Introduction
Attributions and related biases are particularly relevant to the development and maintenance of positive symptoms in psychosis (Howes & Murray, 2014) and depressive symptoms in mood and psychotic disorders (Davidson et al., 2018). Some studies in psychosis show that the attributional style is probably a separate construct of social cognition since it minimally correlates with other domains (Buck et al., 2016). Bentall et al. (2001) differentiate two biases: a general tendency to make non-self-attributions, including people and circumstances, for positive events (“externalising bias”) and a specific tendency to blame others for negative events (“personalising bias”). Individuals who usually tend to explain disturbing events in terms of external (non-self) causes may be particularly prone to develop delusional beliefs about such experiences (Langdon et al., 2013). On the other hand, several studies observed a higher tendency to attribute positive events (but not negative) to oneself (So et al., 2015), but other studies did not (Achim et al., 2016). Moreover, persecutory delusions caused by an externalising attributional bias maintain self-esteem preserved in persons with delusions (Murphy et al., 2018). By contrast, later research from the “defence model” of persecutory delusions predicts that people with this kind of delusions have lower self-esteem than people with depression and a greater externalising bias (Murphy et al., 2018). Connecting depression and psychosis, the Learned Helplessness Model (Abramson et al., 1978) and the Hopelessness Theory of Depression (Liu et al., 2015), provided an important framework for explaining the development of depressive symptoms through specific attributional patterns and had an initial use in the field of psychosis. These initial studies showed that persons with depression present an abolished “self-serving bias”, often named “depressive realism”, or a tendency to internalise blame for negative events (Moritz et al., 2007) and found the opposite pattern in persons with paranoid delusions, including an excessive tendency to attribute positive events to oneself and negative events to external causes, indicating an increased “self-serving bias” (Moritz et al., 2018). However, the way these biases influenced social functioning (SF) remained unexplored. Lysaker et al. (2004) using the Attributional Style Questionnaire (ASQ; Peterson et al., 1982), the main instrument derived from the attributional theory of depression, revealed inconsistencies of the model when relating attributive style to positive psychotic symptoms (externalising bias) and found that it is the tendency to see life events as the result of unstable or unpredictable causes (unstable attribution bias) which is associated with a worse SF in psychosis, regardless of symptoms. However, recent studies notice that several attributional biases as hostility, guilt, or aggressiveness are not associated with SF, unlike other social cognition domains, such as the Theory of Mind or emotion perception (Saffarian et al., 2018). Currently, the prevalence of depressive disorders in schizophrenia is estimated at around 40% and is correlated with poorer outcomes (Berardelli et al., 2019). Beyond this, “hopelessness”, regardless of depressive symptoms, predicts a worse global functioning and is an important risk factor for suicidal behaviour (Cassidy et al., 2018). Given the importance of depressive symptoms (Berardelli et al., 2019; Davidson et al., 2018) and the increased “helplessness” (a bias to externalise both positive and negative events) found in persons with psychosis (Lincoln et al., 2010), the present study aimed to verify whether the reformulated Learned Helplessness Model and the more fully articulated form, Hopelessness Theory of Depression, may be specifically suitable to predict depressive symptoms in persons with schizophrenia-spectrum disorders. Moreover, our principal focus is not to demonstrate the relationship between attribution styles and psychotic symptoms that influent models satisfactorily explain (Bentall et al., 2001; Garety & Freeman, 2013; Moritz et al., 2018; Murphy et al., 2018) but to test their utility to explain increased depressive patterns and predict SF in persons with schizophrenia-spectrum disorders. A cross-sectional study was designed with the following objectives: 1) to compare attributional styles between a group of persons diagnosed with schizophrenia-spectrum disorders vs. a non-clinical group; 2) to check possible relationships between attributional styles and the severity of depression, delusional beliefs, and other psychotic symptoms within the clinical group; and 3) to generate prediction models of SF through attributional dimensions.
We hypothesize that: 1) there will be significant differences in attribution styles between groups; 2) the clinical group will show an increased “depressive pattern” (internal, stable, and global attribution for negative situations, and the opposite pattern for positive ones), and a more “pessimistic” style; 3) an internal, stable, and global attribution for negative events (and the opposite pattern for positive ones) will predict depressive symptoms within the clinical group; 4) results will replicate classical studies in the field (Lysaker et al., 2004), finding that an unstable attribution bias is associated with a worse SF in psychosis, regardless of symptoms. We expect to confirm the suitability of the Learned Helplessness Model to predict depression and a “hopelessness pattern” in persons with schizophrenia-spectrum disorders, and its possible utility in predicting psychotic symptoms and SF.
Method
Participants and Procedure
A total of 55 adults participated voluntarily in the study. The initial clinical group involved 30 individuals diagnosed with a psychotic disorder according to Diagnostic and Statistical Manual of Mental Disorders, 5th edition (American Psychiatric Association, 2013). Five patients did not complete full evaluation and were removed from the study. Finally, 25 participants composed the clinical sample. They were recruited via public mental health centres from Castellon and Valencia (Spain). The inclusion criteria were: 1) diagnosis of schizophrenia, schizoaffective or other psychotic disorder, 2) aged 18-65, 3) clinical stability, 4) medication-stabilised condition, 5) no history of drug abuse in the last four weeks, 6) ability to provide the written informed consent, 7) native Spanish language, and 8) complete all assessment measures. Seventeen participants (68%) had a diagnosis of schizophrenia, 6 (24%) were outpatients, 9 (36%) were attended in a day rehabilitation centre, and 10 (40%) were inpatients. The non-clinical group involved 30 individuals with no history of mental health problems, recruited as a convenience sample (age and gender) in the same geographic area. Demographic data were collected and the Attribution Style Questionnaire (ASQ) was completed. No measure of psychiatric symptoms was obtained, except the general question: “Have you ever had mental health problems?”. The assessment procedure was conducted by the first author (a psychologist with a master’s degree and PhD student) who was trained and supervised by the second author (a senior clinical psychologist with a PhD degree). The study complied with the Declaration of Helsinki ethical standards. The aim and conditions were verbal and written described to prospective participants and all of them provided written informed consent.
Instruments
Attributional styles were assessed using the Spanish version of the Attributional Style Questionnaire (ASQ; Peterson et al., 1982; Sanjuán et al., 2009). It consists of 12 hypothetical situations, 6 positive and 6 negative. A score can be obtained for each of the attributional dimensions (internal, stable, and global) for both positive and negative events separately; two global scores, corresponding to the attributional styles for positive and negative situations, three dimensions for internal, stable or global bias for all events, a self-serving bias, a score that would reflect the tendency to over-attribute positive events to internal causes and negative events to external causes, and a composite index that fits the subject’s explanatory style in terms of pessimism or optimism. According to Sanjuán et al. (2013), the original version obtained internal consistency of alpha coefficients between .70 and .73 for the negative attributional style, with better properties for the Spanish version (Cronbach’s alpha between .74 and .80).
Symptom severity was evaluated using the Positive and Negative Syndrome Scale (PANSS) (Kay et al., 1987; Peralta & Cuesta, 1994). It is a semi-structured interview comprising 30 items, which assess positive and negative symptoms and general psychopathology. Summing subscales scores can derive a total symptom score. The instrument was shown to be reliable with Cronbach’s alpha coefficients of .73 for the Positive Syndrome scale, .83 for the Negative Syndrome, and .79 for the General Psychopathology scale (Kay et al., 1987).
Peters Delusions Inventory (PDI-21; Peters et al., 2004; López-Ilundain et al., 2006) is a hetero-applied instrument consisting of a total of 21 items. A total score and three subscales (conviction, worry, and stress) can be obtained. The inventory has shown an internal consistency coefficient of .91.
Table 1. Clinical and Demographic Characteristics of the Sample

Note. z (Kolmogorov-Smirnoff). PANSS = Positive and Negative Syndrome Scale; PDI-21 = Peters Delusions Inventory; BDI-II = Beck Depression Inventory.
* p < .01.
The Beck Depression Inventory-II (BDI-II; Beck et al., 1996; Sanz et al., 2003) is a self-applied 21-item scale. Its objective is to identify and measure the severity of typical symptoms of depression in adults and adolescents. The scale provides a total score that is the sum of scores on each of the items. BDI-II obtained alpha coefficients of .88 for general population and .92 for patients.
Social functioning was assessed using the Spanish short version of the Social Functioning Scale (SFS-R; Alonso et al., 2008). SFS (Torres & Olivares, 2005) was designed to evaluate SF in schizophrenia through a medical interview. The original 78 items were reduced to 15. The SFS-R includes five areas: 1) social isolation, 2) interpersonal communication, 3) independence-execution, 4) independence-competence, and 5) employment-occupation and allows a total score. The short form had a Cronbach’s alpha of .76 and proved to be reliable for use in clinical practice. In the present study, we excluded employment related items and preferred to use a more objective measure (current employment status).
Statistical Analysis
Statistical analyses were performed using SPSS version 25.0. Mean and standard deviation were used to evaluate descriptive data. Differences between the means of the two groups were evaluated through Student’s t-test for two independent samples and Cohen’s d to calculate the effect size. Bivariate correlations were used to observe relationships between attributional styles, clinical variables, and SF within the clinical group. Multiple linear regressions with stepwise method were conducted to check possible predictors of clinical variables. The criterion was: probability of F to enter ≤ .05; probability of F to eliminate ≥ .10. Psychotic symptoms (PANSS scores) and delusion severity (PDI-21scores) were considered as dependent variables. Age and gender were forced to enter in the first step as possible confounding variables. In the second step, BDI-II and ASQ scores were introduced. In the case of Depression (BDI-II), same method was used in the first step. In the second step, PANSS scores were introduced. In the last step, ASQ scores were introduced. Finally, multiple linear regressions with the same stepwise method were conducted to check possible predictors of SF areas controlling for BDI-II (weighted least squares regression). To avoid possible collinearity between variables, only ASQ composite indexes were included as possible predictors in the last step.
Results
Demographic and clinical characteristics of the participants are shown in Table 1.
Differences between Groups in Attributional Styles
Statistically significant differences were found between both groups for most attributional styles with moderate to large effect sizes (Cohen’s d). Table 2 shows differences between groups in attributional styles. The clinical group was significantly more “pessimistic” (t = -5.69, p < .001).
Table 2. Comparison between Groups in the Attributional Styles (ASQ)

Note. ASQ scores range from 1 to 7. The closer to 7, the more indicative of an internal, stable and global attribution. (-) means “attribution for negative events”. (+) means “attribution for positive events”. The Composite index is a general indicator of “optimism-pessimism”: lower scores suggest a general pessimistic trend.
*p < .05, **p < .01, ***p < .001.
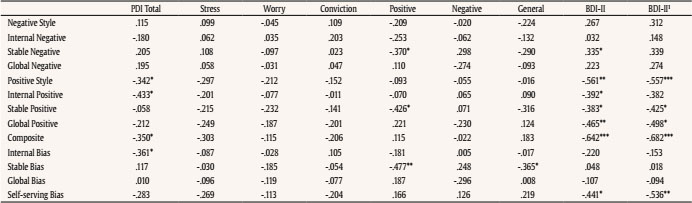
Correlations between Attributional Styles and Clinical Variables (Clinical Group)
An unstable attribution tendency (for both negative and positive events) correlated with positive symptomatology (PANSS positive) and PANSS general psychopathology. Although no significant relation was found between any attributional style and negative symptoms, a stable attribution for negative events (r = -.49, p < .01) and positive events (r = -.37, p < .05) was significantly related to the predominance of negative symptomatology measured by PANSS composite (result not shown in tables).
Regarding relationships between attribution and delusional beliefs, significant correlations were found between the severity of delusions (PDI-21 total score) and an external attribution for positive events, a positive attribution style (inversely), an externality bias, and a pessimistic style (ASQ composite index).
A stable attribution for negative events and an external, unstable, and specific attribution for positive events correlated with depression (BDI-II). A self-serving bias also correlated (inversely) with depression. A general “pessimistic” trend, measured by the ASQ positive-negative composite index, highly correlated with depression (r = -.642, p < .001). Correlations are shown in Table 3a. To demonstrate that relations between attributional styles and depression were not influenced by psychotic symptoms, partial correlations were calculated controlling by positive, negative, and general symptoms. Correlations remained significant (see Table 3a).
Correlations between Attributional Styles and Clinical Symptoms with Social Functioning
General psychopathology inversely correlated with General SF, independence-execution and independence-competence. Correlations between clinical symptoms and attributional styles with SF areas are shown in Table 3b.
Table 3b. Bivariate Correlations within the Clinical Symptom. Attribution Styles and Clinical Symptoms with Social Functioning

Note. PDI-21 = Total, Stress, Worry, and Conviction. PANSS positive symptoms, negative symptoms, and general psychopathology. 1BDI-II = score. 1BDI-II: Partial correlations (df = 20) controlling by PANSS positive, negative, and general psychopathology. SFS-R: Social Functional Scale. Total (general social functioning), social isolation, interpersonal communication, independence-execution, independence-competence. Employment status (negative correlations mean better employment status).
*p < .05, **p < .01, ***p < .001.
Correlations between Educational Level, Employment, Attributional Styles, and Social Functioning
A stable and global attribution for positive events correlated to educational level. The employment status was related to an internal, stable, and global attribution for positive events, and with an internal attribution for negative events. Employment was also related with general SF. A higher educational level and a better employment situation correlated with a lower social isolation. The full correlation matrix is shown in Table 4.
Table 4. Correlation matrix.
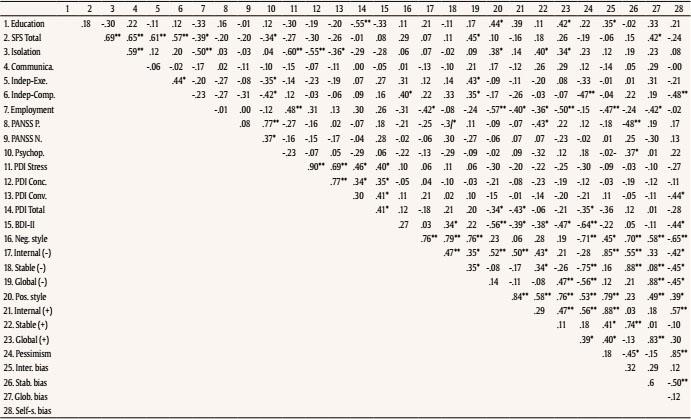
Note. 1. Educational level; 2. General social functioning; 3. Social isolation; 4. Interpersonal communication; 5. Independence-execution; 6. Independence-competence; 7. Employment status; 8. PANSS positive; 9. PANSS negative; 10. PANSS general psychopathology; 11. PDI-21 stress; 12. PDI-21 worry; 13. PDI-21 conviction; 14. PDI-21 Total; 15. BDI-II; 16. Negative attribution style; 17. Internal negative; 18. Stable negative; 19. Global negative; 20. Positive attribution style; 21. Internal positive; 22. Stable positive; 23. Global positive; 24. Pessimistic style; 25. Internal bias; 26. Stable bias; 27. Global bias; 28. Self-serving bias.
* p < .05. ** p < .01.
Employment status was considered as a nominal variable (1 = study or work, 2 = unemployed, 3 = pensioner). For practical purposes we have considered condition 1 as the most satisfactory and condition 3 as the least satisfactory. Therefore, negative correlations would indicate a positive relationship.
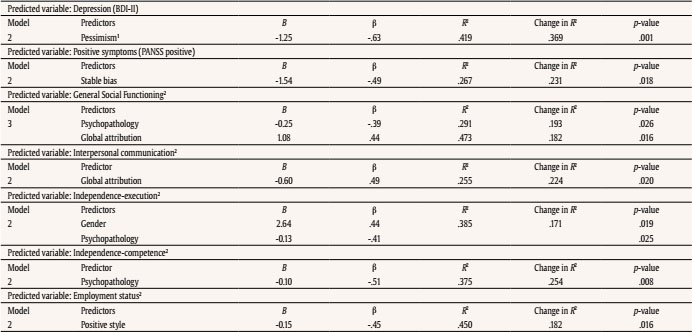
Multiple Linear Regressions
A general “pessimistic” style predicted over 40% of the variance in depression, F(3, 21) = 5.00, p = .009.
An unstable attribution bias predicted more than 25% of the variance in positive psychotic symptoms, F(3, 21) = 2.55, p = .08. No model predicted adequately negative symptoms, general psychopathology, or delusion severity.
Regarding SF, after weighting for depression, PANSS general psychopathology predicted a worse general SF and a global attribution style predicted a better one, F(4, 20) = 4.49, p = .009. A global attribution predicted better interpersonal communication, F(3, 21) = 2.40, p = .09. General psychopathology predicted a worse independence-execution, F(3, 21) = 4.39, p = .015, and a worse independence-competence, F(3, 21) = 4.19, p = .018. A positive attribution style predicted a better employment status, F (3, 21) = 5.72, p = .005. No model predicted adequately social isolation. Table 5 summarises all regression models that were predictive.
Discussion
Results provide evidence for the utility and adequacy of both reformulated Learned Helplessness Model (Abramson et al., 1978) and its more fully articulated form, the Hopelessness Theory of Depression (Davidson et al., 2018; Haeffel et al., 2017), to predict depression in persons with schizophrenia-spectrum disorders. Comparing to a non-clinical group, persons with psychosis show an increased negative attribution bias. Moreover, the clinical group shows a “pessimistic” attribution bias as an important differential trait comparing to controls, with a great effect size. The finding agrees with some studies linking optimism to better mental health levels (Yuan & Wang, 2016). Within the clinical group, “pessimism” predicted more than 40% of the variance in depressive symptoms according to predictions of the Theory of Hopelessness of Depression (Haeffel et al., 2017). Although our results demonstrate the hypothesis that people with psychotic disorders have a “depressive” attribution style, we find no difference in the internal attribution for negative situations. The internal-external dimension has shown low-reliability coefficients, which could be due to a problem of consistency of internality attributions itself (Sanjuán et al., 2013) and should be considered when interpreting the results of this and other studies.
Interestingly, in the current study, an abolished “self-serving bias” (a tendency to internalize blame for negative events) (Moritz et al., 2007) is related to depressive symptoms and to a pessimistic style. Other previous studies find the opposite pattern in persons with paranoid delusions, including an excessive tendency to attribute positive events to oneself and negative events to external causes, indicating an increased “self-serving bias” (Candido & Romney, 1990; cited by Moritz et al., 2018). Additionally, to demonstrate that relations found between a “depressive” attributional style and depression severity are not influenced by psychotic symptoms, we calculated partial correlations controlling by positive, negative, and general psychopathology, and results remained significant. This could be an important finding to support our hypothesis about the suitability of the Learned Helplessness Model to predict depression in persons with psychosis, regardless of psychotic symptoms.
Regarding delusions, some studies employing the ASQ provide support for the hypothesis that delusional persons show an externality bias when attributing causes for negative events, although internal attributions for positive events are not found (Aakre et al., 2009). This bias is more linked to psychosis in general (e.g., Jolley et al., 2006), while more recent studies find that persons who tend to explain negative events by external causes are more specifically prone to delusional beliefs about such experiences (Langdon et al., 2013). In our study, it is the tendency to view life events as the result of unstable or unpredictable causes (unstable attributional bias) and not an externalising bias for negative events which better predicts the severity of positive symptoms, according to our hypothesis and to Lysaker et al.’s (2004) findings. Some studies find increased helplessness (a bias to externalise both positive and negative events) in psychotic patients (Lincoln et al., 2010). An external attribution bias for positive events (but not for negative ones) is related to the severity of delusional beliefs, which is partially in line with these previous studies (Achim et al., 2016; So et al., 2015).
The belief that the causes of both positive and negative events are generalisable and relate to many areas of our lives (a global attribution style) predicts a better general SF and better interpersonal communication in people with psychotic symptoms. However, contrary to Lysaker et al. (2004), negative symptoms are not related to a worse SF, but an unstable attribution bias is significantly related to the predominance of negative symptoms. Higher scores in general psychopathology also predict lower independence for daily life activities. A higher educational level, a better employment status and a stable attribution for positive situations are related to less social isolation. Persons with psychosis who believe that positive events of their lives are stable and predictable enjoy better social relationships and are less isolated, according to Lysaker et al. (2004) that suggest a stable attribution as the most related style to different measures of SF.
Finally, people with psychosis who have a positive attributional style (internal, stable, and global attribution for positive situations) are more likely to remain active.
The results presented here seek to update classical studies based on the theory of attribution from the learned helplessness model and should be put in the context of recent research. So, Moritz et al. (2018) notice that, despite the heterogeneity of attributional styles, there is growing evidence to suggest that people with schizophrenia share a tendency to “monocausal” or one-sided attributions: they do not spread the potential causes for events across different factors (“myself”, other persons or circumstances), confine the causal search to one predominant source (Mehl et al., 2014; Moritz et al., 2015), and is related to a widely studied reasoning bias such as “jumping to conclusions” (Moritz et al., 2018). The attributional style seems more “a thinking style” related to personality than a social cognition domain and it is associated with paranoid traits and not exactly with psychotic symptoms (Savla et al., 2013). Some people in the early stages of the disease are characterised by a paranoid or hostile cognitive style that could be considered as a risk factor for developing delusional belief systems (Garety & Freeman, 2013) and predisposes individuals to develop a psychotic disorder (Healey et al., 2016). Cognitive-behavioural interventions and other addressed to social cognition and reasoning skills have demonstrated that changes in these domains could improve symptoms and SF in psychiatric patients (Horan & Green, 2019; Javed & Charles, 2018).
Our study presents some limitations. First, the small sample size does not allow us to easily generalise the results. Also, a significant portion of clinical subjects was long-term patients treated in psychosocial rehabilitation services, so young patients or those with early psychosis would be underrepresented in the sample. Similarly, since we aimed to test the validity of the Hopelessness Theory of Depression, a group with depression disorders would have been more suitable as a control. Another limitation is the cross-sectional study design that hinders the determination of causal relationships since it is impossible to know whether attribution styles that patients relate preceded the onset of symptoms and influenced SF outcomes or, on the contrary, symptoms modified attribution styles at the present moment. Given that persecutory delusions are especially related to some attributional styles, another problem of our study is the impossibility to compare differences between delusional and non-delusional participants due to the small sample size. We partially improved this limitation by relating attributional styles to delusion dimensions assessed by the PDI-21.
Finally, future research based on longitudinal design studies and more appropriate samples could improve some of these limitations, as well as more ecological assessment methods to avoid shortcomings of attributional style self-report measures. These future studies should attempt to address the issue of how attribution biases relate to the development of psychosis and their interaction with social cognition and other psychological or environmental factors, such as attachment experiences or childhood trauma, to predict SF in persons with schizophrenia-spectrum disorders.
The reformulated Learned Helplessness model provides utility to predict depression in people with schizophrenia-spectrum disorders regardless of psychotic symptoms. The mechanism seems to involve a “pessimistic” bias towards the interpretation of life events. An unstable attribution bias (but not an externalising one) turns out to be more predictive to explain positive symptoms and a global attribution style predicts a better social functioning in people with psychotic disorders. Recent models highlighting the existence of a “monocausal” attribution of events seem to be more adequate to understand the mechanisms of delusions through reasoning biases and could be a risk factor to develop psychosis. How attribution biases and impairments in cognition dimensions interact modifying social functioning remains unclear. If attribution biases and other social cognition domains are involved in the formation of psychotic symptoms and predict social functioning, their inclusion as a core target within psychological intervention programs would be mandatory. Moreover, since hopelessness predicts a worse global functioning and is a risk factor for suicidal behaviour, its assessment must be an essential issue to protect and promote the recovery of people with schizophrenia-spectrum disorders.