Mi SciELO
Servicios Personalizados
Revista
Articulo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Accesos
Accesos
Links relacionados
-
 Citado por Google
Citado por Google -
 Similares en
SciELO
Similares en
SciELO -
 Similares en Google
Similares en Google
Compartir
Revista de Osteoporosis y Metabolismo Mineral
versión On-line ISSN 2173-2345versión impresa ISSN 1889-836X
Rev Osteoporos Metab Miner vol.14 no.4 Madrid oct./dic. 2022 Epub 27-Mar-2023
https://dx.doi.org/10.4321/s1889-836x2022000400006
ORIGINALS
Postoperative hypocalcaemia predictors after total thyroidectomy
1ENT Service. General University Hospital of Elda. Alicante (Spain)
2ENT Service. Doctor Peset University Hospital. Valencia (Spain)
Introduction and objective:
Given the increasing number of thyroid surgeries, the incidence of post-surgical hypoparathyroidism is on the rise. The frequency of hypocalcaemia due to hypoparathyroidism after total thyroidectomy is highly variable according to the literature (0.3-68%). The primary objective of this study is to analyze the biochemical, surgical and demographic factors related to an increased risk of hypocalcaemia.
Methodology:
This retrospective study encompasses 297 patients who underwent total thyroidectomy over a period of 8 years in a tertiary hospital. Demographic, clinical and biochemical data, both preoperative, intraoperative and postoperative, and their relationship with postoperative hypocalcaemia are analyzed.
Results:
The rate of total hypocalcaemia was 40.2%, being transient in 26.1%. Statistically significant variables were age (p=0.04), Graves' disease (p=0.04), carcinoma confirmed by pathology (p=0.04), two-stage thyroidectomy (p=0.00), the number of transplanted parathyroids (p=0.00) and pre- and post-operative PTH (p=0.03 and p=0.00) and the PTH gradient (p=0.00).
Conclusions:
This study demonstrates that there are a series of risk factors intrinsic to the patient and to the surgical procedure capable of predicting the risk of hypocalcaemia after total thyroidectomy. Possibly, the optimization of the surgical technique could prevent the appearance of hypocalcaemia after total thyroidectomy in some cases, while in others, the identification of these factors post-op could allow early detection and effective treatment of these patients. In the present study, age, Graves' disease, and parathyroid autotransplantation were associated with postoperative hypocalcemia. Thyroid carcinoma and two-stage thyroidectomy were protective factors.
Key words: total thyroidectomy; hypocalcaemia; hypoparathyroidism; risk factors
INTRODUCTION
Total thyroidectomy is one of the most frequent cervical surgeries, with a growing incidence in recent decades due to the increase in diagnoses of thyroid disease1-3. One of the thyroid surgery complications is hypocalcaemia due to iatrogenic hypoparathyroidism1,2,4-11. This hypo-function may be due to direct mechanical or thermal damage, inadvertent devascularization or removal of the parathyroid glands, post-surgical edema or hemorrhagic complications1-4,8,9,12. Both the direct damage, as well as the edema and devascularization, can be reversed over time. This explains why hypoparathyroidism is usually transient in most cases3,8,12.
According to the latest data provided by the Spanish Thyroid Cancer Association (AECAT), 75% of cases of hypoparathyroidism in Spain occur as a result of total thyroidectomy, affecting between 10,200 and 17,300 patients. This is the most frequent complication after a total thyroidectomy.
Its frequency varies greatly in the literature, from 0.3% to 68%2,7,10-15. It is difficult to interpret and compare the results of the various studies due to the lack of international agreement. Recently, the SEORL-CCC, together with the SEEN, have reached a consensus where they provide more specific definitions, and also recommendations to reduce hypoparathyroidism16.
Given its high incidence, studying the predictive factors that help identify those patients with a high risk of postoperative hypocalcaemia assumes considerable importance. The main objective of this study is to analyze the biochemical, surgical and demographic factors related to an increased risk of immediate postoperative hypocalcaemia.
MATERIAL AND METHODS
This retrospective study of 297 patients who underwent total thyroidectomy was carried out from January 2011 to December 2018 in a tertiary care hospital.
All patients who underwent total thyroidectomy were included, both in one and in two stages, and regardless of the reason for the indication. All were referred from the Endocrinology Service of the center itself after a complete study. In each of them, the usual protocol was performed by the ENT service: complete history, cervical palpation and laryngoscopy to assess the mobility of the vocal cords.
In this study, post-op hypocalcaemia was defined as serum calcium <8.5 mg/dL and/or appearance of symptoms typical of hypocalcaemia. Hypoparathyroidism is defined as the presence of hypocalcaemia with low or inadequately normal PTH levels. This is deemed permanent if this situation lasts more than 12 months.
Preoperative, intraoperative, and post-op demographic, clinical and biochemical data were collected from each patient through medical records. Data on the surgical reports were collected, including the number of surgeries performed (1 or 2 times), the number of observed and spared parathyroid glands and also the autotransplanted parathyroid glands, the presence of intrathoracic thyroid extension, and the association of other surgical procedures with the thyroidectomy, such as lymph node dissections.
Among the biochemical parameters collected, the following stand out: PTH, albumin-corrected calcium and preoperative vitamin D; postoperative phosphorus, albumin-corrected postoperative calcium at 6 and 24 hours, and postoperative PTH at 24 hours after total thyroidectomy. Finally, in terms of factors related to the patient and their disease, we include age, gender, Graves' disease or carcinoma confirmed by pathological anatomy.
The autoanalyzer used to determine PTH levels was the Roche-Hitachi Cobas® 6000 Series system. The normal range for this test is between 15 and 65 pg/mL. Spectrophotometry was used to determine both serum calcium and vitamin D.
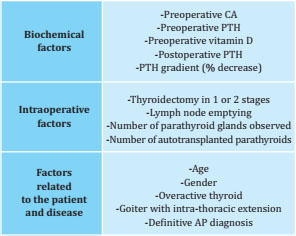
Data analysis was carried out with R software version 3.6.2. All variables were subjected to a normality test. The Student's t test compared continuous parametric variables, the Mann-Whitney U test for non-parametric continuous variables and the χ2 test for proportions, considering a value of p<0.05 as significant. The data are presented in percentages and averages with their respective standard deviations and ranges. For the analysis of the effect size based on differences between groups, Cohen's d and the Odds Ratio (OR) were used. To simplify the graphic presentation of the data, tables and histograms have been used. A table is shown with the risk factors analyzed (table 1).
RESULTS
This study included 297 patients who underwent total thyroidectomy, the vast majority being women (81.5%), with a mean age of 54.2±14.2 years [17-90]. Forty-four patients underwent a two-stage total thyroidectomy, and in addition, 40 of them underwent cervical dissection. More than half of the procedures were performed for benign disease (64%), and of these, 32% with preoperative thyroid hyperfunction (52 with thyrotoxicosis and 43 with sub-clinical hyperthyroidism). Of the patients included in the present sample, 16 had a documented radiological image of intrathoracic goiter. Of those with diagnostic confirmation of cancer (33%), 92 cases corresponded to the differentiated subtype and 6 cases to medullary carcinoma.
Statistical analysis showed significant differences between hypocalcaemia and age (p=0.04), Graves' disease (p=0.04), carcinoma confirmed by pathology (p=0.04), thyroidectomy in two times (p=0.00), the number of transplanted parathyroids (p=0.00), preoperative and postoperative PTH at 24h (p=0.03 and p=0.00) and the PTH gradient (p=0.00). In contrast, no significant relationship was shown with gender (p=0.22), preoperative calcium level (p=0.54), preoperative vitamin D (p=0.24), goiter with intrathoracic extension (p=0.61), cervical lymph node dissection (p=0.33) or the number of parathyroid glands observed during surgery (p=0.99) (table 2).
Table 2. Summary of the statistical analysis of the factors in relation to immediate hypocalcaemia.
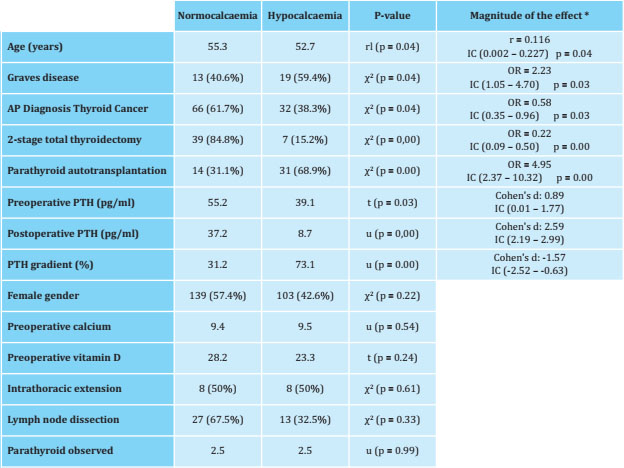
*OR calculated on the rate of overall postoperative hypocalcaemia.
lr: linear regression; r: Pearson's correlation coefficient; t: T-Student test; u: Mann-Whitney U test; χ2: Chi2 test.
A total of 187 complications related to thyroid surgery were recorded in 154 patients. With great difference, the most frequent complication was hypoparathyroidism with 65%.
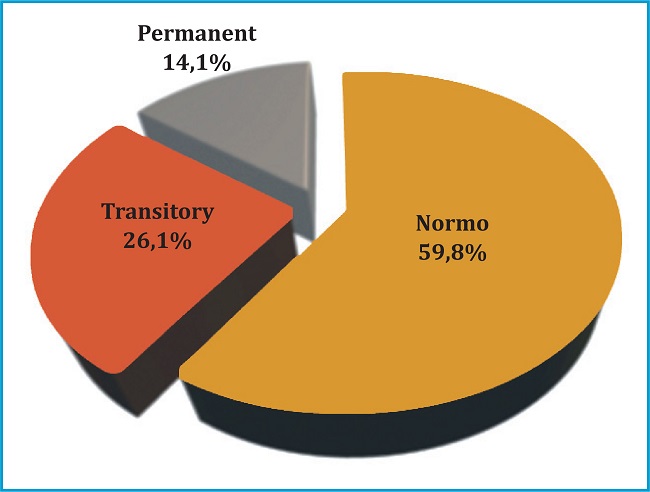
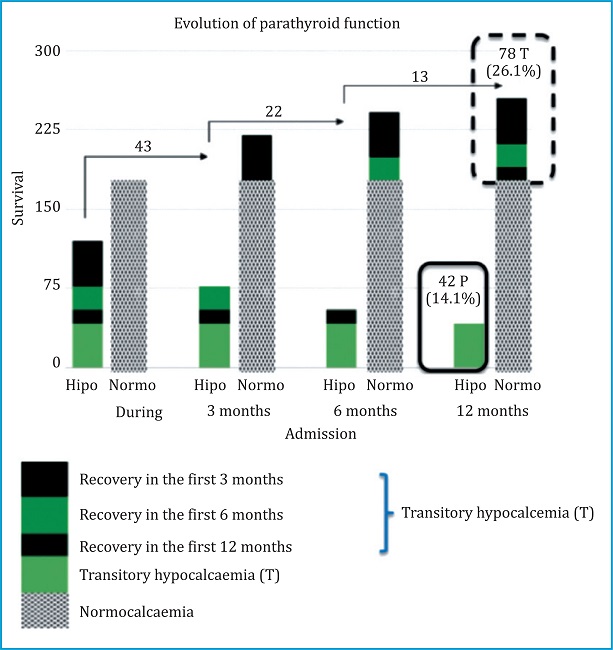
40.2% of the patients who underwent total thyroidectomy developed hypocalcaemia in the postoperative period (figure 1). Of the patients with hypocalcaemia, 43 recovered their calcemia levels in the first 3 months, 22 in the following 3 months, and finally 13 after the sixth month of follow-up. Therefore, the total number of patients with transient hypocalcemia was 78 cases (26.1%) and the remaining patients who did not recover after 12 months of follow-up were classified as permanent hypocalcemia with a total of 42 cases (14.1%). ) (figure 2). No case of hypocalcaemia could be attributed to hungry bone syndrome.
DISCUSSION
According to the latest data provided by the Spanish Thyroid Cancer Association (AECAT), 75% of cases of hypoparathyroidism in Spain occur as a result of total thyroidectomy, affecting between 10,200 and 17,300 patients. This is the most frequent complication after a total thyroidectomy.
No factor alone predicts post-total thyroidectomy hypocalcemia accurately. Rather, it is about several factors that interact with each other, with a high probability of jointly predicting hypocalcaemia. For this reason, there is a great discrepancy in the literature. Some authors propose as possible risk factors the fact of completing a total thyroidectomy in a patient previously operated on a hemithyroidectomy, due to the distortion of the anatomy and the difficult recognition of the parathyroids14,17.
The prevalence of transient hypocalcaemia, that is, when it lasts less than 6-12 months, ranges between 10% and 40%. The permanent one, present beyond 6-12 months, varies from 0.12% to 16.2%, according to the literature1,3,4,14,18. Diez et al. published in 2019 a prevalence of hypoparathyroidism at discharge after total thyroidectomy of 48%, of which 52.5% recovered in the first 3-6 months12. In the present study, the total hypocalcaemia rate was 40.2%, with 54.2% recovering parathyroid function in the first 6 months. Both the transitory (26.1%) and the permanent (14.1%) conform to what is described in the international literature. Thus, studying the predictive factors that help identify those patients with a high risk of post-op hypoparathyroidism is very importance.
The average PTH at 24 hours was 24.6±17.9 pg/mL [3-78]. Patients with postoperative hypocalcaemia had lower mean PTH levels at 24h (8.7 pg/mL) compared to normocalcemic patients, who obtained a mean of 37.2 pg/mL calcemic patients, who obtained a mean of 37.2 pg/mL (p=0.00). PTH has been extensively studied as a predictor of hypocalcaemia in the literature. Some studies propose the gradient or percentage of decrease in the PTH level from the preoperative to the postoperative period, while others propose a single intra‐operative or postoperative PTH level some time after surgery. In the present study, the largest effect size is presented by postoperative PTH (Cohen's d: 2.59), with the additional advantage of costing less, since it does not require preoperative PTH.
Regarding total hemi‐thyroidectomy in a second stage, in the present study the relationship found is protective, so that those patients operated on in a single stage present a higher probability (4.55 times greater) of transient hypocalcaemia (p=0.00), coinciding with the study by Díez12. There is no significant relationship between total thyroidectomy in a second surgical time and permanent hypocalcaemia (p=0.29). This fact could be explained by the reversible parathyroid edema and devascularization caused by the surgery, allowing a second surgical time for recovery.
On the other hand, surgery for thyroid cancer17,19,20 or for Graves' disease17,20 and associated cervical dissection14 have also been proposed as possible risk factors. In contrast, other studies have not found a significant association11. In the study by Díez et al., the presence of lymph node metastases was a negative predictor of parathyroid recovery in patients with thyroid cancer21.
In our study, a significant protective relationship with pathology‐confirmed carcinoma is found, probably because cases suspected of malignancy are handled by a more experienced surgical team. As for Graves' disease, there is a significant direct relationship, probably due to fibrosis due to thyroiditis, with these patients presenting 2.23 times more risk of hypocalcaemia. On the other hand, there is no significant relationship with lymph node drainage.
It is reasonable to think that the fact of preserving at least one parathyroid gland could maintain normal function, and even if it decreased, it could be a transient hypocalcaemia22,23. In various studies, however, including the present study, it has not been possible to demonstrate significantly that the observation and preservation of more than two parathyroids prevents hypocalcaemia14,24.
In some studies, autotransplantation of removed glands could reduce the incidence of hypocalcaemia11. However, in the present study this association is inverse, so that in those patients who have autotransplanted one or more glands, they had a higher risk of hypocalcaemia at discharge (4.95 times more), but this relationship was not significant in terms of permanent hypocalcaemia. This concurs with other studies showing that parathyroid autotransplantation does not guarantee recovery of parathyroid function7,12,18,24.
CONCLUSIONS
Given the increasing number of thyroid surgeries world‐wide, hypocalcaemia is assuming increasing importance and increasing the burden of disease in the population. A more precise understanding of the risk factors would help to better predict the risk of postoperative hypocalcaemia.
The factors directly related to postoperative hypocalcaemia were age, Graves' disease, number of transplanted parathyroids PTH preoperative and postoperative at 24 h and the PTH gradient; meanwhile he carcinoma confirmed by pathology and two‐stage thyroidectomy were inversely related.
Bibliografía
1 Filho EBY, Machry RV, Mesquita R, Scheffel RS, Maia AL. The timing of parathyroid hormone measurement defines the cut-off values to accurately predict postoperative hypocalcemia: a prospective study. Endocrine. 2018;61(2). doi: 10.1007/s12020-018-1601-9. [ Links ]
2 Pǎduraru DN, Ion D, Carsote M, Andronic O, Bolocan A. Post-thyroidectomy hypocalcemia - Risk factors and management. Chir. 2019;114(6). doi: 10.21614/chirurgia.114.6.704. [ Links ]
3 Mordojovich R G, Lavín G M, Ávalos J N. Medición de niveles de parathormona como predictor de hipocalcemia sintomática en el post-operatorio precoz de tiroidectomía total. Rev Chil cirugía. 2015;67(2). doi: 10.4067/s071840262015000200006. [ Links ]
4 Coimbra C, Monteiro F, Oliveira P, Ribeiro L, de Almeida MG, Condé A. Hipoparatiroidismo tras tiroidectomía: factores predictivos. Acta Otorrinolaringol Esp. 2017;68(2):106-111. doi: 10.1016/j.otorri.2016.06.008. [ Links ]
5 Papanastasiou A, Sapalidis K, Mantalobas S, et al. Design of a predictive score to assess the risk of developing hypocalcemia after total thyroidectomy. A retrospective study. Int J Gen Med. 2019;12. doi: 10.2147/IJGM.S204795. [ Links ]
6 Aluffi P, Aina E, Bagnati T, Toso A, Pia F. Factores pronósticos de hipoparatiroidismo definitivo tras tiroidectomía total. Acta Otorrinolaringol Esp. 2008;59(7). doi: 10.1016/S0001-6519(08)75550-X. [ Links ]
7 Eismontas V, Slepavicius A, Janusonis V, et al. Predictors of postoperative hypocalcemia occurring after a total thyroidectomy: Results of prospective multicenter study. BMC Surg. 2018;18(1). doi: 10.1186/s12893018-0387-2. [ Links ]
8 Díez Alonso M, Sánchez López JD, Sánchez-Seco Peña MI, et al. Serum PTH levels as a predictive factor of hypocalcaemia after total thyroidectomy. Cirugía Española (English Ed. 2009;85(2). doi: 10.1016/s2173-5077(09)70122-x. [ Links ]
9 Reddy AC, Chand G, Sabaretnam M, et al. Prospective evaluation of intra-operative quick parathyroid hormone assay as an early predictor of post thyroidectomy hypocalcaemia. Int J Surg. 2016;34. doi: 10.1016/j.ijsu.2016.08.010. [ Links ]
10 Mazotas IG, Wang TS. The role and timing of parathyroid hormone determination after total thyroidectomy. Gland Surg. 2017;6. doi: 10.21037/gs.2017.09.06. [ Links ]
11 Lombardi CP, Raffaelli M, Princi P, et al. Early prediction of postthyroidectomy hypocalcemia by one single iPTH measurement. Surgery. 2004;136(6). doi: 10.1016/j.surg.2004.06.053. [ Links ]
12 Díez JJ, Anda E, Sastre J, et al. Prevalence and risk factors for hypoparathyroidism following total thyroidectomy in Spain: a multicentric and nationwide retrospective analysis. Endocrine. 2019;66(2). doi: 10.1007/s12020-01902014-8. [ Links ]
13 Barquero-Melchor H, Delgado-Rodríguez MJ, Juantá-Castro J. Hipocalcemia e hipoparatiroidismo post-tiroidectomía TT - Hypocalcemia and hypoparathyroidism after thyroidectomy. Acta Med Costarric. 2015;57(4). [ Links ]
14 Grodski S, Farrell S. Early postoperative PTH levels as a predictor of hypocalcaemia and facilitating safe early discharge after total thyroidectomy. Asian J Surg. 2007;30(3). doi: 10.1016/S1015-9584(08)60019-6. [ Links ]
15 Kamer E, Unalp HR, Erbil Y, Akguner T, Issever H, Tarcan E. Early prediction of hypocalcemia after thyroidectomy by parathormone measurement in surgical site irrigation fluid. Int J Surg. 2009;7(5). doi: 10.1016/j.ijsu.2009.07.006. [ Links ]
16 Castro A, Oleaga A, Parente Arias P, Paja M, Gil Carcedo E, Álvarez Escolá C. Resumen ejecutivo del documento de consenso SEORL CCC-SEEN sobre hipoparatiroidismo postiroidectomía. Endocrinol Diabetes y Nutr. 2019;66(7). doi: 10.1016/j.endinu.2019.03.015. [ Links ]
17 Scurry WC, Beus KS, Hollenbeak CS, Stack BC. Perioperative parathyroid hormone assay for diagnosis and management of postthyroidectomy hypocalcemia. Laryngoscope. 2005;115(8): 1362-1366. doi: 10.1097/01.MLG.0000166699.23264.37. [ Links ]
18 Edafe O, Balasubramanian SP. Incidence, prevalence and risk factors for post-surgical hypocalcaemia and hypoparathyroidism. Gland Surg. 2017;6. doi:10.21037/gs.2017.09.03. [ Links ]
19 Payne RJ, Tewfik MA, Hier MP, et al. Benefits resulting from 1- and 6-hour parathyroid hormone and calcium levels after thyroidectomy. Otolaryngol - Head Neck Surg. 2005;133(3):386-390. doi: 10.1016/j.otohns.2005.02.021. [ Links ]
20 Warren FM, Andersen PE, Wax MK, Cohen JI. Intraoperative parathyroid hormone levels in thyroid and parathyroid surgery. Laryngoscope. 2002;112(10). doi: 10.1097/00005537200210000-00031. [ Links ]
21 JJ D, E A, J S, et al. Recovery of parathyroid function in patients with thyroid cancer treated by total thyroidectomy: An analysis of 685 patients with hypoparathyroidism at discharge of surgery. Endocrinol diabetes y Nutr. 2021;68(6). doi: 10.1016/J.ENDIEN.2021.10.009. [ Links ]
22 Edafe O, Antakia R, Laskar N, Uttley L, Balasubramanian SP. Systematic review and meta-analysis of predictors of post-thyroidectomy hypocalcaemia. Br J Surg. 2014;101(4):307-320. doi: 10.1002/BJS.9384. [ Links ]
23 Lorente-Poch L, Sancho JJ, Ruiz S, Sitges-Serra A. Importance of in situ preservation of parathyroid glands during total thyroidectomy. Br J Surg. 2015;102(4). doi:10.1002/BJS.9676. [ Links ]
24 Kihara M, Miyauchi A, Kontani K, Yamauchi A, Yokomise H. Recovery of parathyroid function after total thyroidectomy: long-term follow-up study. ANZ J Surg. 2005;75(7):532-536. doi: 10.1111/J.1445-2197.2005.03435.X. [ Links ]
Received: April 24, 2022; Accepted: October 11, 2022











 texto en
texto en