Frontotemporal atrophy comprises the degeneration of frontal and temporal lobes, due to neuronal loss associated with different pathophysiological processes (Tartaglia & Mackenzie, 2022). The cerebral small vessel disease is mainly characterized by the presence of cerebral microinfarcts, white matter chronic ischemia, or cerebral microhemorrhage (Elahi et al., 2023). Patients with both frontotemporal atrophy and small vessel disease present cognitive symptoms that may progress to dementia.
In this context, the neuropsychological assessment is essential to determine the severity of cognitive symptoms and their emotional and behavioral impact. In addition to psychometric instruments, clinical and research practice in neuropsychology includes objective or psychophysiological assessment tools. These include quantitative electroencephalography (qEEG), which is commonly used in the study of neurodevelopmental and neurocognitive disorders among psychophysiologists (Galiana-Simal et al., 2020). A qEEG is a computer analysis of the EEG signal for the calculation of quantitative parameters, allowing a more in-depth study of brain functioning and dynamics than traditional EEG. For each frequency range (delta, theta, alpha, beta, and gamma) absolute power, relative power, power ratios, and connectivity measures are generated (Livint Popa et al., 2020). It also allows the application of algorithms for the precise localization of the signal source by Low-Resolution Electromagnetic Tomography (LORETA; Ikeda et al., 2019). All measures can be compared with a normative or clinical reference database to estimate deviations, allowing the association between the neuropsychological profile with objective measures of brain functioning. However, despite its safety, low cost, and objective information provided, its potential remains unknown to many professionals.
The aim of this study is to show the usefulness of qEEG as a complementary tool to neuropsychological and neuroimaging evaluation. Specifically, we show the diagnostic process of a case of frontotemporal dementia and small vessel disease in a patient who visited for difficulties in expressive language after 14 years of slow progression. The associations between neuroimaging and neuropsychological findings with psychophysiological qEEG data are discussed.
Case Study
A retired businessman aged 77, with basic education, married, with one daughter, and no toxic habits, visited a primary care unit with her wife, reporting behavioral changes, social withdrawal, and depressive symptoms that approximately began at age 65. In addition, his wife indicates language problems, which have worsened over the years, decreasing in spontaneity, frequency, and fluency, that are progressing into monosyllabic communication. The patient’s medical history includes hypertension, type 2 diabetes, and dyslipidemia under pharmacological control and periodic follow-up. There were no family antecedents of dementia or other neurological or psychiatric diseases. Informed consent was obtained for the anonymous publication of clinical data with research objectives.
Physical examination of the patient showed no relevant findings. The mental status examination showed evident alteration of the communicative capacity and possible depression. Complementary tests included blood tests, cranial magnetic resonance imaging (MRI), 18F-fluorodeoxyglucose positron emission tomography-computed tomography (FDG PET-CT), and neuropsychological evaluation. In addition, EEG activity of 19 cortical positions according to the 10/20 system was recorded under a resting eyes-closed state with linked-ears reference, for subsequent complementary qEEG analysis.
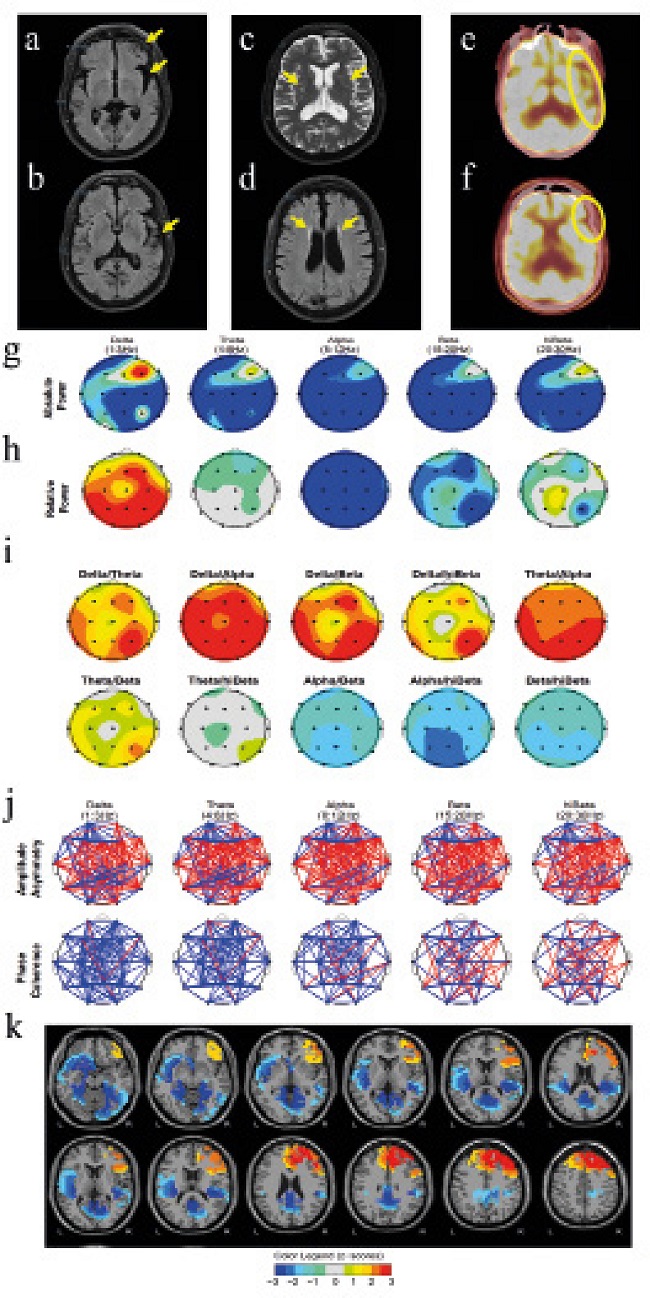
Regarding the blood test, it revealed no alterations. The MRI study showed cortico-subcortical atrophy with frontal and temporal predominance (Figure 1a-b) and hyperintensities in white matter of bilateral subcortical and periventricular areas due to microlesions of vascular origin (Figure 1c-d). The FDG PET-CT study showed frontotemporal hypometabolism with marked predominance in the left hemisphere (Figure 1e-f). The metabolic activity of the basal ganglia, thalamus, midbrain, brainstem, and cerebellum showed no alterations.
The neuropsychological assessment was performed after an initial semi-structured interview, with the instruments detailed in Table 1. A first cognitive screening round revealed mild to moderate cognitive impairment (Mini-mental state examination 24/35, Montreal cognitive assessment 18/30) with substantial impairment in delayed and working memory, verbal fluency, and sentence repetition.
Table 1. Results of Neuropsychological Assessment, Neuropsychiatric Screening, and Functional scales.
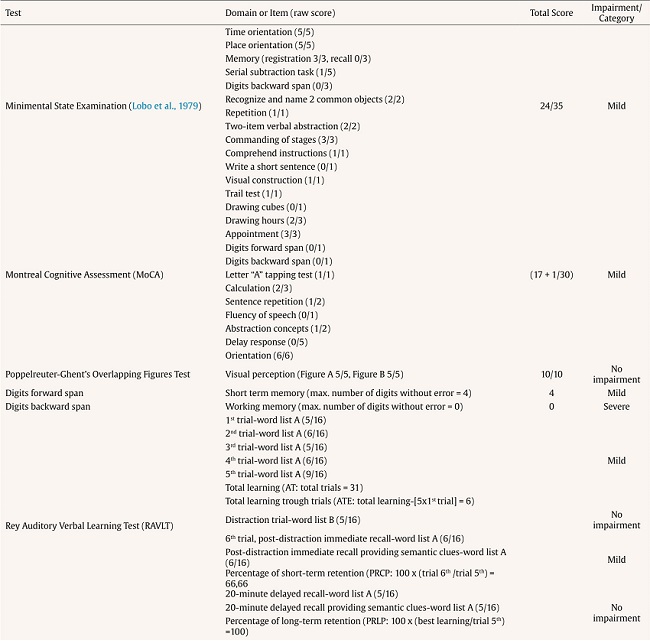
Table 1 (cont). Results of Neuropsychological Assessment, Neuropsychiatric Screening, and Functional scales.
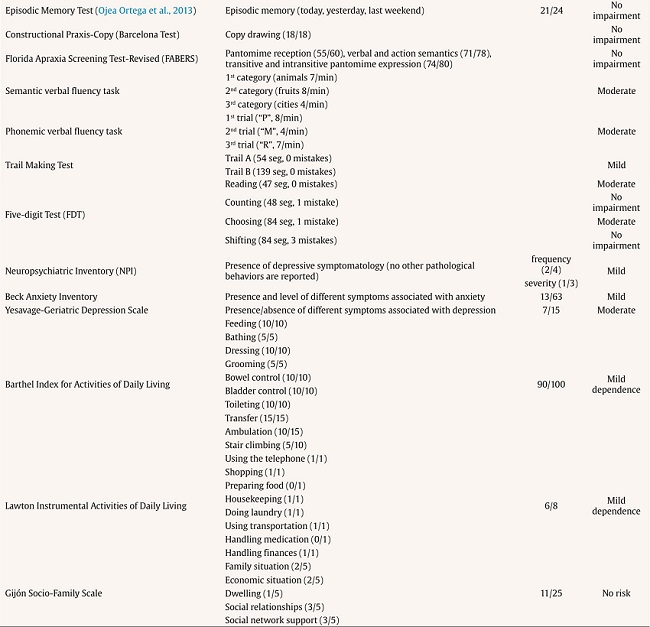
Further examination (Table 1) showed mild impairment in digit forward span, verbal learning ability, semantic and verbal fluency, automatic reading, inhibitory ability, and cognitive flexibility. The task that showed the most severe impairment, with null performance, was the digit backward span. Mild cognitive impairment was concluded with verbal learning impairment and altered language, especially in oral production, fluency, and repetition, with preservation of comprehension, dysarthria, and no paraphasia, compatible with Broca aphasia, as well as partial alteration of executive functioning, with very low performance in working memory and cognitive flexibility.
In addition, instruments were administered to explore the presence, frequency, and severity of neuropsychiatric and specific symptoms of anxiety and depression, with results of possible moderate depression and mild anxiety (Table 1). The patient showed mild dependence in basic activities of daily living and instrumental activities and no social risk was detected (Table 1).
Regarding the qEEG, the most relevant results were a generalized decreased absolute power, except in the right frontal area, which showed elevated power peaks in the slow and fast frequency waves (Figure 1g) and an average alpha peak frequency shifted at low frequencies (7.23Hz with 0.41 standard deviation), which is considered slow, very high delta relative power, with a generalized decrease in the other frequencies (Figure 1h), high slow-wave to fast-wave ratios (Figure 1i), and very altered synchronization between different brain areas, with marked inter- and intrahemispheric frontal and temporal asymmetries (Figure 1j). Finally, LORETA analysis of extreme deviation values (Figure 1k) showed a marked prefrontal asymmetry signal with excess in the right prefrontal lobe and defect in bilateral parahippocampal gyrus and bilateral posterior cingulate, as well as in left inferior frontal gyrus, left superior temporal gyrus, and left insula.
The conclusion was primary progressive aphasia, a form of frontotemporal dementia, as well as small vessel disease, with mild cognitive impairment. Donepezil 10 mg and escitalopram 15 mg were prescribed. Intervention in neuropsychology and speech therapy began with the aim of preserving unimpaired cognitive skills, providing alternative communication systems and for the management of affective symptomatology.
Discussion
We present a case that started with difficulties in the language area, with a personal history of hypertension, diabetes, and dyslipidemia, which, after study, revealed atrophy and hypometabolism of the left temporal and frontal lobes, with microlesions of vascular origin in bilateral subcortical and periventricular white matter. Neuropsychological assessment showed alterations in executive and language domains, with moderate depressive and mild anxious symptomatology. These findings were complemented with a qEEG to establish associations with neuroimaging and neuropsychology. The qEEG data showed close relationship with the rest of the findings. Frontotemporal atrophy has been previously related to low alpha peak frequencies (around 7.5-8.5) and increased relative slow wave contribution, as well as inter- and intrahemispheric asymmetries (Passant et al., 2005), as shown by the patient under analysis. It has also been described that the increase in frontal and temporal slow wave power correlates with PET images showing hypometabolism in these areas and, in a similar way, the qEEG findings in connectivity parameters correlate with the information provided by DTI imaging studies showing damage in white matter (Koberda, 2021); these findings were also common in our case. Particularly relevant, the patient showed excess right prefrontal power, corroborated by LORETA analysis and marked prefrontal asymmetry. This type of findings have been related to depressive states and also to executive dysfunction (Saletu et al., 2010), again, characteristics presented by the patient. In addition, the progressive increase in power and relative contribution of low frequency waves, as well as the shift of the alpha peak to lower frequencies, has been consistently related in the literature to the progression of cognitive impairment to dementia, being particularly relevant parameters when estimating disease progression (Hamilton et al., 2021). Finally, a decrease in the left temporal and frontal signals stand out, which could be associated to the neuroimaging findings and the marked impairment of expressive language. These relationships, although consistent with the findings of the other tests and with the literature, should not, in our opinion, replace the usual diagnostic procedures, but rather complement them. Therefore, the combined use of neuroimaging, neuropsychological assessment, and qEEG may help clinicians to higher diagnostic specificity and grade severity.
Although qEEG provides a large amount of objective and specific information about a patient’s brain, a given qEEG found may not be pathology-specific and can be found in different conditions limiting its use, requiring, at least, additional neuropsychological assessment (Salcini et al., 2020). Therefore, we consider that qEEG may find its best utility as a tool in the context of neuropsychological assessment, so that the professional can contrast and associate neuropsychological findings with the underlying brain psychophysiology; however, due to its limitations, diagnosis of structural brain alterations will require neuroimaging methods. Moreover, objective, psychophysiological data from qEEG could be useful in the follow-up of patients and the study of the disease progression or the effect of therapies, both pharmacological and non-pharmacological, so that this information could be associated to observed cognitive, emotional, and behavioral changes. In conclusion, qEEG is an accessible technology that, despite limitations, provides objective and useful brain psychophysiological information for neuropsychological practice.