Despite numerous theories and extensive research aiming to understand, predict and prevent suicide, the complexity of this phenomenon remains difficult to grasp (Chan et al., 2016; Forkmann et al., 2020; O'Connor & Kirtley, 2018; Van Orden et al., 2010). Expert recommendations stress the need to better describe the phenomenology of suicide, and to do so and in close connection with the clinical assessment and management of people at risk (Al-Halabí & Fonseca-Pedrero, 2021; Hawton et al., 2022; Kessler et al., 2020; Millner et al., 2020; Mou et al., 2020; Pompili, 2018). According to APA, suicidality may present as thoughts (ideas, plans, communication, threats to act, …), behaviors (varying in intentionality, methods and lethality), or risk factors (exposure, social status, self-harming behavior, mental disorder, …) and has a temporality (chronic, repetitive, acute) (Jacobs & Brewer, 2004; Paris, 2002). Given the diversity of factors involved, one pertinent avenue of inquiry is to focus on the mental content characteristic of acute suicidal states. Indeed, theoretical models of suicide refer to socio-cultural norms, thoughts, values and attitudes towards death, to feelings of entrapment and belongingness, i.e. to mental contents involved in suicidality (O'Connor & Kirtley, 2018; Turecki et al., 2019; Van Orden et al., 2010; Vanzyl et al., 2022). Clinically, assessing the mental contents of people experiencing a suicidal crisis can inform the process of case formulation. Furthermore, identifying resources linked to the desire to live at a moment when contradictory wishes to die are also present can foster therapeutic communication. The beliefs and thoughts of individuals in suicidal crisis are therefore key elements to study (Baldessarini, 2020; Gysin-Maillart et al., 2016; Harris et al., 2018; Puddephatt et al., 2021; Schuck et al., 2019; Van Heeringen & Mann, 2014). In this vein, and adopting an orientation towards life focusing on beliefs and values that can steer individuals away from suicidal behavior, Marsha Linehan and her colleagues developed the "Reasons For Living Inventory" (RFLI) (Linehan et al., 1983). This self-report scale has been extensively studied and validated (O'Connor & Nock, 2014). Initially, the RFLI was generated from the answers given by a general population sample asked to list the reasons they had not to kill themselves if they were faced with the idea of suicide. Those reasons were then submitted to another general population sample that included individuals both with and without history of suicidal ideation or attempt. Factor analyses have led to consider 6 factors translating the domains of reasons for living : "Child Related Concerns", "Fear of Social Disapproval", "Fear of Suicide", "Moral Objections", "Responsibility to Family", and "Survival and Coping Beliefs" (which includes positive expectations about the future and trust in personal coping abilities). The 6-factor structure of the RFLI was confirmed by 8 studies on clinical and non-clinical samples in different countries (Cwik et al., 2017; Innamorati et al., 2006; Labelle et al., 1996; Linehan et al., 1983; Osman et al., 1991, 1993, 1999; Ronconi et al., 2009). Linehan's reasons for living are thought to reflect a sense of meaning and purpose in life, and to cover main areas of beliefs and values : on coping abilities, on sense of belonging, on social support, and on religion (Vanzyl et al., 2022).
Numerous studies have tested Linehan's RFLI with clinical and general population samples, and examined its relationships with gender, age, and suicidality (Ehret et al., 2023; Galfalvy et al., 2006; Gorraiz et al., 2023; Linehan et al., 1983; Marty et al., 2010; Osman et al., 1991). They converge to indicate that RFLI scores correlate negatively with suicidality (Christensen et al., 2021; Cwik et al., 2017; Innamorati et al., 2006; Labelle et al., 1996; Linehan et al., 1983; Lizardi et al., 2009; Mann et al., 1999; Moscardini et al., 2022; Osman et al., 1999; Tillman et al., 2017). Regarding gender, some findings show no difference between men and women while others suggest that reasons for living in women would be higher and more strongly correlated with suicidality than in men (Ellis & Lamis, 2007; Innamorati et al., 2006; Lamis & Lester, 2013; Lizardi et al., 2007; Oquendo et al., 2007; Osman et al., 1992; Pompili, Innamorati, et al., 2007; Rich et al., 1992; Segal & Needham, 2007). Regarding age, reasons for living would increase and differences between men and women diminish in older samples (Miller et al., 2001; Segal & Needham, 2007). Regarding correlations between reasons for living, a meta-analysis of 39 studies covering 15 countries worldwide emphasizes the key importance of "Moral Objections", "Survival and Coping Beliefs" and "Child Related Concerns", and concludes on their predictive value and protective role against suicidal ideation and behavior (Laglaoui Bakhiyi et al., 2016). In addition, this meta-analysis shows that 14 studies involved non-suicidal community samples, 25 studies involved clinical samples, 7 involved hospitalized patients in psychiatry, within which hospitalization was related to suicidality in 4 studies (Gilbert et al., 2011; Lizardi et al., 2007; Malone et al., 2000; Mann et al., 1999). Recent research on protective and risk factors for suicidal crises (such as resilience, emotion regulation, social support, loneliness, childhood abuse, impulsivity, aggressivity, sleep disorder, depression, hopelessness) supports the independent contribution of reasons for living to risk attenuation (Gorraiz et al., 2023; Laglaoui Bakhiyi et al., 2017; Marty et al., 2010; Moscardini et al., 2022; Rich et al., 1992; Tsypes et al., 2022). Previous findings also suggest that reasons for living are heterogeneously distributed among individuals (in particular by gender and age), and that it may be possible to discern different profiles of reasons for living characterized by different distributions of scores in "Survival and Coping Beliefs", "Responsibility to Family", "Child-Related Concern", "Fear of Social Disapproval" and "Moral Objections" (Laglaoui Bakhiyi et al., 2016; Malone et al., 2000; Oakey-Frost et al., 2022; Pinto et al., 1998; Tillman et al., 2017).
In brief, the evidence suggests that high scores on the RFLI are associated with a reduction in suicidality. However, most studies have involved people with negligible to moderate risk (general population with no suicidal ideation to psychiatric outpatients under treatment). Given the challenge to understand and treat acute suicidal states, our study is the first to investigate reasons for living in a psychiatric emergency unit during a suicidal crisis. The primary objective of this study was to characterize reasons for living reported by adults during a suicidal crisis hospitalization. Then we aimed to investigate how reasons for living can be relevant to differentiate groups of patients and in relation with suicidality. Further, we aimed to investigate potential differences between adults above 25 and youths aged 18 to 25 who are at heightened suicidal risk (Besch, Greiner, et al., 2020; Bilsen, 2018; Blasco et al., 2016; Cha et al., 2018; Fusar-Poli, 2019; Scardera et al., 2020; World Health Organization, 2021). Clinically, this study sought to identify the mental contents that may constitute strengths or, conversely, be impaired, in order to fuel case formulation and therapeutic intervention with personalized, life-oriented information (Berk et al., 2020; Besch, Debbané, et al., 2020; Gysin-Maillart et al., 2016; Tillman et al., 2017; Vanzyl et al., 2022).
Method
Participants
Participants (N = 61, 66% women) were enrolled in this study after they have been admitted to the "Crisis Intervention Beds" (CIB), a specialized psychiatric unit at Geneva University Hospital which provides a 7-day care to people in suicidal crisis (Greiner et al., 2023). People are admitted to the CIB when they have been assessed as being in acute risk of suicide by psychiatric emergencies or outpatient psychiatrists. The decision to admit is taken by CIB psychiatrists for one of three motives : suicide attempt, suicidal ideation, or acute suicide risk without explicit ideation nor behavior. Admission to CIB includes people without a diagnosis of mental disorder, and in 70% of cases the contact with emergency psychiatry is in fact the first contact of an individual with the inpatient mental health system (Besch, Greiner, et al., 2020; Walter & Genest, 2006). Exclusion criteria relate to conditions that are incompatible with an open inpatient care unit : severe symptoms of disorganized thought, mental retardation, psychomotor agitation with or without auto- or hetero-aggressivity, substance abuse in need for withdrawal, physical conditions that require priority somatic care (e.g. injuries or eating disorders). On average between 350 to 400 patients are typically admitted yearly, approximately 33% men, with a mean age of 36 years. Psychiatric diagnoses are made by CIB psychiatrists on the basis of clinical interviews and observation of patients during their stay.The main diagnosed disorders are depression, personality disorders, post-traumatic stress disorders and substance use disorders, and half the patients present psychiatric comorbidities (Besch, Greiner, et al., 2020).
Instruments
Patients' reasons for living were assessed using Linehan's RFLI (Linehan et al., 1983). The RFLI is a 6-point Likert scale with 48-items and 6 subscales. Its psychometric indices validating a 6-factor structure on a sample of 532 healthy adults aged 26 to 65 are acceptable to good: X2(1065,532) = 3750.30, p < .01, NNFI = .91, CFI = .91, and RMSEA = .07 (Ronconi et al., 2009). Its test-retest reliability indices on a sample of 110 healthy students assessed at a 3-week interval show a high stability: on total RFL score r = .83, p < .05, on subscales the minimal is for "Fear of Social Disapproval" r = .75, p < .05, and the maximal for "Moral Objections" r = .85, p < .05 (Osman et al., 1991). Its internal consistency indices have been extensively published, they indicate that subscales have good to high internal reliability: "Child Related Concerns" Cronbach's α mini = .72 maxi = .84, "Fear of Social Disapproval" Cronbach's α mini = .76 maxi = .84, "Fear of Suicide" Cronbach's α mini = .74 maxi = .82, "Moral Objections" Cronbach's α mini = .74 maxi = .80, "Responsibility to Family" Cronbach's α mini = .64 maxi = .82, "Survival and Coping Beliefs" Cronbach's α mini = .89 maxi = .92 (Innamorati et al., 2006; Linehan et al., 1983; Osman et al., 1991, 1993; Pompili, Innamorati, et al., 2007; Ronconi et al., 2009).
Suicidality was assessed by 3 sets of variables: motive for the present hospitalization, level of suicidal ideation, and suicidal history. Those suicidality variables were informed from different sources and over 2 periods of time. The motive for the present hospitalization was defined at intake by the psychiatrist who decided for the admission with a distinction between suicide attempt, suicidal ideation, and acute risk. The level of suicidal ideation was self-reported by participants between day 3 and day 5 of their hospitalization. Using the visual analogue scale, we employed the average level of suicidal ideation over the previous two weeks rated by patients on a 0 to 10 likert scale (Bryan, 2019; Jollant et al., 2019; Lesage et al., 2012). History of suicide attempt, self-harming behavior and suicide-related hospitalization were collected from participants medical record.
Procedure
Patients enrolled in this study matched with overall CIB population in terms of age, gender, and diagnosed mental disorders (Besch, Greiner, et al., 2020). Recruitment and participation were done in compliance with the intensive care pathway of patients during their stay, which includes 4 phases: admission (day 1), disclosure of the crisis (days 2-4), case formulation (days 5-6), preparation for discharge (days 6-7) (Bateman et al., 2023; Greiner et al., 2022). After the admission phase, and depending of their emotional and cognitive state, patients were proposed by their referring psychiatrist. During the disclosure and formulation phases, participants filled in self-report questionnaires and took a semi-structured interview based on Linehan's RFLI with a senior clinical psychologist.
The study was approved under project-id 2021-01100 by the "Commision Cantonale d'Ethique sur la Recherche" (CCER), the swiss ethics commission.
Data Analysis
This case series is a mixed-method study aiming to analyze the reasons for living in a sample of adults currently hospitalized for a suicidal crisis. It entails describing patients reasons for living, assessing the relationships between reasons, and further examining their associations with suicidality variables. In line with the case series methodology, it is not intended to test hypotheses nor to produce inferential statistical results (Carey & Boden, 2003; Grimes & Schulz, 2002, 2002; Kooistra et al., 2009; Murad et al., 2018; Torres-Duque et al., 2020). It is expected that the results will be valuable in generating hypotheses to be tested in future studies. Chi-square tests, t-tests and ANOVA were used to control for the statistical significance of the associations and differences within this study sample (Dalziel et al., 2005; Galfalvy et al., 2006; Nagata et al., 2013; Waller et al., 2018). Multiple correspondence analysis (MCA) was used to discern groups of individuals according to their reasons for living. MCA is a multivariate analysis technique particularly useful to describe qualitative variables and identify possible underlying relationships between them without prior assumptions (Méndez-Bustos et al., 2022). MCA is suitable for non-normal distributions, non-linear relationships between variables, and shows little sensitivity to outliers (Joyal et al., 2011). Its principle is to convert a set of variables (categorical or not) into low-dimensional variables, and to position the individuals in the low-dimensional space so as to be able to sort them according to their proximity. MCA is relevant for this case series as it can highlight proximities between individuals and reveal groups whose reasons for living correspond (Richard-Devantoy et al., 2016).
Data were managed using Excel, Jamovi and SPSS.
Results
Table 1 presents the age and prevalence of mental disorders detailed by gender. The 3 main psychiatric diagnoses are depression, personality disorders and substance use disorders.
Table 1. N, Age, and Prevalence of Mental Disorders, Detailed by Gender.
| Variables | All | Women | Men |
|---|---|---|---|
| N (%) | 61 | 40 (66%) | 21 (34%) |
| Age mean (sd) | 37.3 (15.3) | 35.0 (15.0) | 41.7 (15.2) |
| Age mini - maxi | 19.0 - 68.2 | 19.0 - 68.2 | 19.5 - 64.8 |
| Prevalence of mental disorders | |||
| Anxiety/Phobia | 9.8% | 12.5% | 4.8% |
| Bipolar | 1.6% | 0.0% | 4.8% |
| Depression | 68.9% | 65.0% | 76.2% |
| PTSD | 1.6% | 2.5% | 0.0% |
| Substance Use Disorders | 19.7% | 10.0% | 38.1% |
| Eating Disorder | 1.6% | 2.5% | 0.0% |
| Personality Disorders | 75.4% | 85.0% | 57.1% |
| ADHD | 3.2% | 5.0% | 0.0% |
| Other | 4.9% | 2.5% | 9.5% |
Note.PTSD = Post-Traumatic Stress disorder, ADHD = Attention Disorder-Hyperactivity disorder. The sum of prevalences exceeds 100% due to comorbidities.
Table 2 presents the motive for hospitalization, suicidal ideation and suicidal history detailed by gender and age group with ε2 effect size estimate. Chi-square tests for motive for hospitalization indicate no differences between women and men (χ2(2,61) = 1.63, p = .442), nor between youths and adults (χ2(2,61) = 0.07, p = .964). Suicidal ideation does not differ between women and men (t(59) = 0.96, p = .344), while it is higher in youths than in adults (t(59) = -2.36, p = .022). Rate of history of suicide attempt does not significantly differ between women and men (t(59) = 0.92, p = .364), nor between youths and adults (t(59) = -1.18, p = .245). Rate of history of self-harming behavior does not differ between women and men (t(59) = 0.96, p = .340), while it is higher in youths than in adults (t(59) = -2.03, p = .047). Rate of history of suicide-related hospitalization does not significantly differ by gender nor age (t(59) = 0.11, p = .909 and t(59) = -0.12, p = .904).
Table 2. N, Age, and Suicidal Variables, Detailed by Gender and Age Group, with Effect Size Estimate.
| Variables | All | Women | Men | ε2 | Youths | Adults | ε2 |
|---|---|---|---|---|---|---|---|
| N (%) | 61 (100%) | 40 (66%) | 21 (34%) | 23 (38%) | 38 (62%) | ||
| Age mean (sd) | 37.3 (15.3) | 35.0 (15.0) | 41.7 (15.2) | 22.2 (1.9) | 46.5 (12.2) | ||
| Suicidal Variables | |||||||
| Motive for hospitalization | |||||||
| Acute Risk | 10% | 10% | 10% | <.01 | 9% | 11% | <.01 |
| Suicide Ideation | 72% | 67% | 80% | .02 | 74% | 71% | <.01 |
| Suicide Attempt | 18% | 23% | 10% | .03 | 17% | 18% | <.01 |
| Suicidal Id. mean (sd) | 5.89 (2.79) | 6.14 (2.80) | 5.35 (2.78) | .02 | 7.00 (2.27) | 5.21 (2.89) | .09 |
| Suicidal History | |||||||
| Suicide Attempt | 26% | 30% | 19% | .01 | 35% | 21% | .02 |
| Self-Harm. Behavior | 21% | 25% | 14% | .02 | 35% | 13% | .07 |
| Suicide Related. Hosp. | 30% | 30% | 29% | <.01 | 30% | 29% | <.01 |
Reasons for living scores, internal consistency statistic α and effect size estimate ε2 are given in table 3, compared by gender and age group. "Responsibility to Family" has the highest score relative to the other reasons, followed by "Child Related Concerns" and "Survival and Coping Beliefs", while "Moral objections" ranks lowest. A Kruskal-Wallis ANOVA test for non-parametric data (Chan & Walmsley, 1997) indicates that "Survival and Coping Beliefs" are higher in adults than in youths (χ2(1,60) = 4.50, p = .03.
Table 3. Reasons for Living Scores with Cronbach's α., and Compared by Gender and Age Group, with Effect Size Estimate.
| RFL | All | α | Women | Men | Youths | Adults | ||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| mean (sd) | mean (sd) | mean (sd) | χ²(1,60) | p | ε2 | mean (sd) | mean (sd) | χ²(1,60) | p | ε2 | ||
| CRC | 3.86 (1.9) | .83 | 3.86 (2.0) | 3.87 (1.7) | .06 | .81 | <.01 | 3.64 (1.8) | 4.00 (1.9) | .80 | .37 | .01 |
| FSD | 2.98 (1.5) | .72 | 3.18 (1.6) | 2.59 (1.3) | 1.79 | .18 | .03 | 2.88 (1.6) | 3.04 (1.5) | .17 | .68 | <.01 |
| FS | 3.06 (1.1) | .72 | 3.17 (1.1) | 2.86 (1.2) | .96 | .33 | .02 | 3.22 (1.3) | 2.97 (1.0) | .19 | .66 | <.01 |
| MO | 2.12 (1.4) | .79 | 2.21 (1.5) | 1.94 (1.1) | .04 | .85 | <.01 | 2.14 (1.3) | 2.11 (1.5) | .26 | .61 | <.01 |
| RF | 4.29 (1.1) | .83 | 4.46 (1.0) | 3.97 (1.3) | 1.79 | .18 | .03 | 4.35 (1.0) | 4.26 (1.2) | .02 | .88 | <.01 |
| SCB | 3.42 (1.1) | .96 | 3.36 (1.2) | 3.53 (1.0) | .60 | .44 | .01 | 3.00 (1.1) | 3.67 (1.1) | 4.50 | .03 | .08 |
| Total | 3.29 (0.9) | .94 | 3.37 (0.9) | 3.13 (0.8) | .51 | .48 | <.01 | 3.21 (0.9) | 3.34 (0.9) | .17 | .69 | .03 |
Note.CRC = Child Related Concerns, FSD = Fear of Social Disapproval, FS = Fear of Suicide, MO = Moral Ojections, RF = Responsibility to Family, RFL = Reasons For Living, SCB = Survival and Coping Beliefs.
Spearman correlations between reasons for living are indicated in table 4. After Bonferroni correction (corrected-p < .003), significant correlations are observed between "Survival and Coping Beliefs" and both "Child Related Concerns" and "Responsibility to Family", and between "Fear of Social Disapproval" and both "Survival and Coping Beliefs" and "Responsibility to Family".
Table 4. Spearman Correlations Between Reasons for Living.
| Reasons for Living | CRC | FSD | FS | MO | RF | SCB |
|---|---|---|---|---|---|---|
| CRC | - | |||||
| FSD | 0.147 | - | ||||
| FS | 0.066 | 0.306 | - | |||
| MO | 0.211 | 0.317 | 0.200 | - | ||
| RF | 0.359 | 0.521* | 0.004 | 0.222 | - | |
| SCB | 0.630* | 0.408* | 0.119 | 0.281 | 0.388* | - |
Note.CRC = Child Related Concerns, FSD = Fear of Social Disapproval, FS = Fear of Suicide, MO = Moral Ojections, RF = Responsibility to Family, SCB = Survival and Coping Beliefs.
*p < 0.003 after Bonferroni correction.
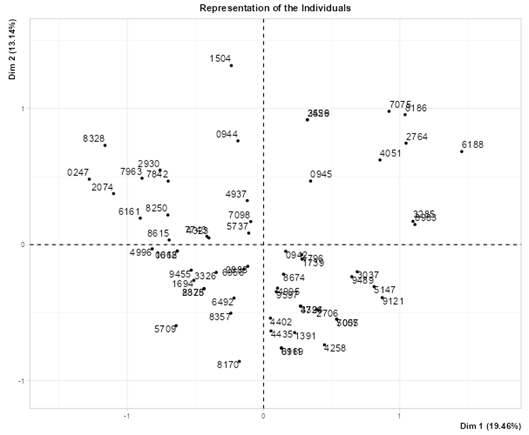
For each reason for living, individual scores were categorized into : "low" (first quartile; lower 25%), "medium" (second and third quartiles; 25-75% ) and "high" (upper quartile; > 75%). The 3 categories obtained for each reason for living then enabled the usage of Multiple Correspondence Analysis (MCA). Figure 1 shows that patients are distributed over the 4 quadrants in the MCA low-dimensional space. Analysis of this graphical representation, with a higher density in the bottom central part and more dispersed individuals in the upper left and right parts (U-shaped, or horseshoe curve), suggests a Guttman effect i.e. a quadratic correlation between low-dimensional variables. This is compatible with the first dimension (horizontal axis) discriminating between patients with high versus low scores, and the second dimension (vertical) between patients with medium versus extreme scores, and confirms the relevance of MCA to this study (Atkinson, 2023; Murakami, 2012).
Patients are grouped according to the quadrant in which they are positioned. This results in 4 groups; their characteristics and scores on RFLI are given in table 5. A Kruskal-Wallis ANOVA test with effect size estimate ε2 indicates that all reasons for living scores are significantly different between groups except for "Fear of Suicide".
Table 5. N, Age, and Reasons for Living Scores Compared by Group, with Effect Size Estimate.
| Variables | Group 1 | Group 2 | Group 3 | Group 4 | |||
|---|---|---|---|---|---|---|---|
| N (%) | 10 (16%) | 21 (34%) | 14 (23%) | 16 (26%) | |||
| Age mean (sd) | 45.5 (17.4) | 32.9 (13.4) | 39.8 (15.0) | 35.9 (15.5) | |||
| Age mini - maxi | 20.9-68.2 | 19.1-60.9 | 21.6-64.8 | 19.0-63.2 | |||
| RFL | χ²(3,60) | p | ε2 | ||||
| CRC | 5.07 (1.12) | 4.98 (1.27) | 3.38 (1.83) | 2.06 (1.29) | 27.79 | <0.001 | .46 |
| FSD | 5.03 (0.76) | 2.87 (1.04) | 2.05 (1.07) | 2.65 (1.74) | 22.22 | <0.001 | .37 |
| FS | 3.84 (1.26) | 3.01 (1.08) | 2.69 (1.13) | 2.97 (0.86) | 5.28 | 0.152 | .09 |
| MO | 3.48(1.49) | 2.46 (1.64) | 1.27 (0.45) | 1.56 (0.49) | 15.44 | 0.001 | .26 |
| RF | 5.31 (0.75) | 4.73 (0.59) | 3.72 (1.05) | 3.58 (1.23) | 24.47 | <0.001 | .41 |
| SCB | 4.39 (0.93) | 4.07 (0.81) | 2.85 (0.62) | 2.45 (0.93) | 28.99 | <0.001 | .48 |
| Total | 4.52 (0.49) | 3.69 (0.38) | 2.66 (0.48) | 2.54 (0.60) | 42.17 | <0.001 | .70 |
Note.CRC = Child Related Concerns, FSD = Fear of Social Disapproval, FS = Fear of Suicide, MO = Moral Ojections, RF = Responsibility to Family, RFL = Reasons For Living, SCB = Survival and Coping Beliefs.
As shown in figure 2, the first group (G1) corresponds to patients characterized by high scores on all reasons for living. The second group (G2) comprises patients characterized by high "Survival and Coping Beliefs", "Responsibility to Family" and "Child Related Concerns". The third and fourth groups (G3 and G4) correspond to patients with low scores except on "Child Related Concerns" and "Responsibility to Family" for group 3, and on "Responsibility to Family" for group 4.
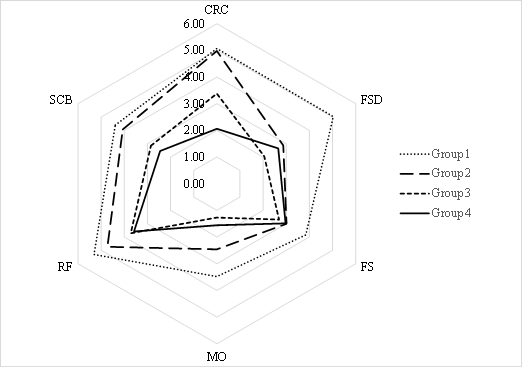
Note. CRC = Child Related Concerns, FSD = Fear of Social Disapproval, FS = Fear of Suicide, MO = Moral Objections, RF= Responsibility to Family, SCB = Survival and Coping Beliefs
Figure 2. Scores of Reasons for Living by Group
Dwass-Steel-Critchlow-Fligner test (Hollander et al., 2014) to compare groups pairwise indicates that "Fear of Social Disapproval" is higher in group 1 (G1-G2: W = -5.89, p < .001, G1-G3: W = -5.77, p < .001, G1-G4: W = -4.29, p = .013), "Child Related Concerns" is higher in groups 1 and 2 (G1-G4: W = -5.50, p < .001, G2-G4: W = -6.42, p < .001, G2-G3: W = -3.85, p = .033), "Survival and Coping Beliefs" is higher in groups 1 and 2 (G1-G3: W = -4.56, p = .007, G1-G4: W = -5.07, p = .002, G2-G3: W = -5.29, p = .001, G2-G4: W = -5.75, p < .001 ), "Responsibility to Family" is higher in groups 1 (G1-G2: W = -3.88, p = .031, G1-G3: W = -4.79, p = .004, G1-G4: W = -4.94, p = .003) and higher in group 2 than in groups 3 and 4 (G2-G3: W = -4.72, p = .005, G2-G4: W = -4.13, p = .018), and that "Moral Objections" is higher in group 1 compared to groups 3 and 4 (G1-G3: W = -5.24, p = .001, G1-G4: W = -4.51, p = .008).
The breakdown of patients by gender and age group in the reasons for living groups are presented in table 6. A chi-square test supports that differences between women and men are statistically significant (χ2(2,61) = 10.04, p = .018), in particular men of this sample are less represented in groups 1 and 4, and more in group 3. Differences between youths and adults are not statistically significant (χ2(2,61) = 2.96, p = .398).
Table 6. Breakdown in the Groups of Reasons For Living by Gender and Age Group.
| Group | Women | Men | Youths | Adults |
|---|---|---|---|---|
| 1. high on all reasons | 23% | 5% | 13% | 18% |
| 2. high SCB, CRC and RF | 33% | 38% | 43% | 29% |
| 3. low except CRC and RF | 13% | 43% | 13% | 29% |
| 4. low except RF | 33% | 14% | 30% | 24% |
Note.CRC = Child Related Concerns, RF = Responsibility to Family, SCB = Survival and Coping Beliefs.
Table 7 presents how the frequencies of motives for hospitalization, level of suicide ideation and suicidal history vary by group of reasons for living. Kruskal-Wallis ANOVA test indicates that between-group differences in history of self-harming behavior are statistically significant (χ2(2,61) = 8.29, p = .040), and differences in history of suicide-related hospitalizations are tendentially different (χ2(2,61) = 6.32, p = .097).
Table 7. Suicidal Variables Compared by Group of Reasons for Living, with Effect Size Estimate.
| Suicidal Variables | Group 1 | Group 2 | Group 3 | Group 4 | χ² (2,61) | p | ε2 |
|---|---|---|---|---|---|---|---|
| Motive for hospitalization | |||||||
| Acute Risk | 0% | 19% | 0% | 13% | 4.68 | .197 | .08 |
| Suicide Ideation | 80% | 67% | 79% | 69% | .98 | .805 | .02 |
| Suicide Attempt | 20% | 14% | 21% | 19% | .33 | .953 | .01 |
| Suicidal Id. mean (sd) | 6.00 (3.08) | 5.55 (3.12) | 5.73 (2.80) | 6.46 (2.22) | .55 | .907 | .01 |
| Suicidal History | |||||||
| Suicide Attempt | 10% | 24% | 21% | 44% | 4.06 | .255 | .07 |
| Self-Harm. Behavior | 10% | 5% | 36% | 38% | 8.29 | .04 | .14 |
| Suicide Related. Hosp. | 10% | 19% | 36% | 50% | 6.32 | .097 | .11 |
Discussion
This case series employed the Reasons for Living Inventory (RFLI) (Linehan et al., 1983) to examine the life-protecting beliefs and values of people hospitalized for suicidal crisis. It was motivated by the importance of mental contents, which critically inform models of suicide, and by the potential clinical benefits of connecting with people in suicidal crisis through resource- and life-oriented assessment. The aim was to explore reasons for living during a suicidal crisis, their associations with gender and age, and the possibility to differentiate groups of individuals according to their reasons for living. In this study women's scores on "Fear of Suicide" and "Responsibility to Family" are higher than men's, which, although not statistically significant, is in agreement with previous findings (Ellis & Lamis, 2007; Innamorati et al., 2006; Lamis & Lester, 2013; Pompili, Innamorati, et al., 2007). Regarding age, adults over 25 showed higher scores than those aged 18 to 25 in "Survival and Coping Beliefs", while a previous study supports significant differences in "Child Related Concerns" and "Moral Objections" between young and old adults (Miller et al., 2001). Looking at the order of importance of reasons for living, the ranking observed in this study differs from what has been reported in studies involving non-clinical people and people at low suicidal risk. In this case series, highest scores are observed for "Responsibility to Family", then "Child Related Concerns", followed in 3rd place by "Survival and Coping Beliefs", whereas previous studies converge in ranking "Survival and Coping Beliefs" first, followed by "Responsibility to Family" and "Child Related Concerns". In addition, previous studies have shown that "Moral Objections" comes fourth whereas here it is the least important reason for living (Berk et al., 2020; Dervic et al., 2011; Ellis & Lamis, 2007; Linehan et al., 1983; Ronconi et al., 2009). Looking at the relations between reasons for living, "Survival and Coping Beliefs" correlates most strongly with the other reasons, which is consistent with previous studies suggesting that it plays a central role in the beliefs and values that may protect individuals from suicidality (Ehret et al., 2023; Oakey-Frost et al., 2022; Osman et al., 1992, 1993; Ronconi et al., 2009; Tillman et al., 2017). By analyzing the proximity between individuals in terms of reasons for living, different groups of patients can be distinguished. This supports recent findings suggesting that people in suicidal crisis present heterogeneous profiles (Oakey-Frost et al., 2022; Tillman et al., 2017; Tsypes et al., 2022).
Results of this case series are in agreement with previous findings of a negative correlation between reasons for living and suicidality (Christensen et al., 2021; Cwik et al., 2017; Labelle et al., 1996; Linehan et al., 1983; Lizardi et al., 2009; Tillman et al., 2017). Regarding the relationships between reasons for living, the main specificity of this sample is that "Survival and Coping Beliefs" and "Moral Objections" have a lower relative importance than has been found in other studies among both non-clinical people and people at low suicidal risk not hospitalized (Berk et al., 2020; Dervic et al., 2011; Ellis & Lamis, 2007; Laglaoui Bakhiyi et al., 2016; Linehan et al., 1983; Lizardi et al., 2008; Ronconi et al., 2009). However, the central role of "Survival and Coping Beliefs" remains supported in patients in suicidal crisis by the fact that this reason correlates the most with the others and is significantly higher in groups of patients with highest total score and least suicidal history. The decrease in "Survival and Coping Beliefs" and "Moral Objections" during an acute suicidal state can be related to the clinical perception that a narcissistic collapse is at core of the suicidal crisis of certain patients, i.e. that they are experiencing a threat to their self-esteem together with a failure in their emotional regulation and external support resources (Gabbard, 2022; Hörz-Sagstetter et al., 2018; Ponzoni et al., 2021; Ronningstam et al., 2018; Ronningstam & Maltsberger, 1998). The low "Survival and Coping Beliefs" observed in this study is consistent with elements known to be involved in the mechanism of suicide such as reduced self-esteem, positive future thinking, problem solving and coping abilities, and increased hopelessness. This may lead to appraise a low score in "Survival and Coping Beliefs" as an index of increased suicidality (Benson et al., 2013; O'Connor & Kirtley, 2018; Turecki et al., 2019; Van Orden et al., 2010). In addition, high "Fear of Social Disapproval" is specific to the group with highest scores in reasons for living and lowest history of suicide attempt and suicide-related hospitalization. This is in agreement with the association between social bonding and reduced suicidality, and with the key role of social support in the universal prevention of suicide (Al-Halabí & Fonseca-Pedrero, 2023; Hayes et al., 2023; Labouliere et al., 2018; Van Orden et al., 2010). Finally, the possibility of distinguishing groups of individuals according to their reasons for living is supported by the clear differences measured between the groups observed in this study (Oakey-Frost et al., 2022; Tillman et al., 2017; Tsypes et al., 2022).
The clinical implications of this case series are fourfold. First, the study characterizes, for the first time, reasons to live at a time when individuals are experiencing an acute suicidal crisis motivating a psychiatric emergency hospitalization. Second, reasons for living are differentially associated to suicidality variables, and therefore may personalize the evaluation process and case formulation. Third, plausibly, reasons for living can be a topic of therapeutic communication during crisis intervention, helpful to connect the individual to personal and social resources, although this implication should be further investigated through clinical research. Finally, the groups identified through reasons for living may have distinct post-hospitalization trajectories, implying distinct therapeutic needs in the follow-up period, which we plan to assess with this sample of patients at 1-year follow-up evaluation.
The findings of this study are compatible with the assumption that different typologies of people in suicidal crisis can be distinguished based on their reasons for living, and that suicidality varies with these typologies. Future inquiry should address the limits of the present study. First, this study can not provide information on the direction of the association between reasons for living and suicidality variables, because it is based on historical and current data as in most other studies with a few exceptions (Lizardi et al., 2007; Oquendo et al., 2004; Tsypes et al., 2022). A longitudinal design would enable to assess the predictive power of typologies presented in this study, potential changes in reasons for living over time, and to study their dynamics and reciprocical interaction with suicidality. Future research should also assess their relations with external factors such as psychotherapeutic treatment, life events, social support or cultural environment (Al-Halabí & Fonseca-Pedrero, 2023; Berk et al., 2020; Laglaoui Bakhiyi et al., 2017; Pompili, Girardi, et al., 2007; Walker et al., 2010; Wang et al., 2013). To better understand interindividual differences in reasons for living, research should also consider psychological processes and personality variables (Bredemeier & Miller, 2015; Crandall et al., 2018; Heisel et al., 2016; Hörz-Sagstetter et al., 2018; Neacsiu et al., 2018). At last, a larger sample size is essential to provide sufficient statistical power to test hypotheses that can now be formulated : 1. Individuals in suicidal crisis may be classified according to different typologies of reasons for living ; 2. Suicide risk varies with those typologies ; 3. Typologies of reasons for living vary according to gender. 4. Suicidal ideation, behavior and lethality may be differentially associated with reasons for living. Gaining further knowledge into reasons for living may critically assist evaluation and intervention before, during and after a suicidal crisis.