INTRODUCTION
Free flap reconstruction of head and neck defects is a challenging and complex surgical procedure. With the recent advances in microsurgery, overall flap survival rate exceeds 95 % in most institutions1. Microvascular anastomosis is considered to be the most critical determinant of successful free-tissue transfer2,3, being venous thrombosis the main cause of vascular failure.
Anastomosis completed by hand-sewn technique using 8-0 or 9-0 nylon is a traditional and standard approach practiced for many years(3). Nonetheless, hand-sewn anastomosis (HSA) is very time-consuming, requires an exquisite and fine technique and can result in operator fatigue, which can lead to inaccurate vessel sewing 4. Furthermore, it is subject to several complications such as laceration of the endothelial lining, low patency, dehiscence, the presence of foreign bodies (sutures) in the lumen, etc. 2,5.
In recent years, the need to reduce surgical time and complications associated to the microvascular anastomosis has led to the development of new devices, and the ring pin anastomotic coupling device has been proved to be the most reliable6. The microvascular coupling device (MVCD) as we know today was described in the 90’s and has gained popularity since.
The MVCD has demonstrated in several studies to reduce operating time, minimize time of ischemia, complications and increase flap survival rates2,6,7,8,9. It is mostly used in venous anastomoses, both end-to-end and end-to-side, as the wall structure of the veins presents less of a technical challenge for mechanical anastomosis2,8. The experience in its use in arterial anastomosis is scarce and controversial6.
In this study we aim to compare the results and microanastomosis-related complications between patients undergoing head and neck free flap reconstruction either using the MVCD or the classic HSA technique for venous anastomosis.
MATERIAL AND METHODS
We retrospectively collected patients that consecutively underwent free flap head and neck reconstruction at our department between June 2016 and January 2022. The first group included patients operated before July 2018, who received the HSA technique for venous anastomosis. The second group included patients operated from July 2018 on, who received the MVCD technique. Patients in this second group in whom vessel size lower than 1,5 mm was observed intraoperatively or in whom and end-to-side anastomosis was planned underwent anastomosis using the HSA technique instead.
Data regarding age, reason for surgery, location of the defect, recipient vessels used for anastomosis, size of the coupler device used, and type of flap were collected. Complications associated to the microvascular anastomosis were recorded (thrombosis, failure of the anastomosis, bleeding, kinking etc.). Flap loss and venous thrombosis rates were calculated for both groups and compared.
The authors perform the single-venous anastomosis technique in free flap reconstruction since they believe that a double-venous anastomosis approach may reduce flow and increase the risk for venous thrombosis. There is a lack of consensus regarding superiority of one or another technique, and results in the literature are controversial 10,11. Mostly, decision to perform a second venous anastomoses should be guided by anatomical location, vessel lie, flap size, and intraoperative visual assessment 11. This topic is out of the scope of this article.
No conflicts of interest are reported by the authors. This study has been approved by the Committee in Ethics of Hospital La Paz.
RESULTS
A total of 89 patients were included. The first group included 47 patients, of whom 16 were women (34 %) and 31 were men (66 %). Mean age is in this group was 48,9 years (Range [7-88]). The main reason for surgery in these patients was squamous cell carcinoma (SCC, 51 %) and the most frequent location of the defect was the oral cavity (49 %). These data is presented in Table I.
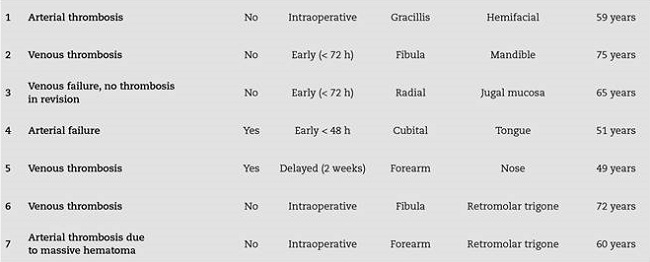
Tabla I. Main reason for surgery and location of the defect in the HSA group of patients.
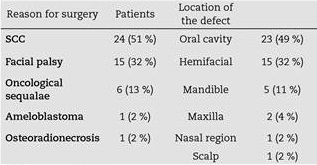
SCC: squamous cell carcinoma.
Regarding the most frequently used recipient vessels these were the facial artery (47 %), followed by the superior thyroid artery (42 %) and the facial vein (38 %) and common trunk of the internal jugular vein (IJV, 38 %). These data is presented in Table II.
Tabla II. Receptor vessels used for microvascular anastomosis in the HSA group.

IJV: internal jugular vein. EJV: external jugular vein.
Different types of flaps were used in this cohort. The flap that was used the most in this group was the gracillis flap for facial reanimation (32 %), followed by the radial forearm free flap (23 %) and the anterolateral thigh free flap (21 %). These data is presented in Table III.
Tabla III. Type of free flaps used in the HSA group.
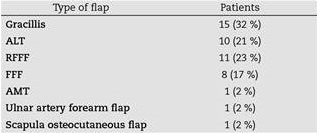
ALT: anterolateral thigh flap. RFFF: radial forearm flap. FFF: fibula free flap. AMT: anteromedial thigh flap.
The second group included 42 patients, including 20 women (48 %) and 22 men (52 %). Mean age in this group was 53,6 years (Range [10-84]). Similarly, the main reason for surgery in these second group of patients was SCC (54 %), and the most frequent location of the defect was the oral cavity (69%) Table IV. The most frequently used receptor vessels were the superior thyroid artery (43 %) and the common trunk of the IJV (43 %). These data is presented in Table V. The most frequent flap in this group was the ALT flap (45%) These data is displayed in Table VI.
Tabla IV. Main reason for surgery and location of the defect in the MVCD group of patients.
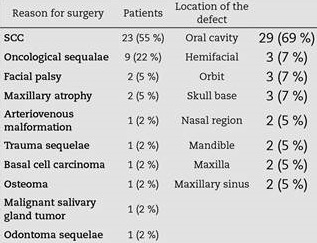
SCC: squamous cell carcinoma.
Tabla V. Receptor vessels used in the anastomosis in the MVCD group.
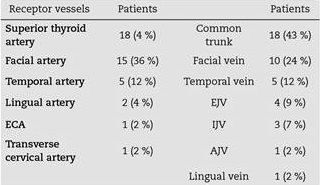
ECA: external carotid artery. EJV: external jugular vein. IJV: internal jugular vein. AJV: anterior jugular vein.
Tabla VI. Free flaps used in the MVCD group.
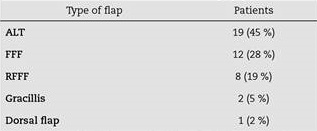
ALT: anterolateral thigh flap. FFF: fibula free flap thigh. RFFF: radial forearm free flap.
In the MVCD group, the coupler size most frequently used in the anastomosis was the 2 mm coupler device (60 %), followed by the 3mm coupler device (16%), and last the 2,5 and 3,5 mm coupler devices (12 % each).
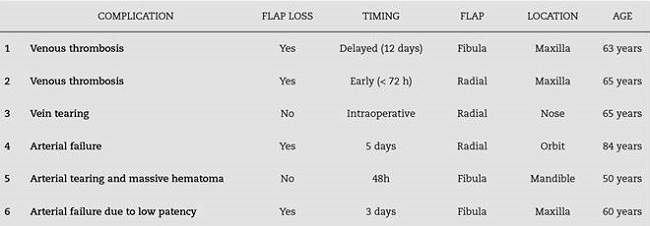
Regarding complications, in the first group (HSA) 3 cases of venous thrombosis were found (6,3 %) and one case of venous failure with congestion of the flap with no thrombosis upon surgical revision. In this group, 2 flaps were lost (4,2 %), one of them an ulnar flap for tongue reconstruction after SCC resection that was lost in the early postoperative period; and the second one was a RFFF used in nose reconstruction in oncological sequelae that was presented a delayed failure. These data are presented in Table VII.
On the other hand, in the second group (MVCD) 2 cases of venous thrombosis were found (4,7 %) and 4 flaps were lost (9,5 %). These data are displayed in Table VIII. Of these, two were FFF used for maxillary reconstruction; one was a RFFF used for maxillary reconstruction that failed in the early postoperative period; and last, one RFFF that was lost 5 days after surgery in eye socket reconstruction.
DISCUSSION
Since its introduction, the MVCD has demonstrated a good performance in microvascular anastomosis in head and neck free flap reconstruction. The MVCD is made of two high-density polyethylene rings with pins that lock between them. It is available in different sizes according to the diameter of the vessel and is used in vessels that have an outside diameter between 0,8 and 4,3 mm, with a wall thickness of 0,5 mm or less4. This device allows intima-to-intima contact between vessels, avoiding the presence of intraluminal foreign bodies, which reduces thrombosis risk and increases the patency rate2.
The main advantages of the MVCD compared to the HSA technique include decreased surgical and flap ischemia time, reduced presence of foreign bodies in the lumen, and lower skill requirements with overall similar results in terms of flap survival. Nonetheless, the use of the MCD for arterial anastomosis remains a controversial topic at present3.
In the literature, many studies have approached the differences between HSA and MVCD. In their study, Wieker et al.5) analyzed 236 patients, in which 201 reconstructions were performed via microsurgical venous coupling device (82,04 %),whereas hand sewn anastomosis was used in 44 patients (17,96 %). The overall transplant loss rate was 2.44 %. Three of the cases were operated by using venous coupling device (VCD), whereas HSA was used in three operations, being the difference statistically insignificant (p = 0,125). The rate of postoperative anastomosis-related complications demonstrated that VCD resulted in significantly lower complications compared to HSA (p = 0,028). Furthermore, the revision rate of operations using VCD was lower at (4,97 %) than the general revision rate among operations using HSA (11,36 %).
In their systematic review, Geierlehner et al.10 analyzed 32 studies and a total of 10.851 patients. 13.317 venous anastomoses were performed (1,04 venous anastomoses per flap), being the coupler sizes used ranging from 1 to 4 mm. The absolute risk of thrombosis was of 2 % in the MVCD group and 2.7 % in the HSA group, meaning an estimated absolute risk reduction of 0.7 %. They observed a lower risk of venous thrombosis for the venous coupler group (RR 0.68 [95 % CI 0.39-1.19]). When analyzing different subgroups, this difference was observed in breast reconstruction but not for head and neck or lower limb reconstruction. Furthermore, sixteen studies calculated the average time of performing a MVCD anastomosis, ranging between 3 and 15 minutes. Two of these also compared the anastomosis time of MVCD with those of HSA. This latter group took significantly longer, 20,75 vs. 9,3 mins (p = 0.001) and 24,7 minutes vs. 9 minutes (p = 0,0001).
Furthermore, Umezawa et al.4 evaluated 191 cases that underwent HSA (44, 23 %) or MVCD (147, 77 %) venous end-to-side anastomosis. The hand-sewn cases tended to involve longer venous anastomosis times than the MACD cases (31.5 versus 11.0 min, P = 0.011. In total, there were 35 complications, namely 10 (23%) in the hand-sewn group and 25 (17 %) in the MACD group. Thus, MACD tended to associate with a lower rate of venous trouble. These advantages were associated with less stress on the surgeon, as recorded subjectively, which explains why MACD was used for the vast majority of the cases after it was introduced in their hospital. They highlighted that when using MVCD, it is important to check the proper placement, the presence of twisting and caliber discrepancies. Because the coupler is hard and thick, it cannot alleviate the twist of the vein; furthermore, improper placement of the coupler can block venous blood flow in the flap due to the thickness and hardness of the coupler itself 4.
There are reports using the coupler device for arterial anastomosis, however, results are controversial. Chen et al. 6 used the coupler device for microvascular anastomosis in 45 patients, using 90 devices, half were used for arteries. The 2,0 mm coupler device was used the most, similarly to our experience. The mean duration of operating time was 7 minutes, compared to 21 minutes with the HSA technique (p = 0,0001). There was one operative arterial thrombosis among the 45 arterial anastomosis and another flap developed venous thrombosis on the second postoperative day.
Also, many authors have used the flow coupler device. Fujiwara et al. 1 retrospectively analyzed 120 patients undergoing free flap reconstruction of the head and neck in their institution and utilized the flow coupler and implantable Doppler to monitor venous outflow and arterial inflow. They found a total flap failure rate of only 0,8 %, whereas venous thrombosis was found in 10 flaps.
Regarding the size of the MVCD used, Hanson et al. 11 recently reported on venous thrombosis rates using the coupling device, reporting rates of 6.9 % using 1.5 mm venous couplers. They observed that venous anastomoses performed with couplers of larger diameter (≥ 2 mm) resulted in lower thrombosis rates. They postulate that the coupler size may have a role in the flap-related outcomes. Furthermore, Patel et al.(12 demonstrated that MVCD can overcome a discrepancy of up to 3:1. In our experience, when vessel diameter size was lower than 1,5 mm we changed to the HSA technique.
As to complications associated to the MVCD, extrusion and foreign body reaction are rare complications reported in the literature. Wu et al.(13 reported two cases of device extrusion that required removal. They performed a systematic review and found 11 cases of coupler extrusion reported in the literature and 8 cases of a palpable device. Also, they found a 2.0% rate of venous thrombosis. Partial flap necrosis (0.4 %), hematoma (0.4 %), and infection (0.3 %) were the next most common complications requiring reoperation. An interesting approach for future investigations would be to use absorbable devices to avoid such complications, specially in areas were soft tissue coverage may be thinner, such as the temporal region.
In our study, we found a lower rate of venous thrombosis in the MVCD group (4,7 % vs. 6,3 %). Despite, this difference may not be significant due to the low number of patients; larger and randomized studies are needed. Nonetheless, the success rate in the HSA group regarding flap survival was higher (4,2 % vs. 9,5 % flap loss). We believe this difference resides mainly in the fact that in the HSA group, there were 38 % of patients who underwent surgery because of facial palsy, compared to 5 % in the MVCD group, and these patients are usually healthy younger and non-smoker pa-tients. Also, the mean age was slightly lower in the HSA group (48,9 vs. 53,6 years). Overall complication rate was 14,28 % in the MVCD group, compared to 14,89 % in the HSA group. Interestingly, three of the four flaps lost in the MVCD group were used in reconstruction of maxillary defects (two fibula free flaps and one radial forearm free flap). Further studies are needed to discuss these results.
As drawbacks to this study, the two groups compared are non homogeneous since several factors such as smoking status and other comorbidities should be analyzed. Also, more facial paralysis patients are included in the HSA group, which might affect results in favor of the HSA group. Thus, results drawn from this study should be taken in consideration cautiously. Furthermore, several factors influence flap loss and microvascular anastomosis failure, such as comorbidities, smoking status, peripheral vascular disease, etc. Larger, randomized studies considering such factors are needed to assess the role of MVCD in head and neck free flap reconstruction and its comparison to the classical HSA technique.
Also, surgical time could not be measured due to the retrospective nature of this study, but it would be interesting to analyze time saving with the use of the MVCD, as well as the learning curve in young trainees.
In conclusion, the MVCD might be a safe alternative to the classic HSA technique, simplifying microanastomosis in free flap head and neck reconstruction, and significantly lowering the difference in surgical experience associated to the HSA technique. Understanding its limitations, indications and benefits can improve the surgical experience and improve outcomes.