1. INTRODUCTION
Epithelioid sarcoma (ES) is a rare and aggressive soft tissue sarcoma of unknown histogenesis, which can be distal or proximal. The classic form (distal-type) of epithelioid sarcoma mainly occurs in teenagers and young adults. Proximal type epithelioid sarcoma (PES) is a rare variant of conventional or classic epithelioid sarcoma, described by Guillou et al in 19971 [1]. PES is mainly seen in axial locations, pelvic or genital regions in patients middle-aged or older. PES is more aggressive than classic epithelioid sarcoma, with tendency to distant metastasis [2]. The survival rate of patients with ES is low, ranging from 25% to 70%, as reported by various studies [3]. Proximal epithelioid sarcoma of the vulva is an extremely rare, having reported less than 50 cases in the English literature with frequent recurrences due to its aggressive behaviour [4]. Due to its rarity, it can pose a diagnostic challenge, often misdiagnosed as a benign lesion, which leads to diagnostic and therapeutic delays, as occurred in our case. We present a case of proximal epithelioid sarcoma of the vulva with a favorable response to treatment by surgical excision and adjuvant radiotherapy.
2. CASE REPORT
A 59-year-old postmenopausal woman with no personal history of interest, no allergies, no toxic habits, and no family history of pathology. Her obstetric history included: menopause at age 55, gesta 3, para 3, and laparoscopic bilateral tubal ligation. The patient presented a progressively growing mass on the left labia majora that had been developing for a few months of evolution. Gynaecologic examination revealed a 2 cm mobile and painless mass that was not attached to deep planes and was not associated with skin ulceration nor did it show right inguinal adenopathies. The mass was excised 6 months later with suspicion of a lipoma. By then it measured 4 cm in its greatest dimension and was relatively well circumscribed. Multiple small whitish-gray tissue fragments that together measured 5 x 4 cm were received for histological study.
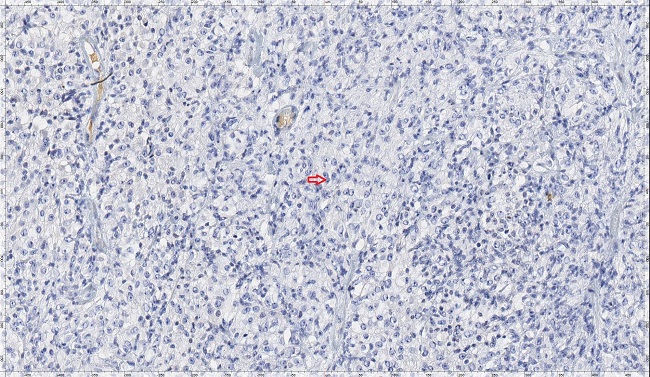
Microscopically, the sample corresponded to fragments fibro-fatty tissue occupied by a tumor highly cellular that growed in a diffuse pattern, made up of cells with extensive, eosinophilic cytoplasm and large rounded nuclei, with mild anisokaryosis, sometimes with an evident nucleolus, distributed in the form of a sheet. There were areas where the cells took on a somewhat rhabdoid pattern and there were some multinucleated giant tumor cells (Figure 1). In some areas the cells showed smaller size and more spindle cell shapes. We identified 7 mitoses for every 10 high-power fields. No extensive necrosis was observed. No evident vascular, adipocyte or muscular differentiation was identified. With immunohistochemical techniques, tumor cells express vimentin, EMA, cytokeratin AE1-AE3 (Figure 2), in a globular cytoplasmic form and do not express INI-1 in the nucleus (Figure 3). All tumor cells were negative for S-100, CK 8/18, CK-19, Melan A and HMB45, CD68, Actin, desmin, myogenin, MyoD1 and CD34. The proliferative rate with Ki 67 was 20% in the most active areas. The histopathological diagnosis was soft tissue of the vulvar region with proximal epithelioid sarcoma.
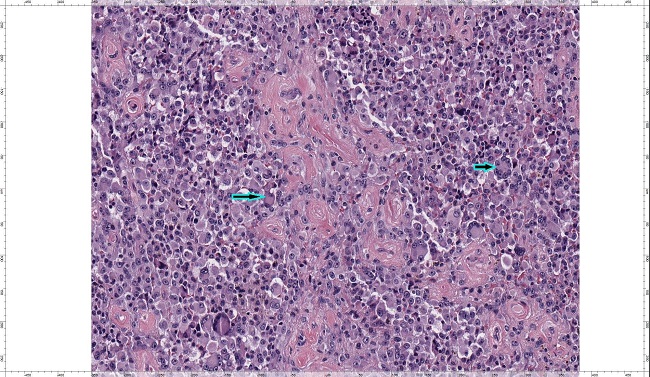
Figure 1: Microscopic image of a proximal-type epithelioid sarcoma of the vulva showing sheets of large round or polygonal cells with prominent nucleoli with areas where the cells acquired a somewhat rhabdoid pattern (long arrow) and some multinucleated giant tumor cells (short arrow). Haematoxylin and eosin 20x.
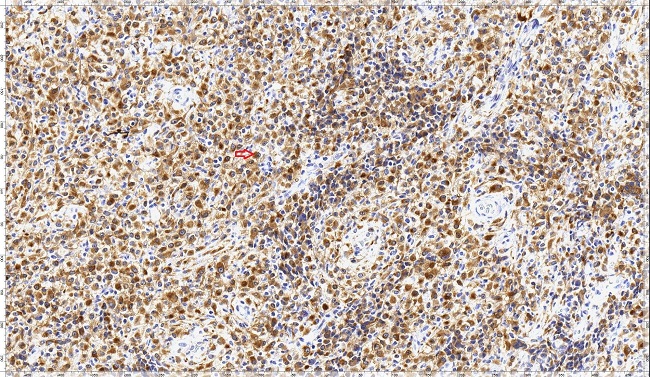
Figure 2: IHC results. Tumor cells showing intense and diffuse expression of AE1/AE3 cytokeratins (short arrow).
Given this diagnosis, the patient was re-evaluated and an extension study was carried out with imaging techniques. One month after surgery, the tumor measured 4.5 x 3 cm, reached to the upper third of the left labia majora more than 1cm from the midline and seemed to infiltrate deeply. The determination of serum tumor markers (CEA-5ng/ml, SCC-1.5 U/ml, and CA 125-15 U/ml) were normal. Magnetic resonance imaging (MRI) demonstrated a well-circumscribe 4 x 1.5 x 2 cm lobulated, subcutaneous soft-tissue tumor, displaying low signal intensity on a T1-weighted (T1W) sagittal image, a high signal intensity on a T2W fat suppression axial image. The CT-thorax-abdomen-pelvis showed no signs of distant spread. Left hemivulvectomy was performed, which showed a remnant of epithelioid sarcoma 2 mm from one of the lateral surgical margins, and bilateral inguinal lymphadenectomy with 25 lymph nodes free of metastases.
The patient received adjuvant external pelvic radiotherapy and brachytherapy in the vulvar bed. External radiotherapy at the level of the pelvis, the patient received 24 sessions for 5 weeks, divided into 5 weekly sessions, 2Gy/session, total dose 48Gy in a linear accelerator with a multileaf collimator using an isocentric technique formed with 18MV photons. Subsequently, she received complementary brachytherapy treatment with microSelectron HDR/Ir-192 in 6 sessions using a Freiburg Flap-type applicator with 4 plastic tubes. She received 3.5 Gy/session prescribed 0.5 cm from the applicator above the surface of the vulvectomy bed. As toxicity, she presented grade 2-3 radiodermitis that improved with nursing care and analgesia.
Currently, 3 years after diagnosis, the patient is in good condition, continues to be followed up by the gynecology service and has not shown signs of tumor recurrence.
3. DISCUSSION
Proximal-type epithelioid sarcoma (PES) of the vulva is an extremely rare malignant tumor of the soft tissues with frequent recurrences due to its aggressive behaviour [5]. The mean age of diagnosis is around 35 years old, similar to other sarcomas [6]. The survival rate of patients with epithelioid sarcoma is low, ranging from 25% to 70% [3]. The labia majora are the most frequent site of appearance in the vulva, both superficial and deep tissues and manifests as a nodular or multinodular tumor [7]. Clinically it can be confused with benign conditions such as infectious granuloma, fibrous histiocytoma, Bartholin's cyst, fibroma, teratoma or lipoma, causing delays in diagnosis and treatment [8], as occurred in our case. It usually presents as a firm, slow-growing, painless nodule deep in soft tissue. The gross appearance of proximal epithelioid sarcoma is variable, but it usually presents as a firm, whitish tumor with several well-defined satellite nodules and, occasionally, foci of necrosis and/or haemorrhage [9].
Histologic features of this tumor include prominent epithelioid cells and the appearance of rhabdoid features with marked nuclear atypia. Its resemblance to epithelioid or squamous cells makes diagnosis challenging [4]. Histologically, PES of the vulva must be distinguished from other neoplastic tumors such as primary/metastatic poorly differentiated carcinoma, malignant extrarenal rhabdoid tumor, rhabdomyosarcoma, malignant melanoma, synovial sarcoma, extraskeletal myxoid chondrosarcoma, epithelioid leiomyosarcoma, angiomatoid epithelioid sarcomas, desmoplastic small round cell tumor, and rhabdomyosarcoma [9]. The histological characteristics that suggest a worse prognosis are tumor greater than 3 centimeters in diameter, vascular invasion, and high mitotic index greater than 2 per 10 high-power fields, deep location, and/or focal necrosis [3, 10].To do this, we must recognize its histopathological, immunohistochemical and molecular characteristics. Among the soft tissue tumors, ES is a pitfall in morphologic diagnosis. It can be diagnosed only through immunohistochemical staining or other ancillary studies. In many cases, however, the immunohistochemical findings overlap and frequently have vague differentiation. Immunohistochemistry (IHC) studies usually reveal ES cells with characteristics of both mesenchymal and epithelioid cells. Mixed positive staining for epithelial markers (EMA and cytokeratins) vimentin, and CD34, helps differentiate ES from carcinoma. The epithelioid sarcoma is also negative for staining S100, CD31 and desmin [11]. The characteristic immunophenotype of epithelioid sarcoma is loss of nuclear immunoreactivity for INI-1. This is related to the biallelic inactivation of the SMARCB1/ INI1 tumor suppressor gene, which is located on chromosome 22q11.2 [12]. It is reported that SMARC1/INI1 (integrase interactor 1) loss is seen in over 90% of ES, both distal and proximal type. INI1 expression is retained in a few patients, so the diagnosis of ES should always be made with caution.
The treatment of proximal epithelioid sarcoma of the vulva is not well defined, but surgical resection with margins greater than 2 centimeters is recommended, similar to the treatment of extragenital epithelioid sarcoma [3, 10]. The width of the free margins is the main risk factor for local recurrence, due to the possibility of the presence of satellite lesions around the primary tumor [10]. Resection of suspected inguinal lymphadenopathy has also been recommended, but there is no evidence showing any beneficial effect in reducing the frequency of recurrences8. Adjuvant chemotherapy has shown quite modest results, which is why it is only recommended in cases of disseminated metastatic disease, more studies are needed to determine its therapeutic relevance in proximal epithelioid sarcoma [3].
Adjuvant radiotherapy is recommended for high-grade tumors or those with inadequate surgical margins. Different studies seem to describe a significant reduction in tumor recurrences after the application of radiotherapy, in such a way that the potential benefit of an aggressive multidisciplinary treatment from the beginning would be recommended.
The importance of identifying this subtype of SE lies in its aggressive behavior. In our case, the patient responded well to adjuvant RT, eradicating the local lesion without developing metastatic lesions.
In conclusion, proximal epithelioid sarcoma of the vulva is a very rare tumor that presents a diagnostic challenge. Due to its low incidence, there are no diagnostic algorithms or specific recommendations. The histopathological study is the only useful and accurate diagnostic method, immunohistochemical techniques being necessary for its correct affiliation. The suggested treatment is total resection of the tumor with wide margins. Due to the high rates of local recurrences and distant metastases, close follow-up of cases is necessary to anticipate recurrences and a fatal outcome.