventional LESP metrics were compared to normal controls with the non-parametric independent-sample Mann-Whitney U test. The degree of correlation between EGJ-CI and LESP metrics was assessed with Pearson's r and Spearman's rho correlations. All statistical analyses were performed using the statistical software package SPSS version 17.0 (SPSS Inc, Chicago, IL, USA). In all cases, a value of p < 0.05 was set for statistical significance.
RESULTS
Demographic and clinical characteristics
Twenty achalasia patients underwent POEM during the 3-year study period; five patients did not undergo postoperative HRM and were excluded. Therefore, 15 achalasia patients (35.2 ± 2.5 years, 73% female) that underwent POEM with a pre- and post- procedure HRM were included in the study. Pre-procedure HRM was performed a mean of 12.0 ± 2.3 days before POEM and post-procedure HRM, 32.4 ± 1.6 days following POEM. At the time of the pre-procedure HRM, 46.7% (7/15) of cases had achalasia type 1, 46.7% (7/15) had type 2 and 6.7% (1/15) had type 3. None of the patients had received prior achalasia treatment and all underwent a successful POEM. Patients were contacted for follow-up Eckardt score assessment a mean of 11.7 ± 2.3 months after the POEM procedure. The mean pre-POEM Eckardt score was 7.0 ± 0.5 (range 4-11) and decreased to 1.5 ± 0.3 (0-3) following POEM (p < 0.001). The control group consisted of 20 healthy volunteers (26.6 ± 1.1 years, 50% female). Baseline clinical characteristics and Eckardt score are shown in table 1.
EGJ HRM metrics
Pre-POEM end expiratory and mean basal LESP were significantly higher in achalasia patients compared to controls (p < 0.001) (Table 1). As expected, 4-s IRP was also significantly higher in achalasia patients compared to controls (p < 0.001). Following POEM, both the mean basal LESP and end expiratory LESP declined compared to pre-POEM values and the final post-POEM values were statistically similar to baseline values in controls (p = 0.099 and p = 0.25, respectively). However, the 4-s IRP remained significantly higher in the achalasia patients post-POEM compared to the baseline IRP in controls (p = 0.011) (Table 1).
Table 1 Demographic and clinical characteristics and HRM metrics in the study groups
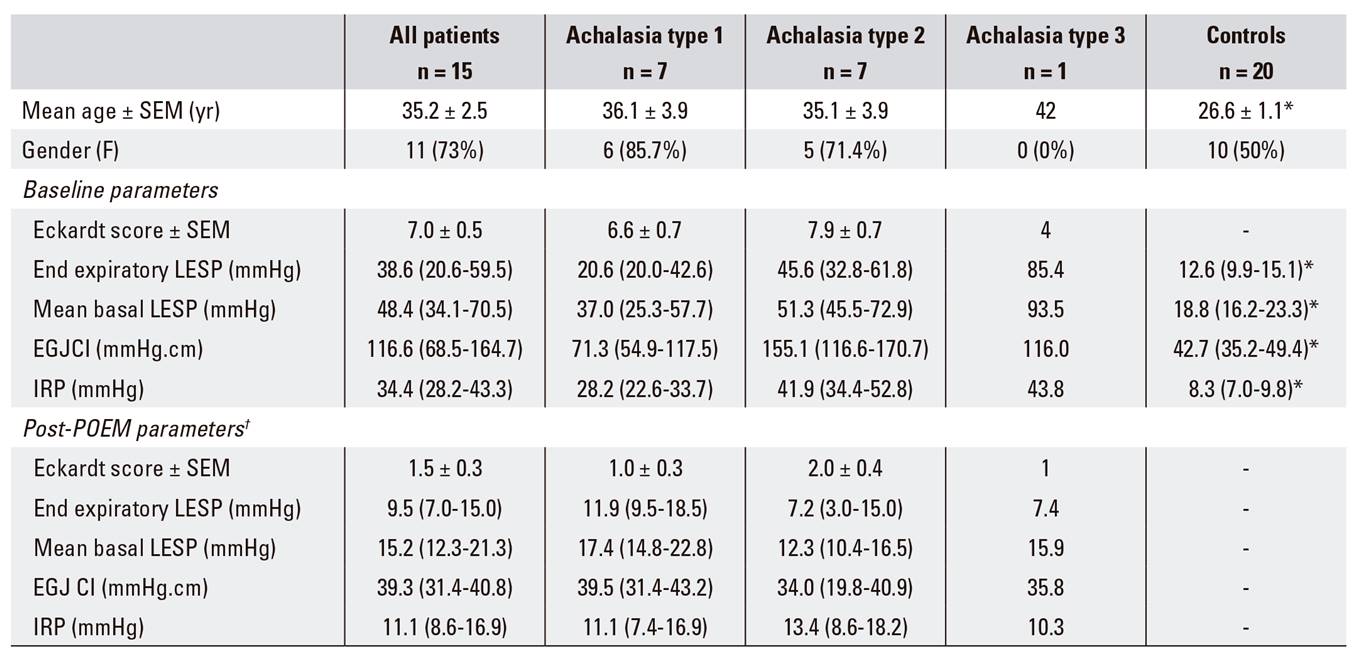
Values reported as median (interquartile range) unless otherwise indicated. *p ≤ 0.005, independent sample t-tests for age; independent-samples Mann-Whitney U test for other comparisons. Fisher's exact test for gender. †p < 0.001 for all comparisons with baseline parameters, independent-samples Mann-Whitney U test.
Similarly, achalasia patients had significantly higher baseline EGJ-CI values compared to controls (p < 0.001). Post-POEM EGJ-CI values were significantly lower (p < 0.001) compared to pre-POEM values and similar to baseline values in controls (p = 0.162) (Table 1). While baseline LESP metrics, IRP and EGJ-CI were not different between type 1 and type 2 achalasia, the degree of improvement of conventional LESP metrics and EGJ-CI after POEM was greater in type 2 achalasia compared to type 1 achalasia (p < 0.05). The degree of IRP change and improvement in the Eckardt score were similar between type 1 and type 2 achalasia (p = 0.223 and p = 0.082, respectively). There was only one patient with type 3 achalasia, therefore definitive conclusion can be made regarding this subtype.
Correlation between EGJ-CI and conventional LESP metrics
EGJ-CI correlated well with end-expiratory LESP at baseline (Pearson's r = 0.75 and Spearman's rho = 0.85, p < 0.001) (Fig. 2). A similar degree of correlation was noted with the mean basal LESP (Pearson's r = 0.79, Spearman's rho = 0.84, p < 0.001) (Fig. 3). After POEM, the correlation remained significant between EGJ-CI and end-expiratory LESP (of 0.70 and 0.77 respectively, p = 0.004) (Fig. 2) and also between EGJ-CI and the mean basal LESP (Pearson's r and Spearman's rho of 0.55 and 0.5 respectively, p = 0.033) (Fig. 3). Although the correlation metrics were less robust.
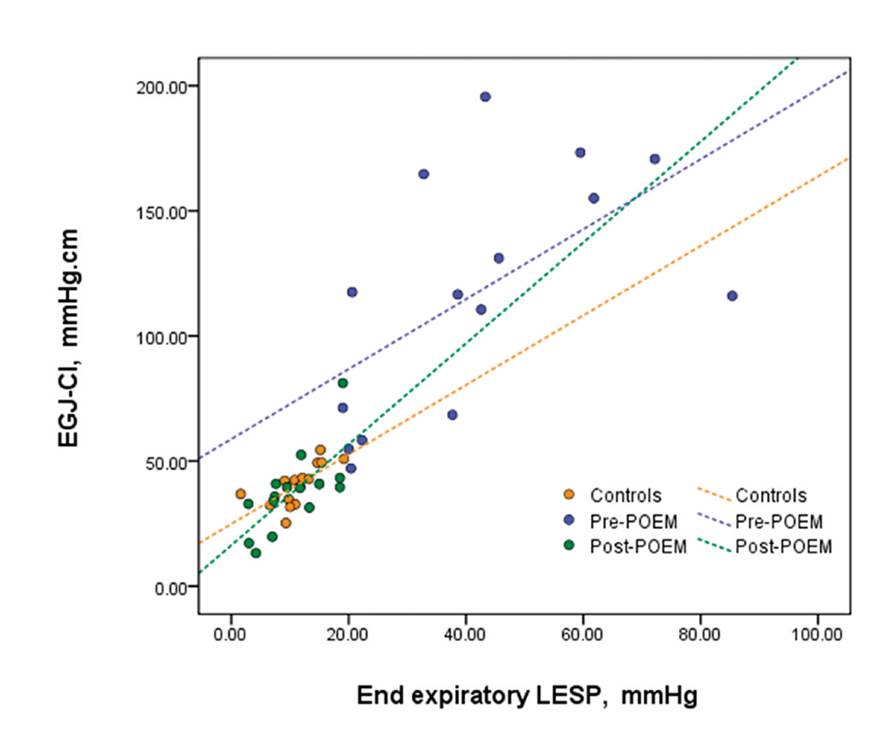
Fig. 2 Correlation of end-expiratory LESP and mean basal LESP with EGJ-CI. There was a modest correlation between these two metrics, both at baseline (Pearson's r = 0.75, Spearman's rho = 0.85, p < 0.001) and after POEM (Pearson's r = 0.70, Spearman's rho = 0.77, p = 0.004).
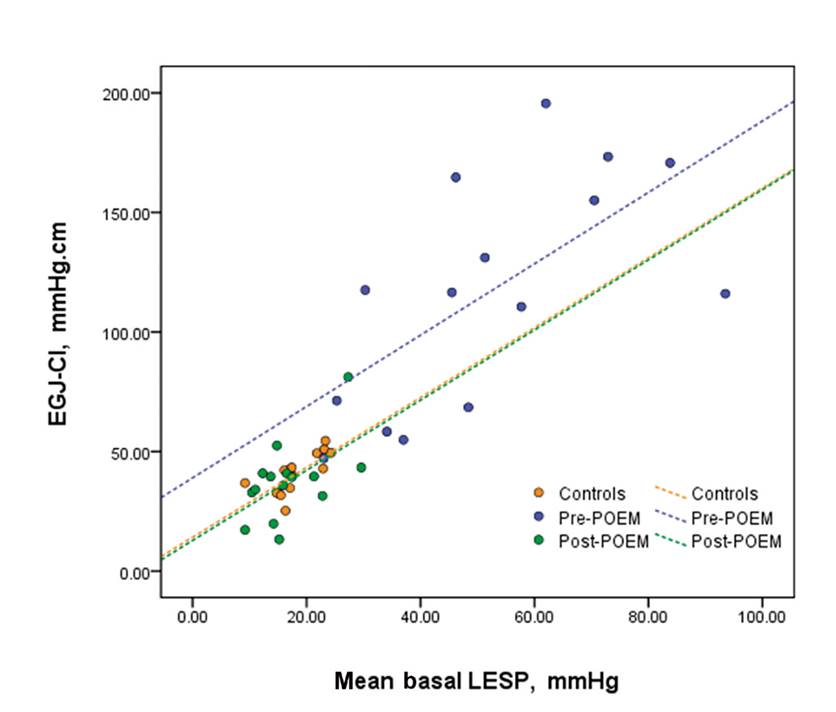
Fig. 3 Correlation of end-expiratory LESP and mean basal LESP with EGJ-CI. There was a modest correlation between mean basal LESP and EGJ-CI at baseline (Pearson's r = 0.79, Spearman's rho = 0.84, p < 0.001), although post-POEM correlations were less robust (Pearson's r = 0.55, Spearman's rho = 0.5, p = 0.033).
DISCUSSION
In this study, we further demonstrate the validity of the EGJ-CI in assessing EGJ barrier function, complementing the existing literature on the use of EGJ-CI. In particular, we report a high correlation between EGJ-CI and individual conventional basal EGJ barrier metrics and the expected reduction in the EGJ-CI to normal levels following disruption of the EGJ barrier during the POEM procedure. These findings complement existing reports demonstrating the value of EGJ-CI as a tool to assess EGJ barrier function, both in terms of assessing the adequacy of surgical intervention to the EGJ and in predicting esophageal reflux burden.
The EGJ-CI is a novel HRM metric that is gathering attention for the evaluation of the EGJ barrier at baseline. In addition to incorporating mean basal and end expiratory LESP, this metric also includes inspiratory pressure augmentation from the diaphragmatic pinch into the calculation, a parameter that has been demonstrated to be an important component of the barrier against reflux 15. Hoshino y cols. 16 first described measuring the DCI of the LES over a ten-second swallow free period (LES pressure integral, or LESPI). However, they did not use the intragastric baseline pressure as a reference and did not control for respiratory cycle duration. Nicodeme y cols. refined this metric by measuring the EGJCI value at the LES above a threshold of 2 mmHg over the gastric baseline and dividing the recorded value by the duration of three complete respiratory cycles 4, thereby making it independent of the length of the respiratory cycle. This new metric, termed the EGJ-CI, has overcome some of the limitations of the LESPI 4,5,6. The St Louis method of calculation simplifies the EGJ-CI by referencing it to the gastric baseline 5. Mean normative reported values are highly consistent in the 39-46 mmHg.cm range. Our current study also demonstrates that EGJ metrics in Chinese healthy controls have the same range as reported in Western populations. Although these values are based on very small numbers of healthy volunteers in both populations and further data from healthy controls is required.
The EGJ is a complicated structure and understanding of its barrier function is crucial in disorders that impact the EGJ, including GERD and achalasia. During the resting phase without swallows or transient LES relaxations, the EGJ barrier is composed of a stable basal intrinsic sphincter pressure as well as a dynamic crural diaphragmatic (CD) contribution that varies with the phase of respiration 17. Despite the advances made with conventional esophageal manometry for the assessment of EGJ function, the metrics used are limited in addressing EGJ competence, reflecting both intrinsic LES pressure and CD contraction components 18. The EGJ-CI allows both these components of EGJ barrier function to be captured in a single metric that also accounts for the variation in the integrity of the barrier during various phases of respiration 4. In this study, EGJ-CI correlated well with conventional LESP metrics in achalasia patients, both pre- or post-POEM. The lower correlation of EGJ-CI to the mean basal LESP compared to end expiratory LESP is due to the fact that the mean basal LESP is influenced by diaphragmatic crural contraction, which can vary with the respiratory cycle. EGJ-CI has the potential to be more convenient than conventional LESP metrics. If this metric can be designed for automated calculation by the software packages used for HRM systems, recording this metric could be even more accurate and efficient.
Achalasia is a primary esophageal motility disorder characterized by the absence of effective peristalsis and inadequate relaxation of the lower esophageal sphincter (LES), resulting in esophageal outflow obstruction 19,20. The IRP is a critical and robust metric for quantifying swallow induced LES relaxation 18,22, with a primary role in the diagnosis of achalasia and esophageal outflow obstruction 10. Recently, Salvador et al. 23 reported that an increased preoperative IRP correlated directly with LES function and severe dysphagia and was restored to normal by Heller myotomy. However, neither pre- nor post-operative IRP levels could predict treatment failures. It remains a challenge to assess the EGJ barrier function and relaxation, particularly following LES disruption in achalasia. It is now evident that the IRP is not representative of outflow obstruction or the lack thereof, following surgical intervention of the LES. Bolus flow time through the EGJ may be better assessed using a combination of esophageal pressure topography and impedance (HRIM), both in the native and disrupted esophagus 11,24. However, this is more cumbersome compared to HRM metrics, including EGJ-CI.
While the IRP remains a primary metric for the assessment of post-swallow EGJ relaxation, it does not assess the basal state of the EGJ barrier. The EGJ-CI has the potential to overcome this limitation and complement the IRP. The first step in determining this is to identify whether EGJ-CI changes reflect surgical or other interventions to the EGJ. Our data complements recent reports that this is indeed the case 7. We report in this study that EGJ-CI values approximate those seen in normal controls following successful POEM (as indicated by low post-POEM Eckardt scores), even though IRP values do not necessarily normalize. IRP values have been noted to remain high following intervention of the EGJ in achalasia 23,25, while EGJ-CI values do appear to normalize. However, it remains to be seen if normalizing EGJ-CI should be the goal in surgical or endoscopic disruption of the EGJ in achalasia and further prospective studies are required. Furthermore, low EGJ-CI values have been shown to correlate with elevated esophageal reflux burden 5,6 and future studies need to address whether the degree of EGJ-CI decline following POEM can predict GERD post-POEM.
There are a few limitations in our study. First, our sample size is small. Second, we did not compare the change in individual clinical symptom pre- and post-POEM, as we used the Eckardt score as a surrogate. Studies designed to assess the individual symptoms following POEM will be needed in order to demonstrate whether EGJ-CI can predict symptomatic outcomes or estimate the efficiency of POEM after a longer follow-up. Third, our control group was younger with different gender distributions than the achalasia patients. This reflects the difficulty in recruiting and identifying older healthy asymptomatic volunteers that are not taking medication. However, we believe these normative values are likely representative as they are similar to those reported in Western populations. Further studies in healthy volunteers of different ages are needed. Measurement of the EGJ-CI may be difficult when LES and CD pressures are low, which needs further evaluation. Finally, the EGJ-CI measurement was manually performed using the DCI tool and HRM analysis software algorithms designed specifically to measure the EGJ-CI could provide more accurate data 5. Nevertheless, we have demonstrated an overall improvement in EGJ-CI commensurate with EGJ intervention, with POEM similar to that seen with conventional EGJ metrics and similar to that reported with HM 7. Therefore, our recordings are likely representative of EGJ barrier function.
In conclusion, the EGJ-CI is a novel HRM metric that has clinical utility for the assessment of EGJ barrier function at baseline. The EGJ-CI performs well in comparison to conventional LESP metrics and combines both intrinsic LES and dynamic CD components into one single metric. Finally, this metric reflects EGJ disruption with POEM when measured following intervention, complementing IRP measurements of post-swallow residual pressure. Further studies are required to assess the role of EGJ-CI for the estimation of the adequacy of EGJ disruption and for predicting symptomatic outcomes following intervention in achalasia and GERD.