A 13-year-old Spanish girl consulted because she had observed a nontender swelling on the palate. The patient's medical history was unremarkable. She visits her dentist every year and has had her premolars and molars sealed in the past. On physical examination, her vital signs were normal and the entirety of her physical examination was normal except her oropharynx. Throat examination revealed a 2 x 1.25 cm midline hard palate swelling that was bony hard in consistency and covered by normally appearing oral mucosa (Figure 1). It was diagnosed as a torus palatinus (TP). The patient was unaware of its previous presence and denied being informed about it by her dentist on any visit. The evolutionary prognosis of the TP was explained to the patient and parents and reassured about it to avoid any anxiety or unnecessary investigation. The patient is currently 16 years old, remains asymptomatic, and the TP has not increased in size.
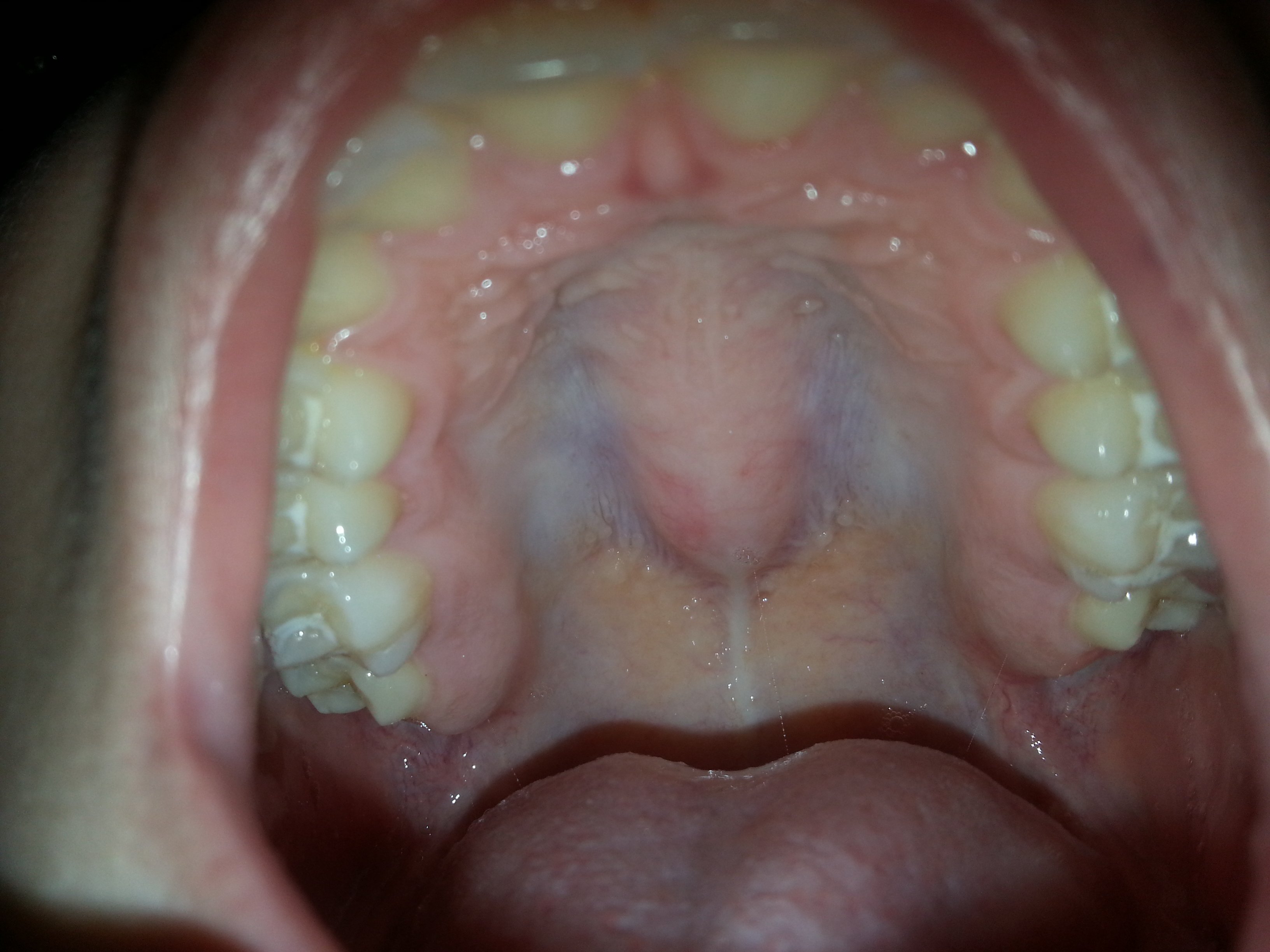
Figure 1. Midline hard palate nontender swelling that was bony hard in consistency and covered by normally appearing oral mucosa. Premolars and molars were sealed.
Masses and mass-like lesions of developmental and genetic origin may affect the pediatric craniofacial skeleton. They represent a major challenge in clinical practice because they can lead to functional impairment, facial deformation, and disfigurement. TP is a bony protuberance located at the midline of the oral surface of the hard palate and can vary considerably in size and shape. Although TP is clinically present around the age of 20 years, they are thought to be detectable during infancy too. TP is considered to be a slow-growing benign lesion that can take decades to grow into a noticeable size and patients generally do not report them as they are asymptomatic [1]. TP is frequently identified on CT scans, where it appears as a bone protuberance in a typical location with a density similar to that of compact bone. This complementary exam is only needed in cases in which possible complications such as pathological fractures and necrosis must be diagnosed or for diverse dental planning. MRI is not an imaging method of choice to identify TP, nor is it used for diverse dental planning [1, 2].
Prior population studies report a widely varying prevalence of TP with a range of 2-67% and suggest differences in prevalence among sexes and populations, occurring most frequently in females and individuals with Asian and Inuit ancestry [3]. A recent study by El Sergani et al. [4] with 1102 adults found that individuals of East Asian ancestry showed the highest prevalence of TP (20%), while individuals of West African ancestry displayed the lowest prevalence (10%). The prevalence in individuals of European ancestry was 18.6%. In males, the prevalence of TP was 5.8-6.2%, and no significant differences were found among ethnicities. Females had a significantly higher rate of TP than males across all three ancestral groups, with East Asians having the highest rate (34.7%), followed by Europeans (24.9%) and West Africans (15.2%). In addition, morphological findings were found in an ethnicity-specific manner in females; the presence of TP was associated with shorter sagittal and wider transverse dimensions of the dental arch. These shape differences were present in East Asians and West Africans, but not in Europeans.
The pathogenesis is not well-understood and appears to be a complex interplay of environmental, genetics (multifactorial inheritance), and biomechanical (occlusive biting forces; dental arch shape) factors [3, 4, 5].
Although TP usually have no clinical significance, they can be a cause for major patient and parental concern. Since the lesions are benign and usually asymptomatic treatment is not warranted. In case of discomfort, prosthetic treatment, or need for autogenous bone grafting, surgical removal can be performed [1, 3].
In conclusion, TP is a common benign exophytic growth in the midline of the bony palate, but its observation in pediatric patients is infrequent. These patients should be reassured about it when incidentally found to avoid any anxiety or unnecessary investigation.














