INTRODUCTION
Up to 70% of treatment decisions rely mainly on laboratory testing. As such, clinical laboratories are recognized as integral in ensuring the accuracy of disease diagnosis, management, and mentoring [1, 2], and maintaining laboratory quality and test availability for every medical testing request is of interest. In addition, ensuring the appropriateness of requested testing is essential. “Necessary or appropriate laboratory testing means the procedure of requesting tests at the right time for the right time using the right methods with knowing of the right cost” [3, 4]. Unnecessarily laboratory tests constitute approximately 10 to 70%. Thus, contribute to inaccurate diagnosis and treatment [5].
Zhi et al. determined inappropriate testing to occur in two forms, overutilization and underutilization, where overutilization is the ordering of tests not indicated and underutilization the failure to order indicated tests [6]. Several studies have revealed that overutilization constitutes approximately 20% of requested laboratory testing [7, 8], and both overutilization and underutilization can be physically and economically harmful as well as life-threatening to patients. For instance, overutilization could result in unnecessary blood sample collection, elevated expense, and inaccurate test results, while underutilization could lead to serious consequences including morbidity due to inadequate or late laboratory testing requests [6]. Overutilization in particular is of concern in numerous countries. The “Choosing Wisely” campaign began in 2014 in the United States, followed by Canada, to encourage physicians and patients to discuss inappropriate tests, methods, and disease management. This campaign has since been adopted by many health care providers in several countries [9].
Overutilization of laboratory testing is influenced by numerous factors, including the experience and specialty of the practitioners [10]. Experienced physicians are assumed to be aware of and familiar with what laboratory tests are best and available for patients. Conversely, less experienced physicians or residents could consume laboratory resources when over-requesting inappropriate laboratory testing [7, 11]. In particular, university and internship student physicians were found to be more often involved in inappropriate requesting of laboratory tests because they are more prone to fear of missing the right diagnosis [10]. Improving and encouraging the proper utilization of laboratory testing was in that case achieved by implementing education, auditing, and use of a highly computerized restricted ordering system [10]. It has been shown more generally that improving the awareness or alertness of doctors concerning factors that contribute to overutilization leads to control of inappropriate testing requests [12]. In a study of one tertiary referral center in Saudi Arabia, Morris et al. reported an increase in the demand for clinical laboratory services despite the fixed budget for such services [13]. They suggested that the demands could be managed by three effective factors: strong medical leadership, coaching, and education [13]. Overall, intervention is necessary to restrict the overutilization of laboratory services by unnecessary tests; towards this end, it is of interest to first assess the extent of inappropriate testing currently requested by physicians.
The present study thus aimed to evaluate the demands for inappropriate laboratory testing by physicians in Saudi Arabia from a different direction, namely measuring the satisfaction of medical laboratory professionals toward testing requests.
METHODS
STUDY DESIGN AND PARTICIPANTS
A list of questionnaires was designed and reviewed by medical academic/researcher staff at the Department of Medical Laboratory Sciences, King Khalid University. In the interest of better understanding and evaluation, survey questions were circulated to participants in the Arabic language and then translated into English. A valid and simple form was generated using Google Forms, a software utility for survey administration. A link including all questions was distributed to medical laboratory professionals throughout Saudi Arabia. The survey form started with a short description of the study, including the topic and objectives. The form constituted three different sections, respectively concerning participant general information (gender and duration of employment), knowledge, and attitudes. The latter two were assessed by asking a straightforward question concerning the targeted factor and another on the most suitable reaction to the factor.
To examine the extent of participant satisfaction concerning laboratory testing requests, the survey was divided into two parts. The first examined participant knowledge concerning inappropriate laboratory testing and consisted of the definition of unnecessary laboratory testing and its impact on laboratory resources. The second constituted an assessment of the proper attitude among clinical laboratory members for preserving laboratory supplies.
A total of twelve questions were used to assess the knowledge and attitudes of the participants. Participants were informed that participation is not compulsory, and that they have the right to not participate or to withdraw even after participating. The study aimed to receive a minimum of 250 responses.
DATA ANALYSIS
Google form, a website data collection, was used for rapid and accurate data collection and management. The website analyzed the data and displayed it as frequencies and percentages. The analyzed data were then entered into GraphPad Prism (GraphPad Prism version 9.00 for Mac, GraphPad Software, San Diego CA) for further analysis.
RESULTS
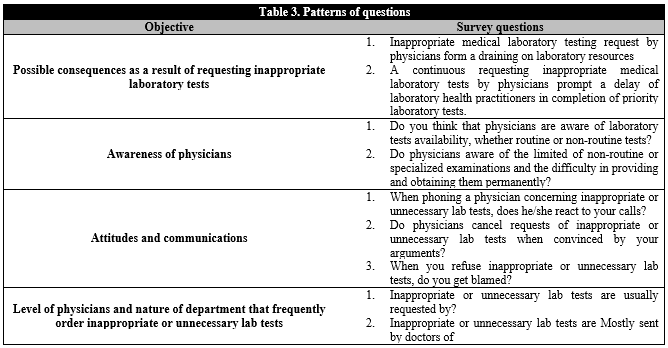
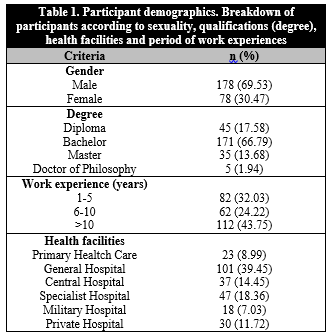
The survey used in this study was designed to determine factors that may influence laboratory resources and distributed to clinical laboratory professionals all over Saudi Arabia. The final study population constituted a total of 256 participants, who were of both genders and represented diverse qualifications, experiences, and types of hospitals. The proportion of male participants was greater than that of females, comprising over two-thirds the total (Male: n=178, 69.5%; Female: n=78, 30.5%; Table 1). The qualifications of the subjects were varied and ranged from a diploma to a Ph.D. (Table 1). The distribution of health facilities and job experience among participants is depicted in Table 1.
Table 1. Participant demographics. Breakdown of participants according to sexuality, qualifications (degree), health facilities and period of work experiences
Participants' definition of inappropriate laboratory testing was determined by means of three different questions (Table 2). The overwhelming majority of participants (89.80%) agreed that inappropriate laboratory testing includes tests that physicians consistently request for every patient, regardless of any individual patient's condition and needs (Table 2). In addition, nearly all participants (85.81%) agreed that inappropriate medical laboratory testing includes physicians classifying a request as urgent when it is not otherwise such, which can delay high-priority tests for other patients (Table 2). Meanwhile, only 65.20% agreed that inappropriate medical laboratory testing includes requests for non-routine testing (Table 2).
Table 2. Definition of Inappropriate medical laboratory testing by medical laboratory practitioners (n=256)
We next examined the potential impact of inappropriate laboratory testing by proposing two possible consequences, the draining of laboratory resources and the delayed completion of priority laboratory tests (Table 3, objective 1). More than 90% of participants agreed on the impact of inappropriate laboratory testing on clinical laboratory resources and test performance (Figure 1).
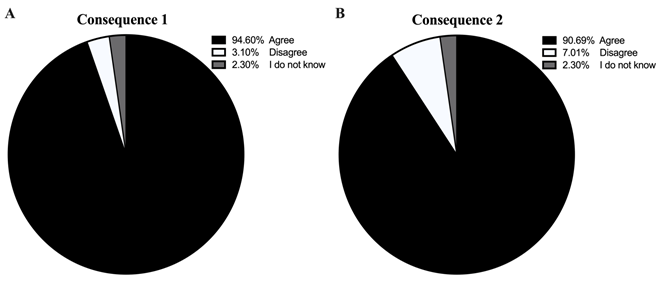
Figure 1. Impacts of unnecessary tests. Charts indicate participant responses to the possible consequences of requesting inappropriate laboratory testing on: A) clinical laboratory resources and B) test performance.
We further explored physician communications to clinical laboratory professionals concerning test availability, awareness of limitations to the supply of some reagents, and reactions when laboratory staff refused to implement unnecessary tests due to such limitations (Table 3, objectives 2 and 3). Approximately half of participants reported physicians as being aware of available tests in the laboratory (Figure 2); however, the same percentage expressed that physicians are not aware of limitations concerning supplies for specialized laboratory tests (Figure 2B). Finally, there was some contrast in participant responses concerning the attitude of physicians upon test refusal (Figure 3). However, the majority were less satisfied with the reactions of some physicians and were criticized when refusing to perform inappropriate tests (Figure 3).
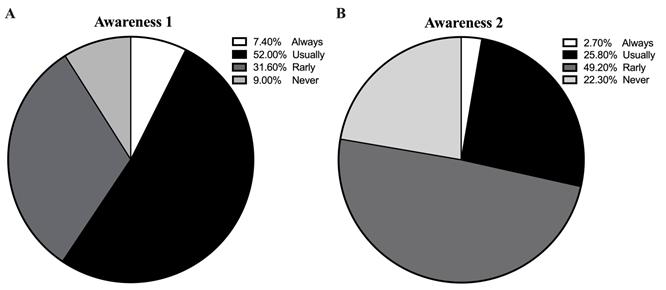
Figure 2. Physician awareness of test resources. Charts indicate participant responses concerning the awareness of physicians toward A) test availability and B) limitations on laboratory testing.
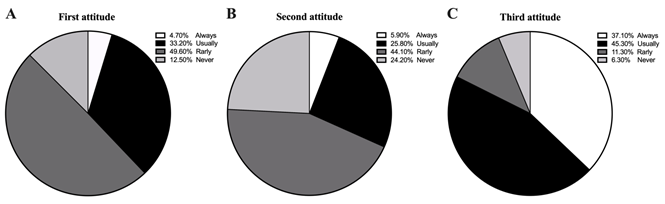
Figure 3. Communication between physicians and clinical laboratory professionals. Charts indicate participant responses concerning the reactions of physicians when an action is taken by clinical laboratory professionals.
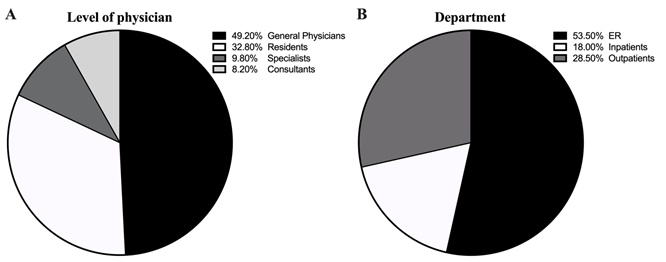
Besides, we were highly interested in determining the types of physicians and departments who contributed most to requests for inappropriate laboratory testing (Table 3, objective 4). Most participants admitted that unnecessary tests were almost all requested by general and resident physicians (Figure 4), while emergency rooms were the leading requestors of inappropriate laboratory testing as stated in Figure 4.
DISCUSSION
Managing the material of health-care providers is critical to providing high-quality care [14]. Diagnostic laboratories are regarded as a core department in the health sector, and maintaining lab resources is therefore of interest [15]. In particular, the management of laboratory resources in hospitals that provide laboratory tests free-of-charge to patients supported by governments is critical for improving laboratory utilization. Additionally, protecting patients' budgets against extra bills for unnecessary laboratory tests in the private sector is also of interest. This survey was designed to determine the current satisfaction of clinical laboratory professionals about laboratory test requests received from physicians as their perceptions are relevant to providing high-quality health services via providing fully equipped laboratories with a stock of routine and non-routine tests. The participants included male and female employees of varying qualifications and experiences from primary, general, specialized, and military health care sectors as well as private health services. This diversity of participants may contribute to a better description of the extent of satisfaction of laboratory professionals in different levels of the health care system.
To define the correct definition of inappropriate laboratory testing as perceived by laboratory practitioners, three different definitions were proposed. Our data showed that the majority of participants define inappropriate laboratory testing as testing requested persistently by physicians for every patient, regardless of any individual patient's condition and needs. This definition was in line with the previously described definition that inappropriate laboratory testing constitutes prescribing laboratory tests at will regardless of guidelines [3].
The survey also highlighted participants' views of the consequences of inappropriate laboratory testing on laboratory resources. Participants agreed that overutilization has negative impacts on laboratory resources. One such impact is the draining of supplies, consistent with the study conducted by Cadamuro et al. [15]. In addition, inappropriate laboratory testing contributes to interruption of timely and needed care, particularly for cases in which testing is critical, as confirmed by almost all participants. The impact of inappropriate laboratory testing is thus not just an issue of cost, but also of sustainability and providing equal health care [3].
The study also allowed for the concomitant evaluation of physicians' perceived knowledge about the availability of both routine and non-routine tests. Such knowledge could exist as a list of the available tests provided by a hospital or be estimated via communication with clinical laboratory professionals. Participant responses indicated a lack of physician knowledge concerning test availability, but especially so regarding the limitations surrounding non-routine or specialized examinations. It is known that overutilization of laboratory tests is highly prevalent, and that such overutilization may occur due to several factors involving physician awareness, knowledge, and insecurity [7]. Overutilization of laboratory testing has also been previously attributed to the culture of the health system and to lack of cost transparency [11]. In addition, concern regarding providing the right diagnosis for treatment management could contribute to overutilization [7]. Generally, inappropriate laboratory testing requests originate with physicians having less experience and knowledge. Recently, several studies determined that residents are responsible for the majority of inappropriate laboratory test orders [7, 11, 16]. This is consistent with participant responses, which revealed that general physicians and residents request the majority of inappropriate laboratory testing, with the emergency department bearing the brunt of the blame.
Eventually, the survey investigated the attitudes of clinical laboratory practitioners toward overutilization of laboratory tests. The results revealed a lack of communication between physicians and laboratories concerning patient condition and thus actual need for tests. To overcome such issues, Cadamuro et al. suggested implementing demand management schemes, which incorporate several strategies including algorithms, education, and more that could help to manage ordering behaviour [15]. However, such strategies would not apply to every health care center and medical condition.
Our study adds to the literature that requests for inappropriate laboratory testing are common, particularly from junior physicians. Most studies that have particularly focused on requests for inappropriate laboratory tests aim to reduce the prevalence of and manage such requests, in addition to preserving resources so as to provide them to the right patient at the right time. Education interventions, understanding cost-effectiveness of tests, and other strategies assist in managing inappropriate laboratory testing. The present study has limitations, including that exact numbers of inappropriate laboratory testing orders in a period of time were not quantified, and that the evaluation was only made with consideration of clinical laboratory practitioners and their perceptions.