INTRODUCTION
Hypomagnesemia is a rare biochemical alteration in outpatients, however up to 12%1 of hospitalized patients can be detected, being is one of the most commonly underdiagnosed metabolic disorders in patients admitted to Postoperative Intensive Care Units. Hypomagnesemia symptoms usually start with serum concentration below 1.2 mg/dL. Frequently it is associated with the presence of hypocalcemia, hypokalemia, and metabolic alkalosis. Total parenteral and enteral nutrition, diuretics and nephrotoxic drugs, diarrhea and hypoalbuminemia play an important role on its onset. Recently, different authors have described several cases of symptomatic hypomagnesemia associated with the prolonged use of proton pump inhibitors (PPIs)2. A severe magnesium deficiency can trigger life-threatening cardiac and neurological disorders3.
We present a case of acute seizure crisis in women who underwent resection of the small bowel secondary to umbilical hernia. After two months of admission, she presented several switch-off episodes and generalized seizures. Imaging tests did not show structural damage. Laboratory tests highlighted severe hypomagnesemia.
During admission, she had difficult-controlled diarrhea, probably malabsortion related. Despite metabolic and nutritional complication secondary to bowel resection usually appear months after post-surgery, it is rare come across with severe electrolytes disorders due to the reduction of the intestinal absorptive surface during the immediate postoperative period.
CLINICAL REPORT
46-year-old woman with a history of obesity and stage IIa cervical carcinoma operated in 2012, without current cancer treatment, who on 28 July 2019 was admitted to the General Surgery Service due to symptoms of abdominal pain and hemodynamic instability, classified as an acute abdomen.
She underwent emergency surgery for peritonitis secondary to intestinal ischemia in relation to intestinal obstruction due to left paraumbilical internal hernia, as a consequence of previous gynecological surgery. Ileiocecal resection of the ischemic loop and jejunal latero-lateral anastomosis were performed.
The postoperative period was torpid requiring admission in the Critical Care Unit (CCU) for hemodynamic and respiratory support secondary to septic shock
She remained in the CCU two months, during which time she presented multiple infectious complications, including several episodes of ventilator-associated pneumonia, caused by multiple germs (Citrobacter freundii, Klebsiella varicola, Klebsiella pneumoniae, Stenotrophomona maltofilia and Acinetobacter baumanii) receiving multiple antibiotic therapy cycles. In addition, she presented diarrhea in the context of adynamic ileus, related to the prolonged use of opioids, neuromuscular blocking agents, and malabsorption with loss of nutrients as a consequence of jejunal resection. Bacterial origin of diarrhea was ruled out.
Nutritional support was initiated on CCU, initially total parenteral nutrition according with her macronutrients and electrolytes requeriments and then enteral nutrition maintaining an optimal hydroelectrolytic and nutritional status
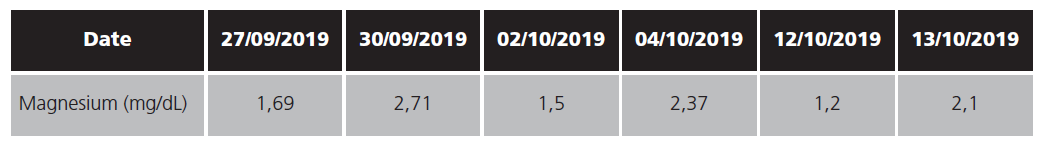
On 28th of September patient was discharge from CCU to general surgery ward, tolerating oral intake and meeting her nutritional requeriments. The same day in the afternoon patients had a generalized tonic-clonic seizure episode, requiring benzodiazepines and readmission to CCU. Head CT scan did not show acute injuries. In the blood tests, severe hypomagnesemia stands out after cessation of intravenous magnesium infusion (table 1). Vitamin D, phosphorus, calcium and sodium plasma levels were normal
Magnesium levels were restored by intravenous magnesium sulphate infusion, with no new seizures. She was discharged again to general surgery ward at 48 hours with magnesium levels in the normal range.
Following days she had watery diarrhea. Clostridium difficile toxine and stool culture were negative. Blood test showed fecal calprotectin elevated in relation with surgery.
On bloods test, magnesium levels showed a progressive decrease probably diarrhea related, prescribing oral supplements.
On October 11th, patient had abdominal pain, poor general health, excessive sweating and hemodynamic instability. Abdominal CT scan was performed showing complete bowel obstruction, requiring urgent surgical treatment. Surgical team found intestinal plastron with adhesive closedloop small bowel obstruction in hepatic flexure and ileum wall ischemia. Wide ileocecal resection and a new latero-lateral anastomosis to right colon were performed.
No incidents were recorded during postoperative evolution until next day (12th October) when patient had an absence seizure episode without other neurological foci. Given the history of hypomagnesemia, 12.5 mEq of magnesium were administered. Patient improved immediately her consciousness level. Electrocardiogram did not show any alteration.
After 24 hour of stability, patient was discharged again to surgical ward with magnesium supplements. On 31th of October patient was discharged home with magnesium oral supplement and she had not any seizure episode.
Karch y Lasagna and Naranjo Adverse Drug Reaction Probability Scale was conducted4-5, obtaining definite as result. In addition, medicines review was performed, including all the medicines prescribed during her admission, ruling out medicines related hypomagnesemia. Medicines may cause magnesium alteration were furosemide6, however this drug started 2 days after of magnesium levels abnormalities. Patient was on omeprazole, which one has been reported as a hypomagnesemia cause1. However scientific evidence shows this side affects after at least one year treatment and our patient only had 15 days on it.
DISCUSSION
Hypomagnesemia has been reported up to 12% of hospitalized patients7. It may go undetected because is not often measured in routine blood tests. Clinical symptoms usually appear with serum levels below 1.2 mg/dL and is usually associated with other electrolytes disturbances as hypocalcaemia and hypokalaemia.
Our patient had serum vitamin D and electrolytes in range and magnesium levels were above 1.2 mg/dL although, they were replenished by intravenous infusion. The required magnesium dose depended on serum levels and clinical symptoms due to sudden onset of symptoms after magnesium infusion discontinuation.
The main problem in our patient was the diahrroea. However there are not reports proposing immediate magnesium deficiency after stop supplement infusion even with diarrhoea controlled as our case.
Our case underlines the importance of continuous monitorization of patient who undergoes intestinal elective surgery and according to new theories, gene screening7. Although this side effect has been reported, evidence has not showed with the immediacy of our case and with different course than expected due to concomitant electrolytes disturbances were not found.
To sum up, magnesium deficiency should be taken into account in patients undergoing elective bowel surgery with a resection greater than 50 centimeters. In addition, this deficiency may occur as single electrolyte disturbance with sudden onset.