INTRODUCTION
Ameloblastic fibroma is a very rare mixed odontogenic tumor, representing only 2 % of odontogenic tumors1 and mainly affects patients in the first two decades of life, with no sex predilection, being 80 % of the reported cases located in the mandible, usually in the premolar and/or molar area2.
Despite many similarities, it is essential to differentiate the ameloblastic fibroma from other mixed odontogenic lesions because it has true neoplastic qualities3 and even malignant transformation cases have been reported4.
The effective surgical treatment includes enucleation and curettage of the surrounding bone and removal of the affected teeth5. Although recurrence of ameloblastic fibroma is rare, a long term follow up is recommended6.
Our objective is to analyze if the ameloblastic fibroma is amenable to conservative treatment and describe the main clinical characteristics and recurrence rates. We performed a literature review of ameloblastic fibroma case series published in the literature and we report our experience in 4 cases treated at the Pediatric Oral and Maxillofacial Surgery Department of Hospital La Paz in the last 15 years.
MATERIAL AND METHODS
We performed a literature review in the data base PubMed. The inclusion criteria were: articles reporting ameloblastic fibroma of the jaws cases, that had been published between 2015 and 2022 and articles in English or Spanish. Exclusion criteria included articles published earlier than 2015, articles in a language different from English or Spanish and articles reporting cases of ameloblastic fibro-odontoma or fibrosarcoma or peripheral ameloblastic fibroma.
For this research we used the following MeSH terms: ((("Ameloblastic"[All Fields] AND ("fibroma"[MeSH Terms] OR "fibroma"[All Fields] OR "fibromas"[All Fields]) AND ("jaw"[MeSH Terms] OR "jaw"[All Fields] OR ("mandible"[MeSH Terms] OR "mandible"[All Fields] OR "mandibles"[All Fields] OR "mandible s"[All Fields]) OR ("maxilla"[MeSH Terms] OR "maxilla"[All Fields] OR "maxillae"[All Fields] OR "maxillas"[All Fields]))) NOT ("odontoma"[MeSH Terms] OR "odontoma"[All Fields] OR ("Ameloblastic"[All Fields] AND "fibro"[All Fields] AND "odontoma"[All Fields]) OR "ameloblastic fibro odontoma"[All Fields])) NOT ("Ameloblastic"[All Fields] AND "Fibro-Sarcoma"[All Fields])). A total of 29 results were obtained. One article was discarded because it was written in Chinese. Seven articles describing ameloblastic fibrosarcoma cases were also discarded. Two articles describing a peripheric ameloblastic fibroma were also discarded. Seven articles presented cases of lesions different from ameloblastic fibroma and, therefore, were not included.
A total of 13 articles fulfilled the inclusion criteria, reporting cases of ameloblastic fibroma of the jaws. One article was rejected because of unavailability of full-text report. Finally, 12 articles were included.
Regarding our experience, a research was performed at the Anatomical Pathology department of our hospital and cases filed as ameloblastic fibroma that had been operated in the last 15 years were selected and analyzed.
RESULTS
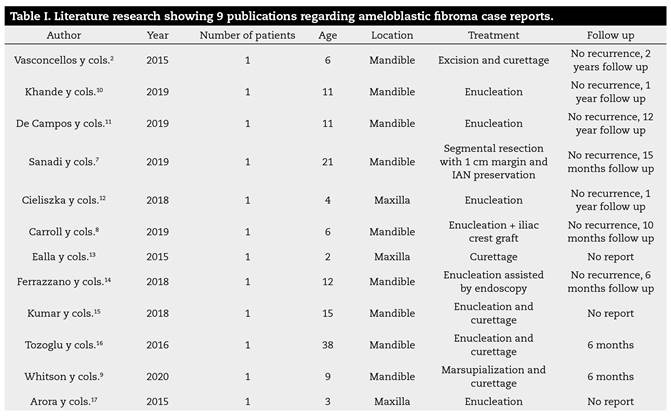
We found 12 articles reporting cases of ameloblastic fibroma of the jaws. All articles were single case reports. Mean age was 8,3 years (Range [2-38]). Only three articles (25 %) reported ameloblastic fibroma cases presenting in the maxilla. All cases were associated to unerupted teeth. Most cases underwent conservative treatment with enucleation and curettage. One patient underwent segmental mandible resection with 1 cm safe margin and IAN preservation7, and one patient underwent enucleation and received an iliac crest graft8. One patient9 underwent marsupialization and curettage, with no recurrence. Three articles did not report follow up length, for the rest of publications, the mean follow up was 26,11 months (Range [6-144]). No recurrences were reported in any of these cases. These research data is presented in Table 1. 2,9,10,11,12,13,14,15,16,17
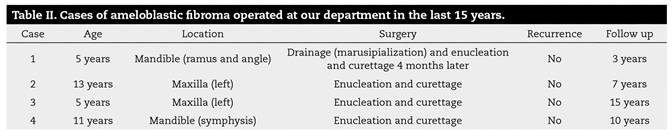
On the other hand, in the research at our hospital a total of four cases were found. Information regarding these cases is presented in Table 2. Cases 2 and 3 presented with lesions in the posterior maxilla and cases 1 and 4 in the mandible (50 %) (symphysis and left posterior mandible). The mean age was 8,5 years (range [5-13]) and we found 2 male and 2 female patients. Mean follow up was 8,5 years (range 3-15 years). Their medical, surgical, and familiar history was unremarkable.
Three patients (cases 2-4) presented with progressive unpainful swelling, and one patient referred pain (case 1). Intraorally, a hard swelling due to buccal cortical expansion was palpated. The overlying mucosa was intact, and absence of the involved teeth was noticed.
Diagnostic workup included preoperative orthopantomography and CT. A multilocular radiolucent cystic lesion with included teeth (Figure 1 and Figure 2) was noticed. The CT demonstrated a well-circumscribed heterogenous cystic lesion showing areas of density similar to liquid and others similar to soft tissue. These lesions showed an expansive behavior with cortical thinning and calcifications, with teeth inclusion.
A biopsy was performed in all cases and, in the case where the patient referred pain as well (case 1), a drainage was placed for marsupialization to alleviate intralesional pressure and pain. The biopsy confirmed the diagnosis of ameloblastic fibroma.

Figure 1. Ameloblastic fibroma in the left mandibular body and angle. A cystic lesion with impacted teeth (75) and cortical expansion is seen.

Figure 2. Surgical specimen of an ameloblastic fibroma showing a solid mass with areas of smooth surface. Grossly, ameloblastic fibroma appears as firm, lobular soft tissue mass with a smooth surface.
All patients underwent enucleation through an intraoral vestibular approach and curettage of the surrounding bone under general anesthesia. The teeth involved were also extracted. The patient that underwent marsupialization presented with infection of the surgical wound, which resolved with intravenous antibiotics (amoxicillin - clavulanic 875 mg/8 h for 7 days) and underwent enucleation and curettage of the ameloblastic fibroma four months later during her hospital stay (case 1). Also, a CT was performed, which showed an overall moderate reduction of the size of the lesion after marsupialization.
Histological examination showed a mass made of mesenchymal and epithelial components of odontogenic origin. The mesenchymal part showed primitive connective tissue that resembled the dental papilla with variable cellular density. On the other hand, the epithelial component consisted of cords and islands bordered by two tight layers of parallel columnar cells in a palisading pattern with nuclei in reverse polarity, confirming the diagnosis of ameloblastic fibroma (Figure 3).
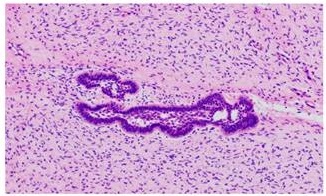
Figure 3. Histological image shows a cell-rich mesenchymal component that resembles dental papilla. In the middle two strands of odontogenic epithelium with parallel layers of hipercromatic cuboidal to columnar cells with a palisading pattern in reversed polarity.
After a mean of 8,5 years of clinical and radiological follow up, there was no evidence of recurrence in all patients, and the surgical defects were filled with bone in all cases (Figure 4). Patients underwent orthodontic treatment without incident and facial symmetry was satisfactorily restored. None of the patients required further surgery.

Figure 4. The same patient as in Figure 1, 28 months after surgery. Satisfactory bone filling is observed.
DISCUSSION
Ameloblastic fibromas are benign tumors defined by the WHO in their latest 2017 classification as mixed epithelial and mesenchymal odontogenic tumours18. These tumours are composed of both epithelial and mesenchymal elements and may show varied degrees of inductive change with formation of dental hard tissues. In this recent edition, some previously poorly defined lesions have been removed, including the ameloblastic fibro-dentinoma and ameloblastic fibro-odontoma, which are probably developing odontomas19.
Its histological features are characteristic but not specific since they may also be seen in an early developing (non-calcifying) odontoma20. Previously, if dentine was seen, the lesions were considered ameloblastic fibrodentinoma, and if dentine and enamel were noted, the lesion was named ameloblastic fibro-odontoma. However, these characteristics are indistinguishable from a developing odontoma, and it is considered that if lesions were left, they would continue to mature into fully calcified lesions19.
Up to 20 % of cases are incidentally detected upon review of routine dental radiograph3. However, most patients generally present with painless swelling of the jaw and the lesion may affect the normal eruption of teeth in the area. An impacted tooth may be associated with the tumor in approximately three quarters of the cases3. Hence, it is why it is often confused with ameloblastoma and dentigerous cyst and can be distinguished histologically by the presence of myxoid appearance of connective tissue20.
Radiographically, ameloblastic fibromas are unilocular lesions, occasionally multilocular when larger, with smooth well-demarcated borders3. AF has no specific radiologic signs and consists in generally unilocular, scarcely multilocular lesions that can mimic the scalloped outlines of unilocular ameloblastoma and the soap bubble appearance of multilocular ameloblastoma. It produces expansion or the cortical bone. Surgical excision and/or thorough curettage with removal of affected teeth is the gold standard treatment.
It is necessary to distinguish ameloblastic fibroma from ameloblastoma and ameloblastic fibrosarcoma since these later two can be locally aggressive and have greater potential for recurrence. Clinically, ameloblastic fibroma usually occurs at a younger age than ameloblastoma. Radiographic examination does not contribute to the differential diagnosis. Ameloblastic fibroma lacks specific radiological signs and generally consists in unilocular or multilocular lesions that can mimic either the unilocular ameloblastoma or the soap bubble appearance of multilocular ameloblastoma on orthopantomography. Histological examination will usually confirm the diagnosis. Ameloblastic fibroma requires a long-term follow-up due to its chances of recurrence or its transformation into ameloblastic fibrosarcoma, but there is varied rate of recurrence by different authors and mostly attributed to incomplete primary removal15.
Also, ameloblastic fibroma exhibits a more indolent clinical course than ameloblastoma and does not tend to infiltrate among trabeculae of bone. It also tends to separate from the bone more readily. Therefore, it can be treated more conservatively than ameloblastoma, and the same was advocated in our cases with complete enucleation of the tumor along with the removal of impacted teeth and posterior curettage of the surrounding bone.
This lesion is considered a benign lesion; however, recent reports have suggested that it has the potential for recurrence and malignant transformation, the ameloblastic fibrosarcoma6. Therefore, some authors have advocated a more aggressive approach of recurrent ameloblastic fibroma21. Regardless of the form of treatment, patients with this tumor must be followed up for a long period to enable the early detection of possible recurrence or development of ameloblastic fibrosarcoma.
In our research, we found 12 case reports of ameloblastic fibroma of the jaws. All articles were single case reports, which emphasizes the peculiarity of this entity. Most of the cases (75 %) were located in the mandible, in line with previous reports, and all cases were associated to impacted teeth. Enucleation and curettage were the most frequent surgical treatment applied. However, Sanadi et al.7) performed a marginal resection with a safe 1cm margin and preservation of the IAN due to concerns about recurrence. Also, Whitson et al.9 performed marsupialization in their case, with posterior curettage and no recurrence in their 6-months follow up. In most articles, the mean follow-up was short (between 6-12 months) and only one article11 reported a 12 year follow up. No recurrences were reported in any of the articles.
In our series we found 50 % of cases located in the maxilla, a higher rate compared to the literature, however, the size of the study is very limited. The mean age was 8.5 years, in line with previous reports where this lesion mostly presents in the first two decades of life. The most frequent symptom was a slowly progressive swelling, and one of them also referred pain. All four lesions showed a cystic multilocular heterogenous appearance on orthopantomography, which was confirmed on CT examination. Histology stablished the definitive diagnosis.
In all cases, enucleation of the lesion and curettage of the surrounding bone was performed, including extraction of the involved teeth. One patient (case 1) underwent marsupialization which demonstrated to reduce the size of the lesion. However, it is a not a stablished treatment of this entity and it was performed to alleviate pain and was followed by enucleation and curettage 4 months later. None of the patients showed recurrence at the longest follow up (mean 8,5 years, 15 years the longest follow up) and all four patients showed satisfactory bone filling and restoration of facial symmetry. Patients underwent orthodontic treatment uneventfully, at least 18 months after surgery.
As limitations to this study the number of patients is low due to the low frequency of this lesion. Further studies with bigger series and longer follow-up are needed to stablish recurrence rates and the risk of malignant transformation.
CONCLUSIONS
Ameloblastic fibroma is an extremely rare entity that usually appears in the mandible in young patients and can be managed in a conservative way through enucleation and curettage, with good results. In our series we did not find any recurrences and facial symmetry was restored satisfactorily.