INTRODUCTION
Stroke, or cerebrovascular accident, is an important leading cause of death and disability worldwide. Risk factors for stroke are well established and mainly include hypertension, dyslipidemia, cigarette smoking, diabetes, and atrial fibrillation.1,2 In Lebanon, a country of the Middle East, stroke is considered as the second leading cause of death among Lebanese people.3 It had an adjusted prevalence of 0.50% (95%CI, 0.33-0.66) in 2012 and a mortality rate of 62.7/100,000 population in 2011.3,4 Moreover, a recently published cross-sectional study indicated that 12.1% of Lebanese stroke-free people experience stroke symptoms.5 However, Lebanon still scuffles with scarcity of reliable information about this disease.
An increase in the number of stroke events related to food and lifestyle changes has been greatly observed in developing countries.6 Many dietary interventions have been implemented in order to reduce the risk of stroke through managing and treating its risk factors, especially hypertension, obesity, dyslipidemia, and diabetes.6 The Mediterranean diet (MeD) is considered to be among the world's healthiest diets and associated with encouraging health outcome and improved quality of life.7 There are many forms of the MeD, yet, this diet is known to be rich in beneficial oils such as olive and canola oil, whole grains, legumes, fruits, and vegetables. A Mediterranean dietary pattern has been found to be associated with lower risks of metabolic syndrome, cardiovascular diseases, and stroke.8,9 Many recently published systematic reviews and meta-analyses emphasized on the association between adherence to the MeD and stroke. The MeD has a protective role against stroke with a relative risk RR ranging between 0.64 (95% CI 0.48-0.88) and 0.90 (95%CI 0.87-0.93).10 Additionally, high adherence to the MeD has a RR of 0.73 (95% CI 0.59-0.91) for unspecified stroke and 0.82 (95% CI 0.73-0.92) for ischemic stroke.9
The Lebanese diet is a highly traditional cuisine. Yet, this diet is comparable to many northern Mediterranean countries. It relies mainly on vegetarian recipes with great profusion of fruits, vegetables, legumes, cereals, and nuts, in addition to olive oil as the main fat used.11 The traditional Lebanese food and dietary habits which contributed to weight control have been highly influenced by the Western during the last two generations with great changes in ingredients and percentages of macronutrients contribution to this diet.11,12 The Lebanese diet has shifted to increasing its fat, milk, and animal protein intake and decreasing the consumption of cereals and whole wheat, hence, growing the risk of non-communicable diseases.13 It has lately shown that it includes more than the 30% limit of fat recommended by the World Health Organization (mainly saturated), and that the carbohydrates and proteins are at lower limit of the recommended intake.14 Although the Lebanese diet attempted to modernize and develop its cuisine, this diet retained many of its Mediterranean characteristics and tried to strongly adhere to culture and tradition.11 In Lebanon, the MeD was found to be negatively associated with waist circumference (p<0.05) and to reduce the risk of metabolic syndrome with OR 0.53 (95%CI 0.3-0.94) and stroke-like symptoms in stroke-free population, adjusted OR 0.87 (95%CI 0.76-0.99).5,8,15 This study aims to evaluate the relationship between diet and stroke by assessing the adherence to the MeD and the risk of stroke in the Lebanese population based on the version of the MeD published by Martínez-González and colleagues.16
METHODS
This is a hospital based case-control study with prospective data collection. It was conducted at five tertiary hospitals (private and governmental) in Lebanon between January 1st, 2015 and December 31st, 2016. The Faculty of Pharmacy at the Lebanese University, Hadath, Lebanon waived the approval of this study since it was observational with no traceability of patients.
Data were collected using a standardized questionnaire written in English and administered in Arabic language. Data regarding diagnosis, laboratory tests, medication, and medical history were collected from patients' files at the hospitals. All other data, including socio-economic and demographic factors, smoking, physical activities, and diets (MeD) were collected from patients' interviews. A public health professional working on this study collected all data and conducted the interview. Patients were approached during their stay at the hospital and an oral consent was obtained from all patients prior to the interview.
Criteria for inclusion included being Lebanese and 18 years of age or older. Cases have to be admitted to hospitals during the study period with stroke or Transient Ischemic Stroke (TIA) diagnosis based on a Computed Tomography (CT), Magnetic Resonance Imaging (MRI) or both. Control patients were hospitalized patients (during the study period) with diagnosis unrelated to stroke or TIA. Controls were chosen from many wards including infectious diseases, cancer, endocrinology diseases, respiratory diseases, kidney diseases, and digestive diseases as well as injuries and orthopaedic surgeries.
There is no study published in Lebanon reporting the prevalence of the adherence to the Mediterranean diet. However, two recently published studies in Lebanon found that around 64.2% and 70.2% of participants had a moderate to high adherence to MeD.15,17 Therefore, we assumed a prevalence of 70% adherence to the Mediterranean diet in Lebanon. Moreover, high adherence to the Mediterranean diet was found to reduce the risk of stroke in a systematic review with a RR raging between 0.64 to 0.90.10 Therefore, we also assumed an OR of 0.64. We set the two-sided confidence level at 95% and the power at 80%, and considered two controls for each stroke case. A total of 252 cases and 504 controls was required for this study.
The outcome of interest was stroke or TIA. Stroke is defined by the World Health Organization as “rapidly developing clinical signs of focal (or global) disturbance of cerebral function, with symptoms lasting 24 hours or longer or leading to death, with no apparent cause other than vascular origin”.18 Patients were classified as “Stroke Patients” or “Stroke-Free Patients”, the dependent variable, based on the assessment and diagnosis of physicians in patients' files, confirmed with CT and/or MRI.
The independent variable was adherence to the MeD where patients had to answer 14 questions. Each question from the MeD original version was given 1 point based on specific criteria (Table 1). Adherence to the MeD was assessed on the total number of points (score) a patient can have, varying from 0 to 14 points. We divided the total MeD sample score into quartiles. A MeD score within the first quartile was considered as low adherence to MeD and a score within the fourth quartile was considered as high adherence to MeD.
Table 1. Criteria for 1 point in the Mediterranean diet
| Mediterranean Diet 14 questions | Patients' answers | Criteria for 1 point |
|---|---|---|
| A. Do you use olive oil as main culinary fat? | Yes / No | Yes |
| B. How much olive oil do you consume in a given day (including oil used for frying, salads, out-of-house meals, etc.)? | Tbsp. | ≥ 4 Tbsp. |
| C. How many vegetable servings do you consume per day? (1 serving: 200g [consider side dishes as half a serving]) | serving | ≥ 1 serving |
| D. How many fruit units (including natural fruit juices) do you consume per day? | units | ≥ 3 units |
| E. How many servings of red meat, hamburger, or meat products (ham, sausage, etc.) do you consume per day? (1 serving: 100-150g) | serving | < 1 serving |
| F. How many servings of butter, margarine, or cream do you consume per day? (1 serving: 12g or a bit more than ¾ of a tablespoon) | serving | < 1 serving |
| G. How many sweet or carbonated beverages do you drink per day? | serving | < 1 serving |
| H. How much wine do you drink per week? | Glasses | ≥ 7 glasses |
| I. How many servings of legumes do you consume per week? (1 serving: 150g). | serving | ≥ 3 servings |
| J. How many servings of fish or shellfish do you consume per week? (1 serving: 100-150g of fish or 4-5 units or 200 g of shellfish) | serving | ≥ 3 servings |
| K. How many times per week do you consume commercial sweets or pastries (not homemade), such as cakes, cookies, biscuits, or custard? | times | < 3 times |
| L. How many servings of nuts (including peanuts) do you consume per week? (1 serving: 30g or a small handful) | servings | ≥ 3 servings |
| M. Do you preferentially consume chicken, turkey, or rabbit meat instead of veal pork, hamburger, or sausage? | Yes / No | Yes |
| N. How many times per week do you consume vegetables, pasta, rice, or other dishes seasoned with sofrito (sauce made with tomato and onion, leek, or garlic and simmered with olive oil)? | times | ≥ 2 times |
Data were analysed using SPSS version 24. Continuous variables were presented as means with standard deviation and categorical variables as percentages. Chi-squared test and sample t test analyzed the differences between baseline characteristics between stroke and stroke-free patients. A stepwise ascending logistic regression was conducted to limit the potential of confounding. Only variables with p<0.2 in the bivariate analysis were included in the multivariate analysis. The strength of association between the dependent variable and independent variable was expressed in odds ratio (OR) through 95% confidence interval. p-value <0.05 determined statistical significance.
RESULTS
In total, only 217 stroke cases and 445 hospitalized stroke-free patients were primarily involved in this study during the study period. All approached participants accepted to be included in the study after explaining the purpose of this study and assuring anonymity and confidentiality. Twelve stroke patients lacked CT scan or MRI in their files and therefore were excluded from the study. Among the included 205 stroke cases, 69.8% had ischemic stroke, 15.1% had hemorrhagic stroke and 15.1% had transient ischemic attack. Among the total 650 included patients, 1.3% of controls had a history of stroke compared to 34.6% of cases.
This study mainly represented Lebanese people living in Beirut and Mount Lebanon governorates (81.8% of the study population). A one-way ANOVA test has been conducted to check for any differences between hospitals included and the variances between hospitals were not statistically significant from each other (p=0.135).
The mean age of stroke was 70 (SD 12) years. The majority of stroke patients were female (55.1%), living with family (88.3%), unemployed (62.9%), married (64.9%), medically insured (59%), and had a lower education level (85.4%). There was a statistically significant difference between stroke and stroke-free patients concerning age (over 65 years), education status, and marital status. Differences between stroke and stroke-free patients in regard to monthly income were also important (p=0.05) (Table 2).
Table 2. Socio-economic and demographic characteristics of the study's participants
| Variables | Total (N=650) | Stroke Patients (N=205) | Stroke-free Patients (N=445) | P value |
|---|---|---|---|---|
| Age in years; mean (SD) | 63.3 (16.5) | 69.6 (12.01) | 60.4 (17.4) | <0.001 |
| Age group; N(%) | <0.001 | |||
| 18-44 | 96 (14.8) | 6 (2.9) | 90 (20.2) | |
| 45-49 | 34 (5.2) | 6 (2.9) | 28 (6.3) | |
| 50-54 | 56 (8.6) | 13 (6.3) | 43 (9.7) | |
| 55-59 | 42 (6.5) | 11 (5.4) | 31 (7.0) | |
| 60-64 | 45 (6.9) | 14 (6.8) | 31 (7.0) | |
| 65-69 | 102 (15.7) | 45 (22.0) | 57 (12.8) | |
| 70-74 | 79 (12.2) | 37 (18.0) | 42 (9.4) | |
| 75-79 | 93 (14.3) | 32 (12.2) | 61 (13.7) | |
| 80-84 | 74 (11.4) | 25 (12.2) | 49 (11.0) | |
| Over 85 | 29 (4.5) | 16 (7.8) | 13 (2.9) | |
| Gender; N(%) | 0.169 | |||
| Male | 265 (40.8) | 92 (44.9) | 173 (38.9) | |
| Female | 385 (59.2) | 113 (55.1) | 272 (61.1) | |
| Living status; N(%) | 0.096 | |||
| Alone | 55 (8.5) | 23 (11.3) | 32 (7.2) | |
| With family | 595 (91.5) | 181 (88.7) | 413 (92.8) | |
| Employment status; N(%) | 0.674 | |||
| Unemployed | 413 (63.6) | 130 (63.2) | 284 (63.7) | |
| Retired | 89 (13.6) | 31 (15.2) | 57 (12.8) | |
| Employed | 148 (22.8) | 44 (21.6) | 104 (23.4) | |
| Education status; N(%) | 0.001 | |||
| Low education | 498 (76.7) | 175 (85.4) | 323 (72.7) | |
| Intermediate | 85 (13.0) | 21 (10.2) | 64 (14.2) | |
| Secondary | 11 (1.7) | 3 (1.5) | 8 (1.8) | |
| Higher education | 56 (8.6) | 6 (2.9) | 50 (11.3) | |
| Marital status; N(%) | 0.002 | |||
| Single | 39 (6.0) | 6 (2.9) | 33 (7.4) | |
| Married | 451 (69.4) | 133 (64.9) | 318 (71.5) | |
| Widowed/Divorced | 160 (24.6) | 66 (32.2) | 94 (21.1) | |
| Monthly income; N(%) | 0.050 | |||
| <500,000 LBP | 359 (56.4) | 129 (64.5) | 230 (52.8) | |
| 500,000 – 1,000,000 LBP | 207 (32.5) | 54 (27.0) | 153 (35.1) | |
| 1,000,000 – 2,000,000 LBP | 65 (10.2) | 16 (8.0) | 49 (11.2) | |
| > 2,000,000 LBP | 5 (0.8) | 1 (0.5) | 4 (0.9) | |
| Medical insurance; N(%) | 0.489 | |||
| Insured | 397 (61.1) | 121 (59.0) | 276 (62.0) | |
| Uninsured | 253 (38.9) | 84 (41) | 169 (38.0) |
Stroke patients statistically differed from stroke-free patients in respect to medications, body mass index and medical history including hypertension, cardiac arrhythmia, coronary heart disease/myocardial infarction, peripheral artery disease, heart failure, deep venous thrombosis/pulmonary embolism, diabetes, dyslipidemia, previous TIA/stroke, and family history of stroke and heart diseases as well as physical activity, cigarette and waterpipe smoking. Those patients also showed significantly higher values of blood pressure than stroke-free patients (Table 3).
Table 3. Medical and health characteristics of patients
| Variables | Total (N=650) | Stroke Patients (N=205) | Stroke-free Patients (N=445) | P value |
|---|---|---|---|---|
| Body mass index in Kg/m2; mean (SD) | 26.5 (5.1) | 27.2 (5.4) | 26.2 (4.9) | 0.016 |
| Medication History; N(%) | ||||
| Antihypertensive | 274 (42.2) | 140 (68.3) | 134 (30.1) | <0.001 |
| Lipid lowering medication | 153 (23.5) | 70 (34.1) | 83 (18.7) | <0.001 |
| Anti-diabetes | 174 (26.8) | 72 (35.1) | 102 (22.9) | 0.002 |
| Antidepressant | 86 (13.2) | 36 (17.6) | 50 (11.2) | 0.034 |
| Anticoagulant | 47 (7.2) | 29 (14.1) | 18 (4.0) | <0.001 |
| Aspirin | 210 (32.3) | 99 (48.3) | 111 (24.9) | <0.001 |
| Clopidogrel | 60 (9.2) | 29 (14.1) | 31 (7.0) | 0.005 |
| Medical History; N(%) | ||||
| Hypertension | 278 (42.8) | 152 (74.1) | 126 (28.3) | <0.001 |
| Diabetes Mellitus | 172 (26.5) | 75 (36.6) | 97 (21.8) | <0.001 |
| Dyslipidemia | 137 (21.1) | 62 (30.2) | 75 (16.9) | <0.001 |
| Cardiac Arrhythmia/Atrial Fibrillation | 93 (14.3) | 57 (27.8) | 36 (8.1) | <0.001 |
| Coronary Heart Disease/Myocardial Infarction | 128 (16.2) | 87 (42.4) | 41 (9.2) | <0.001 |
| Peripheral Artery Disease | 24 (3.7) | 17 (8.3) | 7 (1.6) | <0.001 |
| Heart Failure | 65 (10.0) | 35 (17.1) | 30 (6.7) | <0.001 |
| Deep Venous Thrombosis/Pulmonary Embolism | 41 (6.3) | 25 (12.2) | 16 (3.6) | <0.001 |
| Obesity | 144 (22.2) | 53 (25.9) | 91 (20.4) | 0.128 |
| Previous TIA/stroke | 77 (11.8) | 71 (34.6) | 6 (1.3) | <0.001 |
| Physically active | 251 (38.6) | 58 (28.3) | 193 (43.4) | <0.001 |
| Cigarette smoking status; N(%) | <0.001 | |||
| Non-smokers | 410 (63.1) | 106 (51.7) | 304 (68.3) | |
| Current smokers | 194 (29.8) | 83 (40.5) | 111 (24.9) | |
| Previous smokers | 46 (7.1) | 16 (7.8) | 30 (6.7) | |
| Waterpipe smoking status; N(%) | 0.001 | |||
| Non-smokers | 584 (89.8) | 172 (83.9) | 412 (92.6) | |
| Current smokers | 47 (7.2) | 21 (10.2) | 26 (5.8) | |
| Previous smokers | 19 (2.9) | 12 (5.9) | 7 (1.6) | |
| Family history of stroke; N(%) | 108 (16.6) | 72 (35.1) | 36 (8.1) | <0.001 |
| Family history of cardiac disease; N(%) | 214 (32.9) | 90 (43.9) | 124 (27.9) | <0.001 |
| Blood pressure classification on admission; N(%)19 | <0.001 | |||
| Grade 1 | 95 (14.6) | 62 (30.2) | 33 (7.4) | |
| Grade 2 | 39 (6.0) | 34 (16.6) | 5 (1.1) | |
| Grade 3 | 24 (3.7) | 22 (10.7) | 2 (0.4) |
In the total study sample, the MeD had a minimum of 2 and a maximum of 11 points among included patients with a median of 7 points. Stroke patients had a lower MeD median compared to controls (6 vs. 8 points); similar findings were for female compared to male patients (7 vs 8 points).
The MeD was divided using quartiles [Quartile 1: score≤6 points; Quartile 2: score=7; Quartile 3: score=8; Quartile 4: score≥9 points). Low adherence to MeD was considered based on a score ≤ 6 points and high adherence to MeD was considered based on a score 9 points or more. Around 29.5% of the total sample had a score within the first quartile, where 52.3% of them had a stroke; 22% of total patients had a score within the second quartile with 23.1% of them presenting a stroke; 24.5% of total subjects scored within the third quartile where 17.6% were admitted to hospitals for stroke diagnosis; and 24% of all included subjects scored within the last quartile and 7% of them presented to the hospitals for stroke diagnosis (p<0.001).
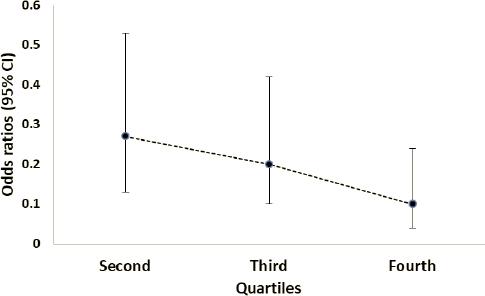
Adherence to MeD was associated with lower likelihood of incident stroke in the second, third, and fourth quartile compared to the first quartile (low adherence to MeD) after adjusting for all potential confounders. The higher the adherence to MeD, the lower the risk of stroke (Table 4 and Figure 1). High adherence to MeD was associated with a decreased risk of stroke, OR 0.1 (95%CI, 0.04-0.24; p<0.001) (Table 4). However, this association depended also on the presence of other stroke risk factors including hypertension history, history of overweight and obesity, being physically active, history of TIA/stroke, and family history of TIA/stroke (Table 4).
Table 4. Association of adherence to Mediterranean diet with risk of stroke
| Variable | Crude OR (95% CI) | Adjusted OR (95% CI) |
|---|---|---|
| First quartile (MeD score ≤ 6 points): Low adherence to MeD | 1.00 | 1.00 |
| Second quartile (MeD score = 7 points) | 0.16 (0.05-0.49)* | 0.27 (0.13-0.53)* |
| Third quartile (MeD score = 8 points) | 0.15 (0.05-0.44)* | 0.20 (0.1-0.42))* |
| Fourth quartile (MeD score ≥ 9 points): High adherence to MeD | 0.08 (0.02-0.26)* | 0.1 (0.04-0.24)* |
| Age | 3.13 (0.0-8.3) | 1.02 (0.99-1.04) |
| Gender | 0.40 (1.15-1.08) | 0.55 (0.3-1.01) |
| Living status | 0.40 (0.09-1.78) | 0.77 (0.32-1.86) |
| Education status | 2.49 (0.62-10.03) | 1.01 (0.73-1.38) |
| Marital status | 1.53 (0.11-20.57) | 1.01 (0.57-1.77) |
| Monthly income | 0.51 (0.14-1.91) | 0.83 (0.63-1.1) |
| Using antihypertensive medication | 0.07 (0.02-0.71)* | 0.2 (0.04-1.01) |
| Using lipid lowering medication | 2.85 (0.62-13.05) | 1.4 (0.56-3.51) |
| Using anti-diabetic medication | 2.26 (0.31-16.44) | 1.05 (0.3-3.66) |
| Using antidepressant medication | 0.97 (0.30-3.08) | 1.07 (0.5-2.28) |
| Using anticoagulant medication | 1.92 (0.43-8.66) | 0.94 (0.34-2.96) |
| Using aspirin medication | 0.76 (0.28-2.02) | 0.73 (0.39-1.38) |
| Using clopidogrel medication | 0.68 (0.15-3.08) | 0.74 (0.28-1.99) |
| Hypertension history | 101.5 (5.1-2001.2)* | 8.4 (1.8-38.8)* |
| Diabetes mellitus history | 0.32 (0.04-2.54) | 0.84 (0.24-2.95) |
| Dyslipidemia history | 0.17 (0.03-0.85)* | 0.53 (0.21-1.33) |
| Cardiac arrhythmia/Atrial fibrillation history | 1.77 (0.50-6.24) | 1.18 (0.55-2.5) |
| Coronary heart disease/Myocardial infarction history | 4.02 (1.23-13.16) | 3.22 (0.99-6.9) |
| Peripheral artery disease history | 0.5 (0.03-8.8) | 0.39 (0.78-1.98) |
| Heart failure history | 0.79 (0.17-3.75) | 0.36 (1.13-1.0) |
| Deep venous thrombosis/Pulmonary embolism history | 10.77 (1.7-68.61)* | 4.38 (1.0-15.07) |
| Overweight and obesity history | 0.02 (0.002-0.21)* | 2.53 (1.56-4.08)* |
| TIA/stroke history | 515.1 (64.4-4119.5)* | 67.82 (20.62-223.1)* |
| Being physically active | 1.08 (0.44-2.7)* | 0.52 (0.29-0.91)* |
| Cigarette smoking | 3.74 (1.39-10.08)* | 1.31 (0.83-2.07) |
| Water pipe smoking | 0.53 (0.06-4.83) | 1.93 (1.0-3.55) |
| Family history of TIA/stroke | 23.11 (6.84-78.12)* | 5.56 (2.82-10.95)* |
| Family history of cardiac disease | 0.67 (0.27-1.7) | 1.08 (0.59-1.97) |
MeD, Mediterranean diet; OR, odds ratio; CI, confidence interval;
*, statistically significant
DISCUSSION
This study shows a significant association between high adherence to MeD and lower risk of total stroke. This study also demonstrates a dose-effect relationship between Mediterranean diet and stroke, which further confirms the association and suggests causality; the higher the adherence to MeD, the lower the risk of stroke.
The findings of this study were in occurrence with the findings of many recently published systematic reviews and meta-analysis emphasizing on the protective role of the adherence to the MeD against stroke.9,10 Another systematic review and meta-analysis comparing many dietary patterns also concluded that the MeD was among the healthy diets to be associated with a reduced risk of stroke.20 In Lebanon, this is the first study to report such an association between adherence to the MeD and stroke. Only one recent data reported that adherence to MeD was associated with reduced stroke-like symptoms among stroke-free population.5
Several studies have supported the favorable effects of the MeD. This diet was found to reduce waist circumference, plasma glucose, total and plasma LDL cholesterol levels and triglyceride.21 Many studies have concentrated their research on this diet and showed that high adherence to MeD is associated with increased chance of longer survival and reduced risk of cardiovascular disease, stroke, cancer, Parkinson's and Alzheimer's disease.22,23 MeD was also found to be inversely associated with risk of the composite outcome of ischemic stroke, where a greater adherence to this diet was associated with significant reduction in overall mortality.20,22,23
The association between high adherence to MeD and reduced risk of stroke may be the consequences of the association of high adherence to MeD and a decrease in stroke risk factors, including hypertension, diabetes, LDL cholesterol, triglyceride, and obesity. The MeD is a dietary pattern characterized by decreased intake of fat, red meat, and dairy products and increased consumption of plants (fruits, vegetables, and whole grains) and olive oil. The MeD diet has been mistakenly considered as a low-fat diet with high carbohydrate intake resulting in increases in diabetes and obesity. However, this diet has high fat content (35% of calories from fat mainly from olive and canola oil and nuts) and emphasizes on whole grains and therefore is considered as a low glycaemic diet.21 The MeD has some beneficial metabolic effects suggesting that this diet might be individualized according to personal preferences and metabolic considerations for weight loss and dietary interventions.24 This diet proved that it is the best diet among diabetic patients in regard to fasting glucose and fasting insulin levels as well as insulin resistance.24
Based on the results of this study, we encourage the public health sector to establish some campaigns and programs to encourage adherence to the MeD since this diet has proved to significantly reduce the risk of stroke. The MeD can be obtained at an affordable cost since its main ingredients are simple and easily available.7 In addition, according to a systematic review investigating the cost and cost-effectiveness of the MeD, this diet is found to be highly cost-effective with a protective role against mortality and morbidity resulting from progressive pathologies. The MeD modifies the outcomes of certain diseases and the costs of their management with gain in life years and quality-adjusted life years.7
Adherence to the MeD is independently associated with the risk of stroke after adjustment for all confounding factors. However, hypertension, overweight and obesity, previous TIA/Stroke, physical activity, and family history of TIA/stroke accounted for some of the association between adherence to MeD and the risk of stroke. In addition to the limited adherence to the MeD diet found in this study among stroke patients compared to stroke-free patients, stroke patients were more hypertensive, less physically active, and more tobacco smokers (cigarette and waterpipe) and had a higher body mass index and higher rates of cardiovascular diseases. Although waterpipe smoking and cardiac diseases (coronary heart disease / myocardial infarction) did not reach statistical significance, their p-value was 0.049, we believe that they were close to be significant with an increased number of subjects included. Having good lifestyle choices is very critical for the prevention of many diseases including stroke. Lebanese people diet has largely shifted in the last few decades. This is alarming because based on evidence from many epidemiological studies including this study, adherence to MeD reduces the risk of stroke among Lebanese patients along with control with other stroke risk factors.
The strengths of this study include the collection of data prospectively, inclusion of five different tertiary hospitals from different Lebanese governorates, diagnosis of stroke based on CT scan or MRI, and control of all common types of potential biases in case-control studies including selection, recall, and observer's bias. The limitations of this study include the representation of Lebanese people mainly from Beirut and Mount Lebanon and reliability of this questionnaire on patients' answers in regard to MeD which may have resulted in a classification bias because some patients might have provided socially desirable responses. Moreover, although the questionnaire explored patients' diet and habits, it did not deal with the period the patients' have been following this diet.
An increased analysis would be of interest to assess the relationship between high adherence to MeD and plasma levels of glucose and lipids as well as obesity in the Lebanese population. This study did not reach the required sample size because it was limited to a specific period for data collection. A larger observational study would be needed in future research to evaluate adherence to MeD and the risk of stroke by subtype and assess whether MeD is beneficial for all Lebanese individuals since we only assessed this diet based on patients admitted to hospitals.