Introduction
Telemedicine is defined as the provision of health services (where distance is a determining factor) by healthcare professionals, who use information and communication technologies to exchange information to diagnose, prevent and treat diseases, and for research, evaluation and ongoing training of healthcare professionals, the aim being to improve the health of the community1,2.
Teledermatology consists of the application of new technologies in the treatment of skin diseases. The use of this treatment modality in prisons enables inmates to be diagnosed and treated without having to transfer them to a hospital, thus avoiding problems of security and the costs associated with displacement. It also helps to preserve inmates' privacy, since it prevents situations in which they have to appear in public spaces handcuffed and under guard3-8. Other advantages of this type of healthcare is that it drastically reduces waiting times for diagnosis and treatment plans, and is also useful for training medical personnel who receive the response from the teleconsultation.
The aim of this study is to analyse the capacity of teledermatology to resolve health issues at a prison that is some distance away from the reference hospital.
Material and method
A retrospective observational study was carried out the Castellón II-Albocàsser Prison, which lies within the healthcare area covered by the Castellón University General Hospital (Health Department of Castelló). It is located in the municipality of Albocàsser, 58 km away from the hospital. The prison has 1,214 cells, with a capacity for 1,704 inmates.
The research project was approved by the medical research ethics committee of the Castellón University General Hospital.
The study population was made up of inmates at the Castelló II-Albocàsser Prison who had undergone some type of dermatological consultation at the Castellón General Hospital in a period of 18 months (dating from when the prison teledermatology commenced on 30 May 2019, to 31 December 2020).
The indirect store and forward teledermatology modality was used for all the consultations9. The nursing personnel at the prison took panoramic and detailed images of the relevant skin lesions. The images were sent to the hospital's electronic clinical records along with the referral carried out by the prison medical services and issued to the hospital dermatology service.
One requirement was that the both the consultation and the response should contain a minimum amount of information agreed on by both parties to provide the necessary clinical data. The response from the dermatology service was sent in deferred transmission modality via the electronic clinical record. The response included the diagnostic approach, the treatment plan, the need for subsequent online or face-to-face check-ups and requests to the medical staff or patient for additional information, if necessary.
The following variables in the clinical record were collected, and the patient's data was anonymised: sex, age, number of completed teledermatological consultations, diagnosis, diagnostic group, type of consultation, complete treatment plan with the teleconsultation, request for subsequent face-to-face consultation and time required for responding to the referral.
The teledermatology service's capacity to resolve issues was assessed according to its ability to establish a diagnostic suspicion, treatment plan and the absence of any need for subsequent face-to-face consultations.
Results
83.8% (31 patients) underwent referral, while the remaining 16.2% (six patients), underwent two. Out of the six patients who received a second referral, two requested it for different reasons, one to recommend a treatment that could not be established in the first visit and another to make changes in the previously recommended medication.
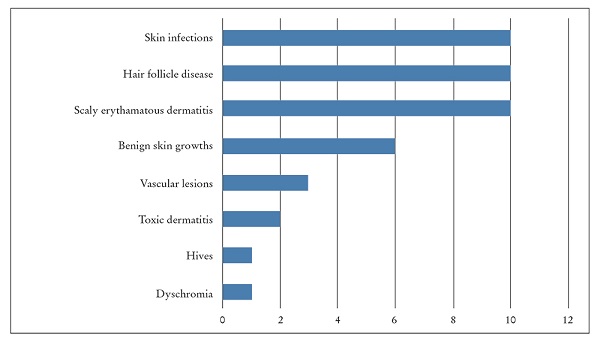
The reasons for the consultation can be seen in Figure 1. The most frequent ones were: skin infections (23.3%, ten consultations), diseases of the hair follicles (23.3%, ten consultations), scaly erythematous dermatitis (23.3%, ten consultations), benign skin growth (14%, six consultations), vascular lesion (7%, three consultations), toxic dermatitis (4.4%, two consultations), dyschromias (2.3%, one consultation) and hives (2.3%, one consultation).
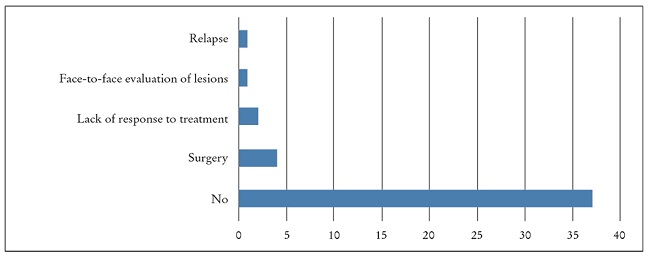
A diagnosis and complete treatment plan were established in 86% of the consultations. 18.6% of the referrals required a face-to-face consultation: one for an assessment of the skin lesions before establishing treatment, four for surgery, two for evaluation due to a lack of response and one for evaluation after a relapse caused by an interruption of the treatment (Figure 2).
Out of the total of 43 teleconsultations, a treatment plan could not be provided for the patient in 14% of the cases (six teleconsultations). A second teleconsultation was required in one of the cases, where necessary data about the patient was provided to enable treatment to be established. Another patient required a subsequent face-to-face consultation to assess the lesions and decide on the approach to be taken. The other four required face-to-face treatment (curettage, surgical excision). On the other hand, complete treatment was established in the other 86% (37) referrals, regardless of the subsequent response to same.
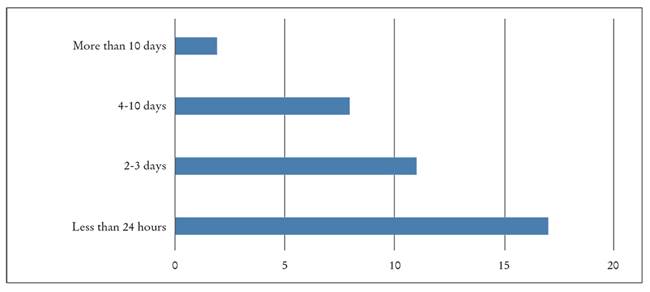
The delay in responding to referrals found in this study was three days or less in 73% of the first consultations. Only three cases showed a delays of more than 20 days in responding to the referral, caused by issues with the data dispatch channels (Figure 3).
Discussion
Previous research has studied the usefulness of telemedicine in prisons, focusing on the financial savings offered by this healthcare modality. Although the most widely studied specialities are psychiatry and infectious diseases, the field is now being opened up include to others such as se dermatology and X-ray diagnosis. Other studies have highlighted other advantages of telemedicine, such as humanising healthcare for prison inmates and the high levels of user satisfaction7.
As regards the type of consultation, the store and forward modality appears to be the most commonly selected one for referrals, with structured case histories and image saving, instead of synchronous modalities with videoconferences. The main disadvantages of this particular method are poor image quality and the need to coordinate times for the patient, the medical staff carrying out the referral and the staff who respond to it.
In a study carried out in France on men of a mean age of 35 years, acne and atopic dermatitis were the main reasons for consultation4. Furthermore, 85% of the users obtained a complete treatment plan. These results are very similar to the ones obtained in this study, with a percentage of 86%. Subsequent face-toface visits were only required in 3% of the cases. This result is quite different from the findings in this study, where 18.6% of the teleconsultations required a subsequent face-to-face consultation. This difference may be due to the inclusion of surgical treatment as a face-to-face consultation.
Our conclusion is that teledermatology in prisons appears to help in resolving many of the consultations about skin pathologies without the need for face-to-face consultations. Shared access to an electronic clinical history is needed to enable information to flow effectively. Future studies should include the satisfaction levels of medical personnel and patients with medical care provided via teledermatology.