Introduction
the outbreak of COVID-19 posed enormous challenges for healthcare systems around the world. The rapid spread of infection and severity of symptoms increased the number of hospital admissions, resulting in a shortage of structural healthcare resources, mainly associated to workforce and medical supplies. In addition, professionals deployed to new areas lacked of competent skills and appropriate protection equipment. Moreover, there was a shortage of intensive care units (ICU) beds and ventilators, to cover COVID-19 patients’ demands ((1). At patient level, the family contact restrictions during hospitalisation emerged emotional reactions which challenged the recovery process of the whole healthcare system.
Healthcare professionals were concerned about their families and their own safety because of the risk of spreading the infection at home, together with their ability to provide competent medical care(1). These concerns were associated with an increase in the workload, the lack of control of patient’s outcomes due to the absence of effective treatments, the severity of the symptoms, isolation of patients and accumulated losses. All these factors exposed staff to high levels of stress. Anxiety, negative thoughts (guilt, shame, etc.), mood disturbance, increased vigilance and reduced sleep quality prevailed among frontline staff,(2) which was aggravated by the absence of positive reinforcement from social inputs because of isolation due to confinement restrictions(3). The degree that would determine if the healthcare workers’ reactions are transient and adaptive to the events experienced or if they become chronic psychological reactions, would depend on their own resilience. Several modulators for resilience have been described, such as, the nature of distressing experiences, personal vulnerabilities, past experiences, organizational factors related to work climate, and sociocultural factors which may modulate the understanding of events(4).
Several theories and empirically tested concepts in the field of emergency psychology have succeeded in preventing acute and chronic stress reactions and increasing resilience among professionals. Self-efficacy,(5) defined as the perception of one’s cognitive capabilities to influence demands from the context and the neuropsychology approach of the stress response,(6) focuses in cognitive strategies to silent emotionally loaded reactions by the hyperactivity of amygdala have been applied(7).
From a psychodynamic perspective, defence mechanisms play a facilitator role in managing emotional demands and preventing work-related-anxiety among healthcare professionals(8). On the other hand, when emotions have been contained for a prolonged period of time they can be activated through projective techniques when individuals try to find causes and explanations for life events(9). Fantastic Reality(10) is a projective technique, which uses images to transcend the individual into a fantastic reality while feeling in a safe cognitive space. This process can be explained by the neuropsychological mechanism through which images stimulate the visual cortex and the emotional memory simultaneously (when individuals freely associate content to the chosen image) connecting with the prefrontal cortex (when verbalising the perceived images), helping them to narrate traumatic and/or stressful experiences.
In addition, Mindfulness(11) and Cognitive Behavioural Therapies (CBT), such as, stress inoculation, anxiety management and exposure therapy have successfully contributed to facilitate self-regulation and preventing an acute stress disorder(12).
At organizational level, group interventions have proven to be effective in gathering a complete picture of events that individuals have been exposed to and in normalising and sharing emotions among members who have been through the same process. Also, group interventions help cognitive restructuring, by which, individuals acknowledge and understand their experiences, in order to facilitate team cohesiveness, identity, and to repair individual and team confidence(13). In this line, quality improvement tools to increase professionals communication, such as, TALK for clinical debriefing©(14) and the Schwartz rounds® methodology to normalize and share emotions, have been successfully implemented in group format(15). To maximise effectiveness, a multicomponent approach considering group, individual and environmental interventions have been reported to be more effective when managing traumatic stress at the work setting. Also, when psychological support is immediately available on site during a crisis event, these techniques can help to expose individuals to approximate to the pre-crisis psychological balance(16).
When exposed to a rapid and devastating health emergency, the challenge is to find the relevant elements among all the evidence-based knowledge, and combine them in order to provide significant support to the main actors in a real-world context.
In order to prevent chronic maladaptive psychological reactions among hospital healthcare professionals facing first wave of COVID-19, a tailored ad hoc preventive psychological programme named Support Tools for Emergency Psychology (STEP) was developed. This preventive psychological programme was based on the theories mentioned above and implemented in our hospital setting. Our hypothesis was that professionals would value the possibility of accessing psychological support at the time of complex decision-making processes for patient care and workforce re-organization.
The objective of this study was to analyse the STEP programme in order to identify the key elements required to implement a psychological support service for frontline healthcare staff who faced the COVID-19 emergency.
Methodology
the study had a qualitative design, and it was carried out between March andJune 2020 in a public hospital in Girona, Spain, which has a capacity of 337 beds and provides healthcare coverage to 147 000 inhabitants. The workforce of our hospital setting is composed of approximately 733 healthcare professionals and 85 non-healthcare staff(17).
At the peak of the first pandemic wave, the whole hospital required a reorganization to cope with the rapidly increasing demands. Most of hospital beds were allocated to patients with COVID-19 and many healthcare professionals, including the psychologist, were relocated to different areas. A voluntary multidisciplinary frontline team of 8 psychologists was created to provide support to hospital staff, patients and their families. The background of the voluntary psychology team varied from clinical psychology, palliative care, emergency psychology, neurodegenerative disorders and neuro-rehabilitation psychology. This team developed the STEP programme, aimed to provide support to hospital staff. This programme was implemented in areas in which frontline clinical care is provided and included both, individual and group interventions.
Intervention
The STEP intervention programme comprises 3 tools with different objectives, as described below:
STEP 1.0: the objective was to conduct a clinical debriefing to identify and address professionals’ needs or concerns. It was based on “TALK for clinical debriefing ©(14). In addition, it incorporated principles of Mindfulness and the facilitator role of Defence Mechanisms from the psychoanalytic theory. Variables and relevant questions were: 1) concerns and needs, 2) resilience, 3) support required, and 4) learnings (Table 1).
Table 1. STEP 1.0 intervention procedure. STEP programme targeted to staff of a public hospital in Girona, Spain.
| INTRODUCTION |
|---|
| Psychologist introduction Objective of the session: to identify and address professionals’ needs and concerns Rules: 15 minutes duration, confidentiality, non-judgemental, positive thinking, self-efficacy Acknowledgement: to transmit gratitude expressed by the hospital directorate Open questions: “How are you?” “What are your main concerns?” |
| ANALYSIS |
|
- The analysis should end with one key issue to target for improvement - Stress positive thinking - Prioritise feasibility - Prioritise aspects to improve under the control of the group |
| LEARNINGS |
| Summary: professionals are required to list learnings from the session |
| KEY ACTIONS and LEADERSHIP |
| Solutions: Professionals agree on which actions to undertake and who will be leading |
| DECOMPRESSION TECHNIQUES |
| To shake for 40 seconds. To blow candles. Jumping on their toes. Sit on a chair and move head upside down. Tens/loosen all muscles of the body. Relax and breath on 4-2-7 + visual positive stimulus. To identify their own relax thinking style. To remember that someone close to you would tell you to relax. To identify a positive thinking and self-instructions. |
| SELF-CARE TRAINING |
| Psychoeducation: concept of stress Techniques: A) Allow yourself 2 minutes at the beginning of your working-shift to focus. B) Focus on professional aspects of your work: tunnel vision. C) Allow yourself a rest every 2h: send a message to your family, decompress yourself, talk to your colleagues, think about what you will do when you arrive at home. Physical activity helps. D) Avoid talking about the same things for a long time. E) Do not forget hydration during working times. F) Accept that nobody can expect to be euthymic all the time. G) Stop if you are feeling overloaded, search for a private place and decompress. H) Remember that it is not necessary to feel broken to seek psychological support. I) Avoid moaning. J) Think about a ritual to take off the work uniform after the working-shift and understand that work has finished. |
STEP 1.5: the objective was to ventilate emotions while keeping awareness that the outbreak was not finished yet. Specific groups were also created to include only professionals who had been infected by COVID-19 and had already returned to work. This used Schwartz rounds® methodology(15). In addition, it incorporated Fantastic Reality projective techniques(10) using 30 pictures of roads with different features (Figure 1). Variables relevant to this tool were: 1) roads features, 2) emotions, 3) thoughts, 4) resilience, 5) learnings, and 6) whether professionals previous infected with COVID-19 reported differently at the group interventions compared to the rest of their colleagues who were not infected by COVID-19 (Table 2).
Table 2. STEP 1.5 intervention procedure. STEP programme targeted to staff of a public hospital in Girona, Spain.
| INTRODUCTION |
|---|
| Psychologist introduction Objective of the session: To express contained emotions during the outbreak Rules: duration of 30-40 minutes, confidentiality, non-judgemental |
| ROAD PICTURES WHICH BETTER REPRESENTS YOUR WALK THROUGH THE OUTBREAK |
| Pictures of roads with different features are presented to participants with the objective to emerge contained emotions. Professionals are required to pick up one or more of those, the ones which better represent how they felt along the COVID-19 outbreak |
| REASONS FOR CHOOSING THE PICTURES |
| Professionals are required to share their reason for picking up each picture |
| SWAPPING CHAIRS |
| “Now, that you are in this chair, what would you tell your colleague who was sitting where you are now?” |
| LEARNINGS |
| Professionals are requested to verbalise what they have learned along the path they have walked so far with during the outbreak |
| PSYCOEDUCATION OF EMOTIONS |
|
- Concept of contained emotions - Normalisation of emotions - Need for ventilation - Situations where individual therapy can be required |
STEP 2.0: The objective was to increase professionals’ awareness of the physical signs of emotions, and their management during peak working times. It included principles from Mindfulness and projective techniques by using four pictures of emoticons, extracted free from internet, which included happiness, anger, sadness and fear. The variable relevant to this tool was the perception of self-efficacy on managing emotions by analysing the change in scoring when performing the body scan (meditation technique) (Table 3).
Table 3. STEP 2.0 intervention procedure. STEP programme targeted to staff of a public hospital in Girona, Spain.
| INTRODUCTION |
|---|
| Psychologist introduction Objective of the session: increase awareness of physical signs of emotions and how to manage them during peak working times Rules: 30 minutes duration, confidentiality, non-judgemental |
| METHOPHOR |
| We are at a different time in this crisis. It helps to think about a marathon that started weeks ago and we cannot still see where it ends. Now we need to take a break and refuel without stopping to keep on moving and to perform and feel good. What is happening to you is what we expected to happen and what is desirable. It is normal to feel tired and to feel discomfort during this marathon. Despite the fact that it is normal and expected, it does not mean that we have to accept it without doing anything about it. |
| BODY SCAN |
|
1-In a likert scale 0-10, which emoticon better represents how you have felt over last two weeks?. 2- In a likert scale 0-10, which emoticon better represents how you feel at present? (just before the body scan) 3- Guided body scan. Professionals are required to focus their attention on specific areas of the body, top-down named by the psychologist, with a non-judgemental attitude. 4-In a likert scale 0-10, which emoticon better represents how you feel at present? (just after body scan). |
| PSYCHOEDUCATION |
| Professionals choose which emotions were the most predominant and prioritise them for psychoeducation: function of emotion, adaptive and maladaptive signs, and resource bag strategies are provided (based on CBT and mindfulness) |
| CLOSING THE SESSIONS |
| Using the “Marathon metaphor” professionals are encouraged to use those emotional tools presented during the session: “Continuing with the marathon, maybe those minutes have helped you realize that you have a foot injury and that you need some time to heal it and allow yourself a longer break. Or that you need to surround yourself with people who love you and you need to feel their support. Giving encouragement and feeling that they give it to you usually helps! These resources that we have talked about are different components of provisioning. You decide which ones can help you better right now.” “We invite you to use these strategies that we have shared over the next few days and notice if they can help you. We also encourage you to practice these three steps to identify, be aware/recognise, and manage what you notice and feel, at moments like going to work, having a shower, queuing in the store, folding clothes... Stop and listen to your body, it can help you. In order to be able to continue with the marathon, these supplies are needed. * Remember to keep awareness to identify during group sessions those individuals who may need individual sessions. |
Psychologists, had access to COVID-19 protection equipment and free access to all wards including the ICU and emergency care unit. They implemented a hotline, to provide immediate assistance if required, available from 8:00 to 20:00, seven days a week, and a specific contact email address, which was disseminated across all hospital wards and through line managers. Also, outpatients’ offices for individual interventions and team meetings were available to them. Psychologists were distributed in specific hospital wards.. Each ward was checked to detect the need for psychological care and/or support, for both patients and hospital staff. Group interventions were also offered, either directly to hospital staff or through their line managers. There were on average six individuals per group, andthe duration of the intervention ranged from 15 to 40 minutes, depending on the clinical tool implemented. Group interventions were conducted by two psychologists and took place on each ward. Hospital staff who were working together were allocated in the same group intervention.
To reduce variability when carrying out group interventions to professionals, psychologists conducted training sessions during the first hour of each shift (at 8:00am and 3:00pm, respectively depending if it was a morning or a back shift) and those sessions included role-playing and shadowing techniques.
Both, individual and group interventions were always carried out during the staff members’ working hours, and the participation in the psychological interventions was voluntary.
Participants
All hospital staff who attended the STEP programme were included in this study. Different professionals were included in the study, such as, clinical staff (including line managers) working in either frontline (ICU, emergency and recovery wards) or non-frontline roles (preventive services, radiology, pharmacy, laboratory services, outpatients, appointment centre team, patient complaints team), non-healthcare workers (kitchen, cleaning services and hospital hotel services management) and professionals who returned to work after recovering from COVID-19 disease.
Data sources and measurements
Data were collected from three sources between March and June 2020: 1) psychologists’ paper note transcriptions from the STEP programme, 2) anonymous questionnaires completed by participants, and 3) focus group with psychologists as participants.
The following variables were included: 1) Variables targeted by the STEP programme: transcriptions of paper notescollected by psychologists during group interventions were analysed to identify relevant variables targeted by the STEP programme, and a list of questions according to different dimensions were formulated to get relevant information on psychological intervention targets (Table 4); 2) An anonymous ad hoc questionnaire was developed and distributed to clinical staff. Responses were analysed to identify professionals’ preferences to receive psychological care and support. The questionnaire included two questions: i) what were the priority areas that professionals wish to receive psychological support on, and ii) which format did professionals prefer to receive support: group, online, individual, paper materials. Before introducing STEP 1.5, the questionnaire was distributed in envelopes in all wards with the aim to identify what were the professionals’ needs when admissions started to decrease. An additional envelope was provided to return the fulfilled f questionnaires. Enough envelopes were handed out for all shifts, including weekends. The questionnaires were anonymous and voluntary; and 3) A focus group was conducted to collect psychologists’ feedback on defence mechanisms most frequently emerged in STEP 1.0 and on professionals’ characteristics which were associated with the referral process to the individual therapy either for those who dialed the hotline, those who were selected when scanning the wards, and for those who accepted a referral through their line manager.
Table 4. List of variables from paper notes transcriptions collected by psychologists during group interventions. STEP programme targeted to staff of a public hospital in Girona, Spain.
| Variables | Items |
|---|---|
| STEP 1.0 | |
| Concerns and needs | What were the more frequent concerns and needs that arose in STEP 1.0? |
| Resilience | What were the professionals’ resilience responses emerged? |
| Support required | What professional skills were required to improve? |
| Learnings | What were the learnings professionals more often verbalised after STEP 1.0 group intervention? |
| STEP 1.5 | |
| Roads features | What were the road pictures features most frequently selected by professionals to describe how they have felt along the outbreak process? |
| Emotions | What emotions were associated to those features? |
| Thoughts | What thoughts were associated to those features? |
| Resilience | What effective coping strategies emerged as been used along the outbreak? |
| Learnings | What learnings professionals more often verbalised have acquired during STEP 1.5? |
| Professionals infected with COVID-19 | Did professionals who were infected with COVID-19 report differently at the group interventions than the rest of their colleagues who were not? |
| STEP 2.0 | |
| Body Scan |
- In a likert scale 0-10, which emoticon better represents how you have felt over last two weeks. - In a likert scale 0-10, which emoticon better represents how you feel at present (just before the body scan) -In a likert scale 0-10, which emoticon better represents how you feel at present (just after body scan) |
| Questionnaires | |
| What priority areas professionals wished to receive psychological support |
- Emotional (feelings, physical signs of stress, reverberant thinking). - Teamwork communication. - Improve skills to communicate to patients’ families. - Self-care. |
| What format did professionals preferred to receive support |
- Group. - Online. - Individual - Paper materials |
| Psychologists feedback (focus group) | |
| Individual sessions | Professionals’ characteristics associated to professionals referred to individual therapy |
| Defence mechanisms | Defence mechanisms most frequently emerged in STEP 1.0 |
Although an external blinding evaluation of measurements was not possible, data were always evaluated by two independent psychologists.
Ethical approval was obtained from the Girona Ethic Committee for Clinical Research and Medicines (CEIm Girona, Spain, Hospital Universitari de Girona Josep Trueta).
Results
three hundred professionals participated in the study, 100.0% in STEP 1.0 group interventions, 27.3% in STEP 1.5, 2.7% in STEP 2.0 and 10.0% in individual interventions (Table 5). Twenty two professionals out of 110 (20.0%) self-requested for group interventions to be conducted. Line managers or hospital prevention services requested the rest of group interventions. Within STEP 1.0 (concerns, needs and support required), risk of infection and self-confidence on managing patients’ symptoms were the most common concerns at the beginning. Professionals received self-care advice and training on effective communication with patients’ families and with team members, such as, protocols for breaking bad news and for making condolence calls(18). Working in a supportive team was the key factor more often associated with resilience by professionals. . Learning points included to share and normalise concerns, to identify supportive colleagues, and to prioritise demands were the learning points emerged with STEP 1.0Regarding STEP 1.5 variables (road pictures, resilience and learnings), on average, each professional chose to conduct this exercise using one picture. Several characteristics of road pictures facilitated participants’ projection of emotions (Figure 1), and a list of associated thoughts and reported coping strategies was identified, allowing participants to implement and learn from them (Table 6). Pictures facilitated the ventilation of emotions and were associated with thoughts when professionals rememorized the outbreak experience. For instance, fear and rage were associated to isolation when coping with the requirements of new roles. Distress and anxiety were associated with lack of protective equipment. Insecurity and anger were associated with lack of consistency in the information provided to professionals. Emotional lability, hopelessness and sadness were associated with their perception of a lack of validation from managers. Hopelessness and impotence were associated with frustration about deceases.
Table 5. Description of patients admitted to hospital, professionals participating in STEP programme and the interventions conducted along the whole COVID period. STEP programme targeted to staff of a public hospital in Girona, Spain.
| TOTAL | MARCH 2020 | APRIL 2020 | MAY 2020 | JUNE 2020 De-escalation | Individual therapy (whole period) | |
|---|---|---|---|---|---|---|
| Clinical tools | STEP 1.0 | STEP 1.5 | STEP 1.5/2.0 | Individual | ||
| Group sessions n (%) | 110 | 81 (74.0) | 28 (25. 5) | 1 (0.9) | - | |
| Participants n (%) | 300 | 300 (100.0) | 82(27. 3) | 8 (2.7) | 30 (10.0) | |
| COVID-19 patients’ admissions n (%) | 615 | 243 (39.5) | 309 (50.2) | 54 (8. 8) | 9 (1.5) | - |
| Professionals infected n (%) | 115 | 78 (67.8) | 34 (29.6) | 3 (2.6) | 0 | - |
Source: Institut Assistència Sanitaria, Girona, Spain (http://www.ias.cat/)
Table 6. STEP 1.5 - Findings. Responses that pictures evoked in professionals and coping strategies used and personal learnings. STEP programme targeted to staff of a public hospital in Girona, Spain.
| Roads features most preferred | Emotions evoked | Thoughts associated | Effective coping strategies used | Learnings |
|---|---|---|---|---|
| Isolated/empty roads | Isolation, fear, rage | What to say to patients’ families, how to perform in my new professional role |
- Positive self-instructions. - Pay attention to safety measures. - Relaxation when faced with the risk of infection. - Team building, cooperation, the team was protective. Friendship. - Tunnel focus on day by day. - Share and express feelings to line managers - Positive expectations towards future. |
- Self-confidence -Awareness of the skills to cope in front of adversity. - New professional skills - Look after myself |
| City roads | Distress, anxiety | No protection | ||
| Lots of signs pointing toward different positions | Doubtful, insecure, Anger | Chaos, many changes in protocols and professional roles, disinformation, contradictory information | ||
| Lots of turns | ||||
| Intersections | ||||
| Ups and Downs | Emotional lability, hopelessness, sadness, | Not enough validation received from management, not enough support, | ||
| Straight with no ending | Uncertainty, impotence, hopelessness | Frustration by deceases |
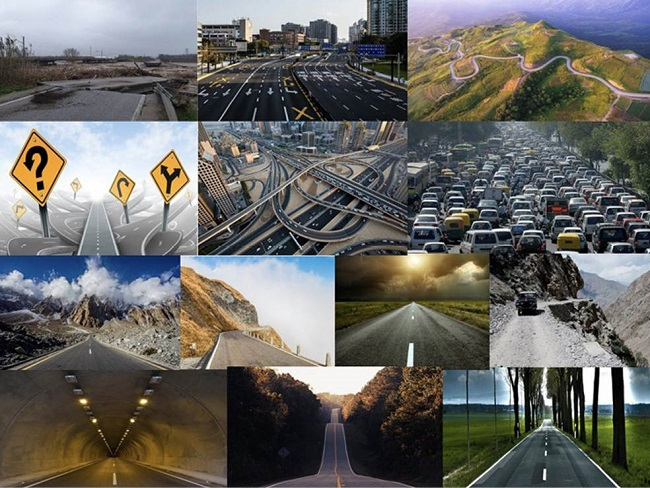
Figure 1: Road Pictures. A sample of the most frequently road pictures* selected by professionals to describe how they perceived their experience during the COVID-19 outbreak. STEP programme targeted to staff of a public hospital in Girona, Spai.
Regarding professionals who suffered COVID-19 infection, emotions and thoughts did not differ from the rest of participants. However, resilience was different, as it was more difficult for them to adapt on their return to work because of the persistence of COVID-19 symptoms, and some reported symptoms of agoraphobia. They acknowledged that the infection process made them aware of the importance of positive thinking skills and stop being self-demanding. They also valued sharing their experience with other colleagues who had been through the same process.
STEP 2.0 variables showed that confronting professionals with a quick body scan was intended to help them to experience the benefit of 5 minutes break to focus their attention on the present circumstances, moment-by-moment, observing without interpreting to achieve self-control. This tool was introduced to just one group who had not been through the STEP 1.5, and the initial benefits were rapidly dismantled by a need to ventilate. No further implementation of this tool was possible, as de-escalation started and STEP programme was interrupted.
A total of 203 professionals (response rate 67.7%) responded to the questionnaire, including doctors, nurses, nursing assistants, admin support, pharmacists, radiologist, social workers and hotel services. Professionals stated that they needed emotional support (71.0%), particularly on feelings (59.0%) rather than thoughts (26.0%). In addition, they preferred group format during working-shifts (61.0%) rather than online workshops after work (9.0%) or paper-based materials (33.0%); 24% preferred individual sessions.
Finally, focus group with psychologists showed professionals’ characteristics associated to individual therapy. Psychologists reported that 30 professionals received individual interventions, 10 (33.3%) of which were requested by professionals’ themselves. The average number of sessions per professional was three. The factors present in those professionals who required individual therapy were caring for dependants, lack of access to childcare, being deployed to a new professional role, communication difficulties among the members of the team, excessive clinical workload, pre-existing anxiety and/or other mental health disorder, grief process due to a deceased in the family, being infected by COVID-19, lack of a social network or living alone. In relation to defence mechanisms emerged at STEP 1.0, psychologists identified that initially, when professionals were high on adrenaline, the most frequently observed defence mechanisms were dissociation and denial of physical signs and emotions associated to stress.
Discussion
this study showed that initially, when demand overloaded capacity, self-protection and self-efficacy, particularly on managing patient families’ demands and improving communication with new team members, appeared to be the main concerns. Subsequently, a request for emotional support, particularly on managing feelings contented, was needed. In addition, working in a supportive team was associated to increased resilience. On the other hand, caring for dependents, a lack of social network, living alone, experiencing a grief process, being infected by COVID-19, pre-existing mental health conditions, and non-adjustments within the team were vulnerabilities for a referral to individual therapy.
The STEP programme helped to identify these needs and to tailor interventions based on sound knowledge on stress management at the workplace during a healthcare emergency. For instance, WHO recommendations focus on the need to normalize strong emotions and stress, to address self-care, social support, clear communication and distribution of tasks and the utilization of psychosocial and psychological help without stigmatization(19). The clinical tool STEP 1.0 provided professionals with self-care guidance, improving team communication and professionals’ self-efficacy to confront patients’ isolation and the requests from families. Self-efficacy1 and self-care(20) have also been reported as major concerns in professionals deployed into new roles. The implementation of STEP 1.0 facilitated the development of targeted educational materials accordingly in order to empower professionals. The clinical tool STEP 1.5 facilitated the emotional healing which literature reports as necessary to achieve adaptive responses after the outbreak(12, 21). It was a professionals’ request the need to ventilate emotions, and the STEP programme facilitated to bring contented emotions to the surface and ventilate while helping to process potentially traumatic experiences at the same time. The group intervention format helped to stress the normalisation of those reactions and contributed to a constructive, rather than traumatic, narrative of the experiences that professionals had been through.
Although, STEP 2.0 could not be implemented widely, as the de-escalation process was initiated, the experience reassured us that interventions were supportive when followed a chronological phases approach with specific needs and concerns required to address. At the beginning of the “Cognitive” phase, infection and self-efficacy were major concerns, and dissociation and denial of stress physical signs were the defence mechanism more active. The “Ventilation” phase was characterised by the expression of contented emotions when it was required, and the “Recovery” phase occurred when the clinical overload decreased and professionals were able to focus on emotions management training. Emotional ventilation was not found to be useful when introduced during the cognitive phase, and training on emotions management should only happen after ventilation. In addition, the implementation of face-to-face psychological support at frontline and during working shifts were the preferences reported by professionals
Our study has strengths and limitations. The fact that an external and blinding evaluation of measurements was not possible and a more elaborated statistical analysis was not conducted may bias the interpretation of our results. However, data were evaluated by two psychologists and training sessions were conducted previously to group interventions to unify criteria. This contributed to reduce variability and potential bias. In addition, professionals’ participation on STEP programme activities was high, we had a large sample including both healthcare and non-health workers, which increased representativeness and external validity, making it more pragmatic and applicable. STEP programme contributed to overcome professionals’ stigma linking psychological support to mental health weakness, therefore rejecting any psychological aid. For instance, interventions based on self-administrated computer-based educational programmes have reported high levels of attrition of about 40%(22).
In conclusion, the STEP programme showed that professionals’ needs and demands changed along with the outbreak overload so interventions had to be tailored accordingly. Future research should analyse the impact of professionals’ resilience in patients’ outcomes and their satisfaction.














