INTRODUCTION
The anatomy of the first vertebra, namely atlas, has significant clinical implications [1]. Atlas is situated between the occipital bone and the second cervical vertebra (axis). It is one of the main points of head movement, due to joints, and serves as an attachment for several muscles [2]. Anatomically it is not a typical vertebra due to its shape and absence of body and spinous process. Nevertheless, its function and variations of development are important in clinical settings.
Most congenital anomalies of the vertebra are diagnosed incidentally during imaging investigations and are often associated with cervical spine anomalies. Congenital clefts and other developmental anomalies of the atlas vertebra are rare but may present as a diagnostic dilemma especially in neck pain, radiculopathy, neck mass, and after trauma [3, 4]. Particularly, differentiation of developmental variants of the atlas from the burst fracture of Jefferson (fracture into two, three or four segments) is essential to prevent unnecessary medical intervention [5].
We report an anatomical case and analysis of the literature about posterior arch clefts of atlas.
CASE REPORT
During routine examination of newly prepared osteology specimens for anatomical classes, we observed an unusual structure of the atlas. Only one case (1,82%) was encountered out of 55 first vertebrae. The anteroposterior length of the atlas was 40.2 mm and the anteroposterior length of the vertebral canal was 37.4 mm. The transverse dimension of the vertebra was 51.3 mm and of the vertebral canal 39.0 mm. The posterior hemiarches were completely separated and had a 5 mm defect. Apart from the posterior midline cleft there were no other defects (Figure 1). The defect is classified as type A based on Currarino classification (Figure 2) [6].
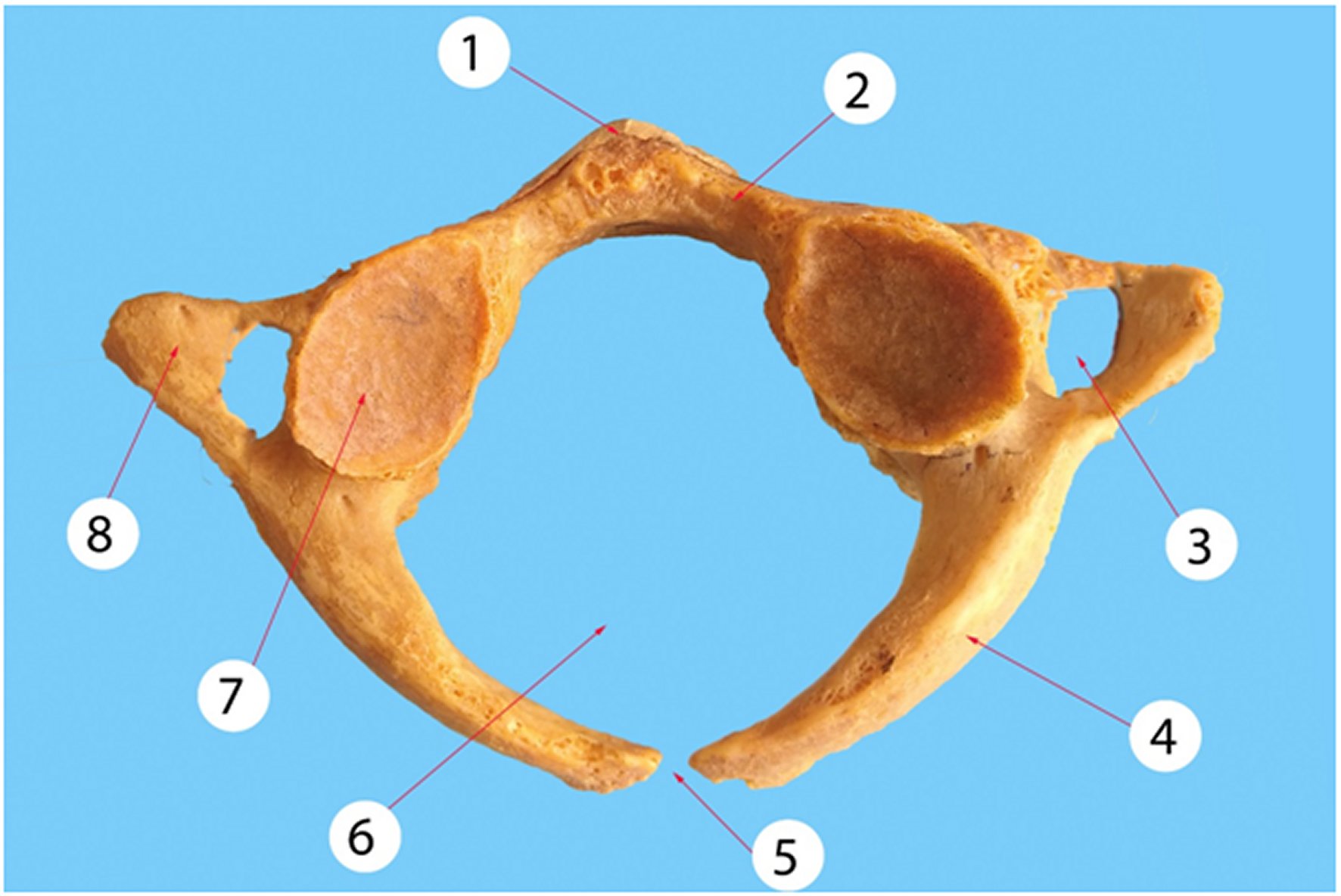
Figure 1. Posterior midline cleft.1: anterior tubercle; 2: anterior arch; 3: foramen transversarium; 4: posterior arch; 5: posterior midline cleft; 6: vertebral foramen; 7: superior articular surface; 8: transverse process.
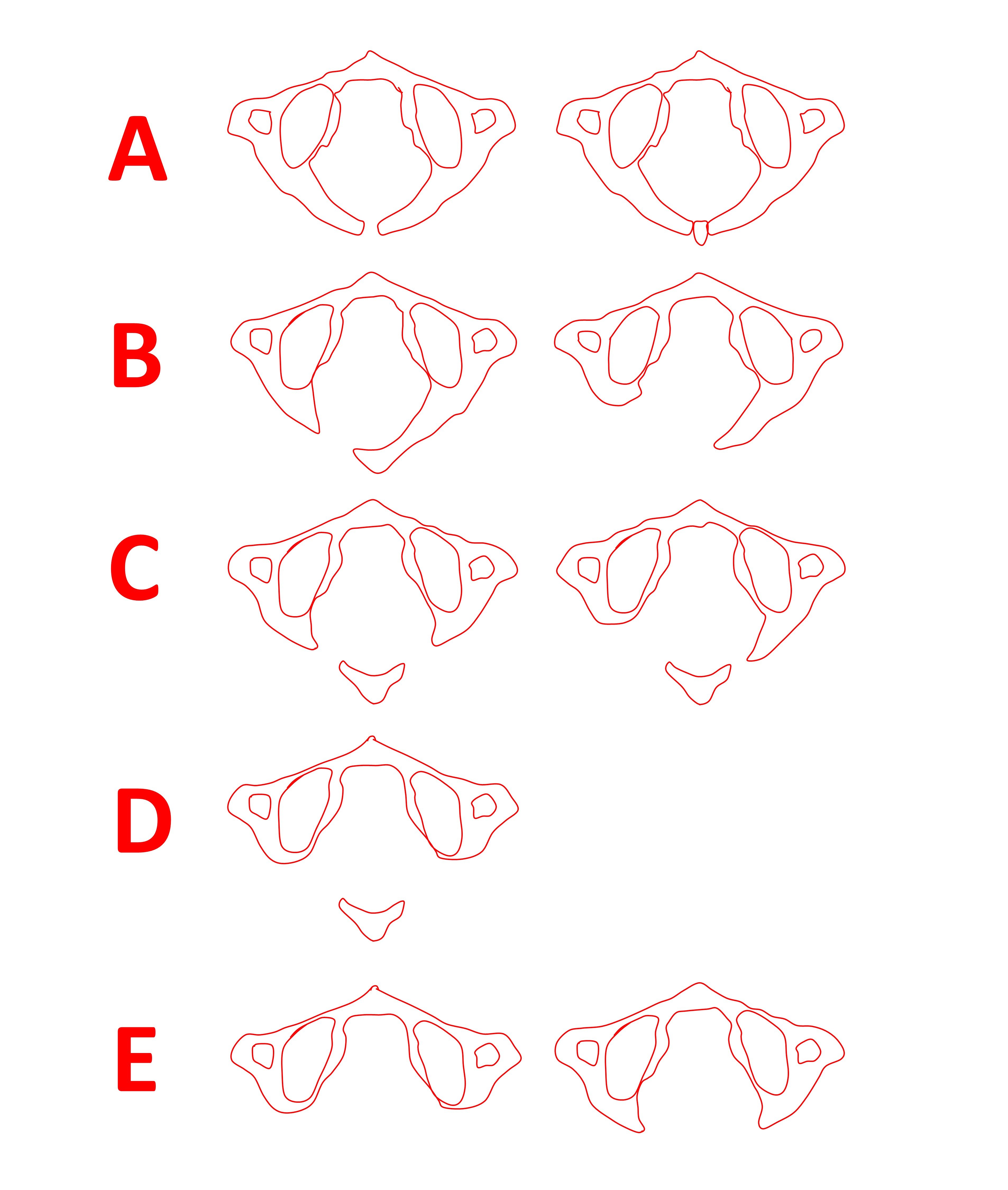
Based on Currarino and coworkers [6].
Figure 2. Currarino classification.Type A: failure of posterior midline fusion of the two hemiarches; type B: unilateral defect; type C: bilateral defects; type D: absence of the posterior arch, with persistent posterior tubercle; type E: absence of the entire arch, including the tubercle.
DISCUSSION
Anatomical variations and defects of the skeletal system often arise due to disturbances of ossification. Posterior midline clefts of the atlas, rachischisis or spina bifida occulta, are different since they are a developmental failure of chondrogenesis. During dissection of 1613 atlases Geipel noticed that 4% had posterior midline cleft. The majority of his cases (97%) were median clefts. The remaining 3% of cases were located laterally at the level of the vertebral artery sulcus [7, 8].
In the embryological period atlas is formed from three primary ossification centers: an anterior center developing into the anterior tubercle and two lateral centers giving rise to the lateral masses and posterior arch. In approximately 2% of the population, an additional ossification center may arise in the posterior midline, therefore forming into a posterior tubercle. Fusion of ossicles usually occurs during age 3 to 5 years. Incomplete posterior fusion may even be normal in children up to 10 years old [9].
Congenital anomalies of the posterior atlas arch can be classified according to a system proposed by Currarino and coworkers (Figure 2). They can be asymptomatic or present with neck pain, stiffness, and various chronic and acute neurological symptoms [6].
Type A is the common (approximating 80% of cases) type of anomaly and is encountered in 4% of the general population. In contrast, all other morphological types (B to E) are encountered in only 0.69% of the population [9]. This case also reports a type A anomaly, which is the most common.
One of the major concerns regarding posterior clefts is the differential diagnosis with Jefferson burst fracture. This is important to proceed to definite management, which differs between the two conditions. In the case of the midline clefts, when ligamentous and bony injury has been excluded by imaging techniques, management is usually symptomatic with simple analgesics. On the other hand Jefferson fracture treatment consists of external immobilization of the cervical spine with a sternal occipital mandibular immobilization brace or Halo fixation vest for up to 16 weeks [10].
Differentiation of the developmental anomalies from burst fractures of the atlas can be made by inspection of the lateral cervical and open-mouth radiographs and confirmed by CT. On the lateral radiograph the cortical bone of the anterior arch may be absent or indistinct when a cleft is present [11]. Linear tomography may further reveal smooth corticated margins, which contrast with the sharp non-corticated appearance of a fracture [12].
Although, congenital anomalies are benign they frequently occur with various combinations of neural abnormalities, suggesting that an interrelationship may exists. The neurological symptoms may include weakness in the four limbs, acute neurologic deficits such as transient quadriparesis, paraparesis, Lhermitte's sign, chronic neck pain, and headache [13, 14, 15]. This anomaly is also commonly seen in gonadal dysgenesis, Klippel-Feil syndrome, Arnold-Chiari malformations, and Turner and Down syndrome [8].
Sometimes bony projections of the type A cleft defect may become symptomatic without exacerbating factors (degeneration, atlanto-axial instability, trauma). The possible explanation is that bony expansion of the posterior hemiarches is pulled by ligamentous and muscular structures that normally insert on the posterior tubercle of the atlas [16]. Surgery is the treatment of choice in symptomatic cases by excision of the posterior arch. This is performed because a trivial trauma, such as a fall when walking, can precipitate severe neurologic deficits and even respiratory distress [17].
Hegazy stated that the defect in vertebral arch similar to found in our case could be due to developmental failure of fusion of the vertebral arch halves [18]. He added that it mostly affects the lumbosacral region. However, it is a rare anomaly in cervical vertebrae. It is called spina bifida. It is either not manifested called spina bifida occulta or associated with protrusion of meninges or neural tissue noticed seen as a bulge on the back of vertebral column. Moreover, the foramen transversarium found normally in cervical vertebrae represents a separation between the original transverse process and the costal element caused by presence of vertebral vessels.
CONCLUSIONS
Awareness of posterior midline clefts is important for proper differential diagnosis in cases of spinal trauma. When spinal trauma has been excluded the patient should be managed conservatively with the exception of symptomatic cases. It is important to consider that this anomaly can be associated with several genetic anomalies.














