INTRODUCTION
It has been just over a year since the first cases of the Coronavirus SARS-CoV-2, leading to the disease COVID-19, have been identified. Over this period, much has changed in terms of knowledge about the virus and its management. It has, indeed, been a steep learning curve for all involved.1 While physical distancing and other preventive measures have become an integral part of daily life for most, the hope for recovery from this pandemic focuses on widespread vaccination against COVID-19. This paper comes at a time when a number of vaccines that have been deemed to be safe and effective by international medicines regulatory bodies are available and vaccine roll out is underway in several countries, although challenges in assessing the efficacy of candidate SARS-CoV-2 vaccines still exist.2-4 It is also a time when virus variants have been identified and are causing significant concern. While vaccines are available, there are issues with the supply chain and the world is dealing with an exceedingly high rate of infection and death.5-7 This has been described as the pandemic paradox by the WHO regional Director for Europe, Dr Hans Kluge.8 Significant challenges are additionally related to vaccine equity, with low and middle income countries struggling to engage in effective vaccination programmes. The World Health Organisation (WHO) has been working hard to address this issue - and a recent study commissioned by the Foundation of the International Chamber of Commerce (ICC), clearly demonstrates that unless there is global access to the vaccine, this would result in not only a moral failure but also an international economic failure.9,10
Once an effective population programme is in place, it is essential for vaccine uptake by the population to be as high as possible to enable the attainment of herd immunity.11,12 A possible barrier to this could be vaccine hesitancy, which has been defined as ''delay in acceptance or refusal of vaccination despite availability of vaccination service. It is complex and context specific, varying across time, place, and vaccines. It is influenced by factors such as complacency, convenience, and confidence''.9,13 Vaccine hesitancy was identified as one of the ten global health threats of 2019.14 A significant factor fuelling vaccine hesitancy in the present pandemic is the current misinfodemic, with social media facilitating the spread of misinformation.15 One paper suggested that identifying and correcting information on social media platforms, while important, was not having the desired effect.16 Through the use of infodemiology, defined as 'the science of distribution and determinants of information in an electronic medium, specifically the Internet, or in a population, with the ultimate aim to inform public health and public policy', WHO has created an infodemiology strategy for the world with the aim of flattening the misinfodemic curve.17,18 Trained infodemiology managers, through a specifically developed social media tool, monitor trends, correct misinformation and disseminate evidence-based information on various media channels, online and offline.19
The Theory of Planned Behaviour suggests that, whether or not a person will comply with a particular behaviour, in this case taking the COVID-19 vaccine, depends on three major factors.20 These factors being: i) the person's attitudes towards the vaccination in general and the COVID-19 vaccine in particular; ii) the attitudes of 'significant others' about the vaccine; iii) the perceived behavioural control which refers to the perceived difficulty in performing the behaviour, that is, taking the vaccine.
All these three factors are influenced by the social representations people have of vaccines. These representations are created and changed by social media. Social media are major determinants of attitudes and behaviour. Moreover, it is well established that attitudes are not directly correlated with behaviour. While individuals may have a positive attitude towards something, they will not necessarily behave in a manner which is consistent with that attitude.21-23 Research by Fishbein and Ajzen based on Theory of Reasoned Action found that attitudes of significant others in a person's life have an important effect on whether people comply with performing a particular behaviour.24 Therefore, positive health behaviour can be enhanced, if those who are important in a person's life encourage them to do so. Further studies showed that compliance with a health behaviour was predicted even better if self-efficacy and perceived control were considered together with attitudes and subjective norms.25,26 In circumstances when people believe that a particular health-related behaviour can bring about a change in their lives and when they believe that they have control over whether or not to perform this behaviour, the likelihood that the person performs this behaviour increases.
Two consecutive studies, informed by the theories outlined above, were conducted. The primary aim of Study 1 was to explore the attitudes, and factors influencing these attitudes, towards the COVID-19 vaccine amongst people living in Malta while Study 2 aimed to identify the reasons as to why individuals were unsure or unwilling to take the vaccine.
METHODS
Study design
In terms of Study 1 a cross-sectional web-based study design was employed to gather data about attitudes and behaviour towards the COVID 19 vaccine. The anonymous questionnaire was disseminated through the most common social media platforms such as Facebook, Messenger, and WhatsApp. Respondents were encouraged to share as widely as possible on their own social media apps. Inclusion criteria were that respondents resided in Malta and were over 16 years of age.
The same methodology was employed for Study 2, however this was open to an international population not just individuals residing in Malta.
In both studies, the researchers identified themselves as being affiliated with the University of Malta and respondents were informed that the questionnaire was anonymous, voluntary and that it was very short, taking up only very few minutes of their time. The questionnaires were initially designed in the English language and then translated to the Maltese language by a translation expert. The Maltese version was back translated and verified as being correct in both languages. The questionnaire was designed to have the English version of the question, followed by the Maltese version. This design, based on the Skopos Theory, has been found to be the most appropriate, since the Maltese people tend to code switch between the Maltese and English language.27 The studies utilized google forms to gather the data. Prior to initiating the studies, the questionnaires were pilot tested with individuals from different backgrounds using a variety of devices.
In Study 1, data was collected using a questionnaire made up of 17 questions. It was structured as follows: Demographics: Gender, age, marital status, educational level, country of residence, whether respondents where health workers, suffered from chronic disease and whether they took the influenza vaccine the previous year. While the questionnaire was clearly addressed to people residing it Malta, it was possible that people residing in other countries would still answer it. The question asking respondents to indicate their country of residence was inserted to address this issue. Any responses from individuals indicating their country of residence was not Malta were discarded.
Questions to determine attitudes towards COVID-19, about the vaccine, vaccine hesitancy and factors that could influence these attitudes were loosely based on the Theory of Planned Behaviour.20 These included whether participants engaged in preventive behaviour, whether they believed that COVID-19 vaccine will help protect the health of the people who get it; whether the opinion of family and friends was important in their decision to take the vaccine; whether they valued the advice of health professionals regarding the effectiveness of the COVID-19 vaccine; how much they believed that they know about COVID-19 and how much news and information they had seen and heard about COVID-19. The responses were measured on a Likert scale with 1 being strongly disagree/not at all and 10 being strongly agree/very much.
The intention regarding participants' willingness to accept the COVID -19 vaccine and whether they demonstrated vaccine hesitancy was explored using Likert scales and binary questions. These included: whether they intended to take the COVID-19 vaccine when it became available (1 being definitely no and 10 being definitely yes); whether they were willing to give COVID-19 vaccine to their children and whether they would encourage their elderly parents to take the COVID-19 vaccine. In the latter two questions the responses were categorical: Yes/No/Unsure/Not applicable.
For Study 2 basic demographics of gender, age, educational level and country of residence were collected. Respondents were asked whether they intended to take COVID-19 vaccine when it becomes available with possible responses being yes, no, unsure. Those that answered no or unsure where invited to give reasons for their choice, either select from a predetermined set of responses and/or list their own reasons. Respondents were free to choose any number of reasons.
Data for Study 1 was gathered between 30/10/2020 and 16/11/2020 and data for Study 2 was gathered between 26/10/2020 and 26/11/2020.
Statistical approach
Data was analysed using the statistical package R.28 Descriptive statistics were generated to provide a demographic profile of respondents. Mean/median scores and quartiles were generated for the Likert scale variables to identify the respondents' attitudes towards the COVID-19 vaccine and their degree of willingness to take the vaccine. T-tests and one-way ANOVA tests, followed by post-hoc pairwise t-tests with p-values corrected for multiple comparisons using the Benjamini-Hochberg (BH) correction, were used to determine the relationship between demographics and responses related to attitudes and willingness as measured by the Likert scale variables. The Likert variable measuring willingness to take vaccine was regressed against the other scale variables and the key demographics. The main predictors were then identified as the ones for which this multivariate regression gave significant beta coefficients. Pearson correlation coefficients were calculated to determine which factors could influence respondents' decision to take the vaccine. Chi-squared statistics were used in Study 2 to determine associations between demographics and willingness to take the COVID-19 vaccine and reasons for being unsure or unwilling to take the COVID-19 vaccine. The level of significance was set at p<0.05
Controlling for duplicates and sampling bias
The only manner in which google forms allows for control of duplicate responses is to allow it to record the email of the respondent. Since the questionnaires were anonymous, this was not possible. The data was reviewed and cleaned prior to analysis.
The methodology employed, whereby the questionnaires were initially disseminated by the investigators, could lead to selection bias, whereby respondents would pertain to a demographic similar to the investigators. This was mitigated by employing snowball sampling following the initial volunteer sampling.
The study received ethical clearance by the University of Malta Ethics Research Committee UREC. (Ethics ID 6443-22092020).
RESULTS
A total of 2529 individuals participated in the first study as illustrated in Table 1. The sample participants were predominantly female (72.3%), with nearly 60% having a tertiary education. All age groups had a good representation.
Table 1. Demographic and descriptive data for Study 1 and Study 2
| N (%) | Study 1 | Study 2 |
|---|---|---|
| Gender | ||
| Male | 655 (25.9) | 220 (26.4) |
| Female | 1827 (72.3) | 609 (73.0) |
| Prefer not to say | 7 (0.2) | 5 (0.6) |
| Age (years) | ||
| 19 or under | 59 (2.3) | 40 (4.7) |
| 20-29 | 307 (12.1) | 136 (16.1) |
| 30 -39 | 486 (19.2) | 141 (16.7) |
| 40-49 | 657 (26.0) | 212 (25.1) |
| 50-59 | 518 (20.5) | 169 (20.0) |
| 60 and over | 456 (18.0) | 126 (15.0) |
| Marital status | ||
| Single | 522 (20.6) | N/A |
| In a relationship/married | 1727 (68.3) | N/A |
| other | 246 (9.2) | N/A |
| Level of education | ||
| Primary | 21 (0.8) | 5 (0.6) |
| Secondary | 380 (15.0) | 91 (10.8) |
| Post-secondary | 595 (23.5) | 172 (20.4) |
| Tertiary/further education | 1502 (59.4) | 562 (66.6) |
| Country of residence | ||
| Malta | 2529 (100) | 719 (85.2) |
| Other | - | 103 (12.3) |
| Healthcare worker (HWC) | ||
| Yes | 368 (14.6) | N/A |
| No | 2121 (83.9) | N/A |
| Chronic/long term condition | ||
| Yes | 582 (23.1) | N/A |
| No | 1737 (75.3) | N/A |
| Influenza vaccine last year | ||
| Yes | 759 (30.1) | N/A |
| No | 1737 (68.7) | N/A |
Percentages do not add up to 100% due to missing data
The second study, the demographics of which are presented in Table 1, was primarily targeted at finding out the reasons why participants were against or unsure of taking the vaccine. There were 843 respondents with a similar general profile to the first study. Of the participants, 12.3% were international respondents. Just over half (51.0%) of the participants stated that they were willing to take the vaccine, 32.6% were unsure and 15.6% were not willing to take the vaccine.
Study 1
Attitudes towards COVID-19 vaccine and influencing factors
The results presented in Table 2 relating to attitudes towards the COVID-19 vaccine and relevant influencing factors, demonstrates that in most questions, 50% of respondents gave a score of 8 or above (score of 1 indicated an absolute negative response and a score of 10 an absolute positive response).
Table 2. Study 1- Attitudes toward COVID-19 Vaccine and influencing factors
| Attitude towards COVID-19 Vaccine | Mean (SD) | Minimum | Q1 | Median | Q3 | Maximum |
|---|---|---|---|---|---|---|
| I would take the Covid-19 vaccine when it becomes available | 6.85 (3.19) | 1 | 5 | 8 | 10 | 10 |
| How much would you say that you know about COVID-19 | 7.38 (1.67) | 1 | 6 | 8 | 8 | 10 |
| How much news and information have you seen and heard about COVID-19 | 8.46 (1.47) | 1 | 8 | 9 | 10 | 10 |
| I engage in preventive behaviour(wearing mask/visor, social distancing, frequent hand washing, sanitiser use) | 9.28 (1.24) | 1 | 9 | 10 | 10 | 10 |
| I believe that the COVID-19 vaccine will help protect the people who take it. | 7.50 (2.59) | 1 | 6 | 8 | 10 | 10 |
| The opinion of family and friends is important in my decision to take COVID-19 vaccine | 4.82 (3.10) | 1 | 2 | 5 | 8 | 10 |
| I value the advice of health professionals regarding the effectiveness of the COVID-19 vaccine | 8.00 (2.44) | 1 | 7 | 9 | 10 | 10 |
Q1: 1st Quartile; Q3: 3rd Quartile.
Welch t-tests indicated that women were more likely than men to engage in preventive behaviours such as mask/visor wearing, handwashing/sanitizing and social distancing (t=8.97, df=949.14, p<0.00005) but to believe less that the COVID-19 vaccine will help protect the health of the people who take it (t=-3.6479, df=1147.6, p=0.0003). Men were more likely to value the advice of health care professionals regarding the effectiveness of the COVID-19 vaccine (t=2.3364, df=1183.8, p=0.02) and were more likely to be willing to take the vaccine (t=5.83, df=1164.2, p<0.00005).
Willingness to take the COVID-19 vaccine
The key Likert variable was the respondents' score to the statement “I will take the Covid-19 vaccine when available” which will be referred to as the variable “WillTake”. The mean score of “WillTake” among all respondents was 6.85 SD=3.19 with a median of 8 indicating that 50% of respondents scored 8 and over. This implies a strong willingness to take the vaccine
There was a strong correlation between participants who believed that vaccination will help protect people against COVID-19 and willingness to take vaccine (r=0.79, p<0.005). There was also a significant relationship between willingness to take the vaccine and giving importance to the opinions of family and friends. Pearson's correlation coefficient r for the relationship between willingness to take the vaccine and giving importance to the opinion of family and friends was quite significant (r=0.22, p<0.005), but an even more significant relationship was found between willingness to take the vaccine and the importance given to the advice of health professionals (r=0.74, p<0.005).
A one-way ANOVA test of the scale variable “WillTake” with age showed significant differences between the age groups (F(5,2420)=3.34, p=0.005). To ascertain between which age categories this difference was significant, ANOVA was followed by post-hoc pairwise t-tests with p-values corrected for multiple comparisons using BH correction. Results showed that respondents over the age of 60 were more willing to take the COVID-19 vaccine as compared to those between the ages of 30-39 (p<0.02) and those between 40-49 years of age (p<0.01). The one-way ANOVA of “WillTake” by level of education indicated no significant differences between the educational categories (F(3,2476)=2.15, p=0.09), although there was a very strong difference among the educational categories in the belief that the COVID-19 vaccine will protect against the virus (F(3,2477)=8.01, p<0.00002). Those having a tertiary education were more likely to believe that the vaccine will help protect the health of the people who take it, than those whose highest qualification was secondary (p=0.003) and post-secondary education (p=0.0003).
Predictors of willingness to take COVID-19 Vaccine
Regression analysis was conducted to determine predictors of willingness to take the COVID-19 vaccine. As indicated above, the variable “WillTake” showed a strong willingness by most of the respondents to take the vaccine. A good indication of this positive attitude towards the vaccine was also shown by the fact that more than half of the respondents (56%, n=1196) would encourage their elderly parents to take the vaccine, 32% (n=674) were unsure and only 12% (n=263) of those who answered would not. As expected, respondents were more cautious in declaring their willingness to give the vaccine to their children: of those who answered the question 43% (n=654) said 'yes', 36% (558) were unsure and 21% (n=321) said 'no'.
A regression analysis was carried out to determine the best predictors of willingness to take the vaccine. The variable 'WillTake' was the predicted variable while the main demographic variables and the other scale variables were the predictors.
The regression model obtained explained 83% of the variance (R2=0.834). Residual standard error was 1.355 on 1351 degrees of freedom. Table 3 lists the beta coefficients of the predictors of willingness to take the vaccine.
Table 3. Study 1 - Regression predicting willingness to take COVID-19 vaccine
| Variable | Beta | p-value |
|---|---|---|
| Knows about COVID-19 | -0.021887 | 0.41243 |
| News and Information seen about COVID-19 | -0.013112 | 0.65409 |
| I engage in preventative behaviour | -0.028971 | 0.35847 |
| Believes that COVID-19 vaccines will help protect the health of the people who take it | 0.228807 | <0.0005 |
| Opinion of family and friends important in decision to take COVID-19 vaccine | 0.016498 | 0.20025 |
| Value the advice of healthcare professionals re effectiveness of COVID-19 vaccine | 0.236737 | <0.0005 |
| Is a health worker | 0.050775 | 0.63272 |
| Has a chronic condition | 0.008421 | 0.92905 |
| Sex male | 0.176704 | 0.5311 |
| Age 20-29 | 0.208428 | 0.62593 |
| Age 30-39 | 0.301352 | 0.45829 |
| Age 40-49 | 0.284435 | 0.48095 |
| Age 50-59 | 0.301576 | 0.45694 |
| Age 60 and over | 0.427421 | 0.30803 |
| Education primary | 0.356446 | 0.41913 |
| Education secondary | -0.030026 | 0.81031 |
| Education tertiary/further | -0.077934 | 0.40024 |
| Had flu jab last year | 0.276383 | <0.0020 |
| Unsure if give COVID-19 vaccine to children | 2.036730 | <0.0005 |
| Willing to give COVID-19 vaccine to children | 4.241188 | <0.0005 |
| Unsure if encourage COVID-19 vaccine to elderly parents | 0.285070 | 0.08969 |
| Willing to encourage COVID-19 vaccine to elderly parents | 1.065202 | <0.0005 |
Study 2
Descriptive data of the study population (N=843) for Study 2 is presented in Table 1. Of the participants, 73% were females and 66.6% had a tertiary education. The reasons for refusing to take the vaccine or being unsure are illustrated as percentages in Figure 1 and Figure 2. The main issue for not wanting to take the vaccine is related to the belief that it may not be safe (85.2%, N=132). Oddly, fear of injections was cited as the major reason for being unsure of taking the vaccine (82.5%, N=275) followed by 56% who declared that they wanted more information about the vaccine and 50.1% who would not be willing to be among the first to take the vaccine.
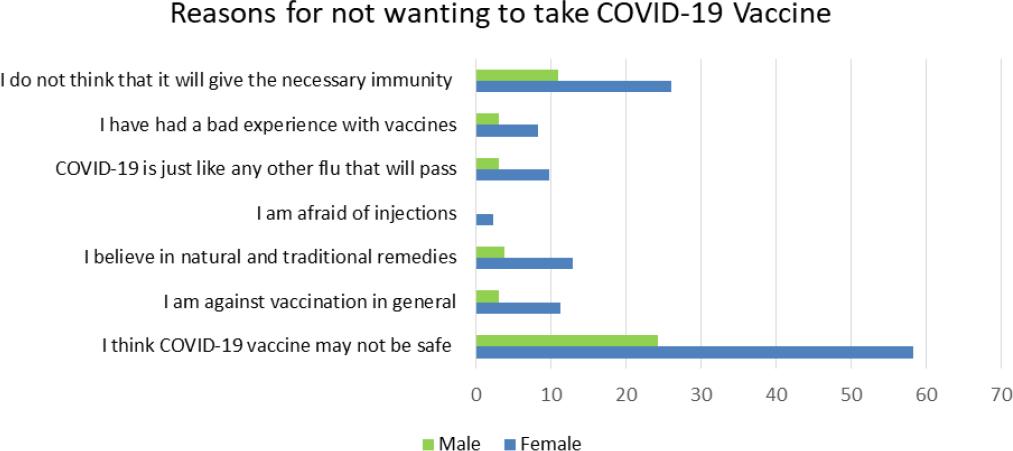
Figure 1. Study 2 - Reasons given by respondents who were unwilling to take COVID -19 vaccine presented as percentages (N=132)
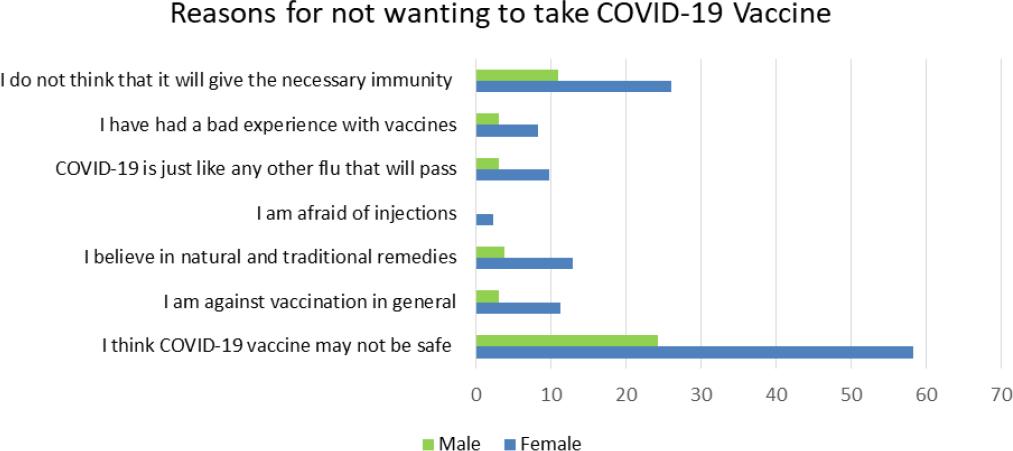
Figure 2. Study 2 - Reasons for being unsure whether to take vaccine presented as percentages (N=275)
When studying willingness to take the vaccine in terms of demographics, males were more willing to take the vaccine, while females were more likely to declare that they were unsure (chi-square=14.63, df=4, p=0.006). Different age groups also gave statistically different responses with those between the ages of 40 to 49 years old being more likely to state that they were unsure whether to take the vaccine while those who were 60 years and over being more likely to say that they intended to take the vaccine (chi-square=23.99, df=10, p=0.007).
The predetermined reasons given for being unsure or unwilling to take the vaccine did not significantly differ between respondents. The only exception was being unwilling to take the vaccine due to fear of injections: females were more likely to give this reason then males (chi-square=7.43, df=1, p=0.0064) and Maltese residents were more likely to give this reason when compared to international respondents (chi-square=7.87, df=1, p=0.005).
Additional comments were provided by individuals who were unwilling or unsure of taking the vaccine presented in Table 4.
Table 4. Study 2 - Additional reasons for not refusing to take vaccine and being unsure of taking COVID-19 vaccine
| Reasons for refusing | Reasons for being unsure |
|---|---|
| • Too short a time for development and testing (10 comments) | • Planned pregnancy/fear of being pregnant (3 comments) |
| • Long term repercussions (2 comments) | • Prefer vaccine that has been tested |
| • Do not trust system | • Allergic to latex |
| • Political game | • Afraid of long-term effects (2 comments) |
| • I want to build my own immunity | • Not convinced of number of infected reported |
| • Harmful substance in vaccine (2 comments) | • Never took vaccine before |
| • Vaccine not reliable | • Not convinced of the safety standards of vaccine |
| • Have a condition/cancer (2 comments) | • How long will immunity last? |
| • Do not believe COVID is a threat | • Length of testing too short |
| • Vaccine will not help | • Something that nobody knows about |
| • Vaccine is a money-making venture | • Depends where it has been developed |
| • Not safe with lower efficacy | • Would like to know how effective it is |
| • I am not a guinea pig |
DISCUSSION
The two consecutive studies conducted sought to demonstrate willingness to take the COVID-19 vaccine, predictors of vaccine uptake and possible reasons for vaccine hesitancy. The present studies have demonstrated encouraging results in terms of willingness for vaccine uptake, with over 50% indicating a very strong willingness to take the vaccine and 32.6% being unsure, at a time when information about the safety and efficacy of the vaccines was rather limited. The data collection period also coincided with Malta entering into the second wave of the pandemic. Study 2 identified that 15.6% were categorically against taking the vaccine. The results for vaccine uptake are in line with to international studies. Willingness to take the vaccine from a European study was reported at 73.9%, the UK Oxford study reported 71.7%, a global survey of 19 countries was 71.5% and in the USA 52% were very likely and 27% somewhat likely to take the vaccine.29-32 Data for refusal to take the vaccine was within the range of internationally reported numbers.29,33-36
Vaccine hesitancy is related to attitudes.13 Participants who were unsure whether or not to be vaccinated wanted more information about the vaccine. The availability of increased information with regards to safety and efficacy of the vaccines is however rivalled by the misinformation circulating on the social media. Those who were categorical in their intention not to take the vaccine had a different set of attitudes which exhibited a general lack of faith in vaccines. This is especially evident in the data presented in Figures 1 and 2 and Table 4.
The attitudes of significant others were identified as being an important factor influencing vaccine uptake. A strong positive correlation was found between willingness to take the vaccine and giving importance to the opinion of family and friends as well as valuing the advice of health care professionals. Males were more likely than females to value the advice of health care professionals regarding the effectiveness of the vaccine. The results reflect this argument and support the Theory of Reasoned Action and the Theory of Planned Behaviour.20,24
Respondents believed that they were very knowledgeable and were well informed through the media about COVID-19 as seen in Table 2. Interestingly these two factors did not feature as predictors of vaccine uptake. While copious amounts of information are available, especially on social media, a lot may be misleading, bias or untrue, fuelling vaccine hesitancy. The World Health Organization is doing its utmost to identify and address misinformation -however, increased responsibility and appropriate and effective campaigns are still necessary globally.37 Positive attitudes toward vaccination can be encouraged through media advocacy involving the strategic use of social media for advancing a social or public policy initiative such as vaccination. Through advocacy, decreasing vaccine hesitancy and promoting vaccination is no longer seen as an issue concerning the individual but rather a societal concern placed at the top of the public agenda.
Gender has been demonstrated to be a significant issue during this pandemic. The present study showed that while women were more likely to engage in preventive behaviour as demonstrated in other studies, they were less likely to believe that the vaccine will protect the health of the people who take it and were less willing than men to take the vaccine.38-40 The latter was evident in both studies with more females declaring that they are unsure of taking the vaccine. This lack of conviction by women has been identified by a number of other studies.41,42 A study conducted in eight OECD countries which undertook a detailed analysis regarding gender-based issues pertaining to the pandemic demonstrated the same results and recommended gender-based public health policies and communication.43 Taking a vaccine may be considered a risk and studies about decision making and risk taking among men and women based on a psychological assessment of risk personality show that women are more cautious and take longer to evaluate risk.44,45 Oddly, the fear of injections was a significant reason as to why females in Malta were unsure of taking the vaccine. This reason was found to be of minimal concern in a European study.29
Respondents between the ages of 30 and 49 appear to be less willing to take the vaccine than those over 60 years of age. These findings are supported by other studies in the US, UK and Ireland.42,46 The US study analysed national trends, between April and December 2020, in the public's likelihood of getting the vaccine and reported that those aged over 65 are more willing to take the vaccine than those between 18-49 years.46 Similarly the UK reported that those over 65 were less resistant to taking the vaccine and in Ireland those who were more resistant were between the ages of 25 and 44.42 These results could be indicative that the message regarding the vulnerability of the elderly to COVID-19 is clear and has been received.
While educational background had no influence on willingness to take the vaccine, those with a tertiary education were more likely to believe that the vaccine will protect the people who take it. Conversely, in US studies people with a bachelor's degree or higher were more likely to be willing to get vaccinated.46,47
The best predictors obtained by regressing willingness to take the COVID-19 vaccine on the other Likert scale variables and the main demographic factors largely confirmed results obtained from pairwise correlations, chi-squared tests, ANOVAs and t-tests. It is to be expected that not wanting to give the vaccine to one's children and elderly relatives are strong predictors of not willing to take the vaccine oneself. Having taken the flu vaccine last year is a strong predictor of willingness to take the COVID-19 vaccine. The latter would seem to indicate that a positive attitude towards the COVID-19 vaccine goes along with a positive view towards vaccination in general. The fact that willingness to take the vaccine is strongly predicted by belief that it will help protect the health of the people who take it and also by valuing the advice of health professionals would seem to indicate that vaccine hesitancy is strongly related to mistrust in medical evidence.
Vaccine hesitancy is more of a continuum than a binary decision. At one end there are those who accept all vaccines with no doubts, at the other end are those who completely refuse vaccination and then there is a heterogeneous group in the middle of the continuum. These tend to delay vaccination or accept vaccination but are unsure in doing so.13 Social psychological theories propose that it is easier to change the attitudes if they are within the 'latitude of acceptance'.23,48-51 For this reason campaigns are most effective when targeteding this heterogeneous group of people in the middle of the continuum.52 Campaigns are unlikely to change attitudes of those who are directly opposed to vaccination and therefore these should not be targeted initially. Communication campaigns promoting group strategies can encourage cohorts of people to move from knowledge to action.
The main strength of this study was the large number of respondents, especially in Study 1. Additionally, Study 2 was found to clearly support and complement the findings of study 1. However, the results need to be interpreted with caution due to some limitations. These are cross-sectional studies conducted on social media. The responses therefore exclude those who do not use social media. There respondents are predominantly female and have a tertiary education and as such are not representative of the general population. Response bias in favour of those having a positive attitude towards the vaccine could have also been present. The studies were conducted at a time where the health landscape was, and still is, extremely fluid with much more limited information about COVID-19 and the COVID-19 vaccines. Responses are therefore reflective of the information available at the time.
CONCLUSIONS
A generally positive attitude towards COVID-19 vaccine has been reported and clear predictors of willingness to take the vaccine have been identified. The opinion of significant others, such as family, friends and healthcare professionals were positively associated with willingness to take the vaccine A degree of vaccine hesitancy was present, primarily in women and mainly linked to lack of conviction about vaccine safety. Therefore, information campaigns should focus on providing more information about COVID-19 vaccine safety, reassuring the population, especially women. The positive link identified between the opinions of significant others and vaccine uptake, indicates that vaccine strategies targeted at groups of individuals such as work groups and leisure groups are likely to be more effective.














