My SciELO
Services on Demand
Journal
Article
Indicators
-
 Cited by SciELO
Cited by SciELO -
 Access statistics
Access statistics
Related links
-
 Cited by Google
Cited by Google -
 Similars in
SciELO
Similars in
SciELO -
 Similars in Google
Similars in Google
Share
Archivos Españoles de Urología (Ed. impresa)
Print version ISSN 0004-0614
Arch. Esp. Urol. vol.58 n.1 Jan./Feb. 2005
International Section
EXTRAMAMMARY PAGET'S DISEASE OF SCROTUM.
A CASE WITH LOCAL LYMPH NODE METASTASIS.
David Parada1, Otto Moreira2, Carmen López1, Jhonny Rodríguez3, María Elena Marín4 y Rosa M. Farías5.
Service of Pathology1, Vargas Hospital. Caracas, Venezuela.
Service of Urology2, Vargas Hospital. Caracas. Venezuela.
Service of Surgery3, Vargas Hospital. Caracas, Venezuela.
Service of Infectology4, Vargas Hospital. Caracas, Venezuela.
Internal Medicine5. Caracas, Venezuela.
Summary.- OBJETIVE: We describe the clinical, histological and immunohistochemical studies in a case of extramammary Paget's disease localized in the scrotum with lymph node inguinal metastasis.
METHODS/RESULTS: A 80-year old man consulted with a one-year history of a pruritic erythematous skin rash of the scrotum. Physical examination showed demarcated erythematous lesion involving the scrotum and right inguinal adenopathy. Final histological examination revealed extramammary Paget's disease with inguinal metastasis.
CONCLUSION: Extramammary Paget's disease of the scrotum is a rare disease. This pathological condition may spread to dermal region and the regional lymph nodes. Although genitourinary cancer may accompany scrotal extramammary Paget's disease, an extensive search for cancer may be unnecessary..
Key words: Scrotum. Paget's disease. Extramammary. Carcinoma In-Situ. Immunohistochemical.
Resumen.- OBJETIVO: Describimos los estudios clínicos, histológicos e inmunohistoquímicos en un caso de enfermedad de Paget extramamaria localizada en el escroto con metástasis a los ganglios linfáticos inguinales.
MÉTODOS/RESULTADOS: Una paciente de 80 años de edad consultó por una lesión eritematosa pruriginosa del escroto de un año de evolución. El examen físico mostró una lesión eritematosa demarcada que involucraba el escroto y adenopatía inguinal derecha. El exámen histológico final demostró enfermedad de Paget extramamaria con metástasis inguinal.
CONCLUSIÓN: La enfermedad de Paget extramamaria del escroto es una rara entidad. Esta condición patológica puede invadir la región dérmica y los ganglios linfáticos inguinales. Aunque neoplasias genitourinarias pueden acompañar la enfermedad de Paget exramamaria, una búsqueda extensa para cáncer puede ser innecesaria.
Palabras clave: Escroto, enfermedad de Paget, extramamaria, Carcinoma In-Situ, inmunohistoquímica.
Address for Correspondence
David Parada D, MD, MsC, PhD.
Department of Pathology.
Vargas Hospital.
San Francisquito a Monte Carmelo
Esquina El Recodo, San José
Apdo. 1010, Caracas. Venezuela.
e-mail: parada@cantv.net
Acepted for publication: October 21st, 2004
INTRODUCTION
Extramammary Paget's disease (EMPD) is an intraepidermal adenocarcinoma initially reported by Crocker in 1889 (1), who described a man with an eczematoid rash of the penis and scrotum. Although the male genitalia were the first extramammary site described, they represent a rare anatomical location with few cases reported. Compared with Paget's disease of the breast, which is invariably accompanied by underlying breast cancer, extramammary Paget's disease may not be associated with underlying malignancy (2).
The scrotum is an uncommon site to the presentation of extramammary Paget's disease (3). This intraepidermal malignancy rarely invades the dermis, and spread to the local inguinal lymph nodes or remote sites, and only few cases have been reported (3,4). We describe the clinical, histological and immunohistochemical studies in a case of scrotal EMPD with dermal invasion and lymph node inguinal metastasis.
CASE REPORT
A 80-year old man presented to our institution with one-year history of a pruritic erythematous skin rash of the scrotum. Physical examination was unremarkable except for a well demarcated erythematous lesion involving the scrotum, with focal ulceration (Figure 1 A,B). Mobile, non-dolorous right inguinal adenopathy was evident. Preoperative scrotal skin biopsy confirmed extramammary Paget'S disease and the patient underwent evaluation for internal malignancy. Prostate specific antigen, alpha-phetoprotein and carcinoembryonic antigen were normal. Transrectal prostate ultrasound, cystoscopy, abdominal CT, esophagogastroduodenoscopy, colonoscopy and chest x-ray were performed. Colonoscopy showed benign tubular adenoma and diverticular disease. The results of all other studies were negative. The patient was offered resection with right superficial lymph node dissection and skin grafting of the involved area. Follow-up at 6 months revealed no signs of recurrent disease.

FIGURE 1. A,B. Preoperative appearance of extramammary Paget's disease of scrotum.
C,D. Scrotectomy specimen with erythematous patch and pale areas.
MATERIAL AND METHODS
The scrotectomy specimen was received fresh and measured 10.5 x 6.3 x 1.9 cm. At its center there was an erythematous patch that measured 6.5 cm in maximal diameter, the surface was irregular with areas of pale induration (Figure 1 C,D). Right inguinal superficial lymphadenectomy was also obtained and dissection evidenced three lymph nodes, the greater 2 x 1.5 cm, with irregular external surface. Cut sections showed homogeneous aspect with focal hemorrhage. Sections were taken from the lesion and the lymph nodes, fixed in 10% buffered formalin, processed in a standard fashion, and stained with hematoxylin-eosin. Immunohistochemistry on paraffin-embedded tissue was performed with the following antisera: Cytokeratin 7 (CK7, diluted 1:50; Dako Corporation, Carpinteria, Calif.), Carcinoembryonic antigen (CEA, diluted 1:100; Dako Corporation, Carpinteria, Calif.), Cytokeratin 20 (CK20, diluted 1:50; Dako Corporation, Carpinteria, Calif.), Epithelial Membrane Antigen (EMA; diluted 1:50; Dako Corporation, Carpinteria, Calif.), HMB-45 (prediluted; Dako Corporation, Carpinteria, Calif.), S-100 Protein (S- 100; diluted 1:200, Dako Corporation, Carpinteria, Calif.) and Prostate Specific Antigen (PSA; prediluted; Dako Corporation, Carpinteria, Calif.).

FIGURE 1. C,D. Scrotectomy specimen with erythematous patch and pale areas.
RESULTS
A-) Scrotal skin biopsy:
Histological examination revealed focal areas of epithelium containing nests and singly arranged large cells with pale staining cytoplasm and hyperchromatic nuclei containing occasional prominent nucleoli (Figure 2 A,B). The surrounding epithelium in these areas showed no evidence of atypia and demonstrated normal epidermal maturation. Immunohistochemical stains for CK7, EMA and CEA were strongly expressed in neoplastic cells; normal epithelial cells were negative (Figure 2 C-F). Stains for CK20, HMB-45, S100, and prostate-specific antigen were completely negative. These histological and immunohistochemical findings supported the diagnosis of extramammary Paget's disease.
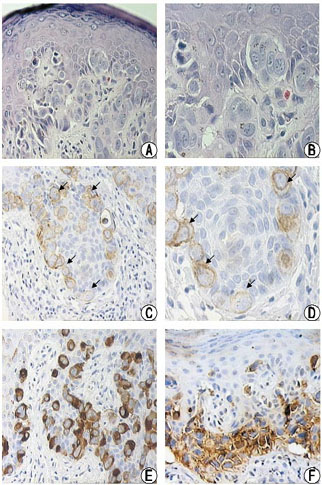
FIGURE 2. Scrotal extramammary Paget's disease.
A,B. Histological examination showing nests of neoplastic
epithelium and individual large cells with pale cytoplasm
and hyperchromatic nuclei (H-E, x100 and x400).
C,D. Cytokeratin 7 expression in neoplastic cells
(Black arrows, DAB, x200 and x400). E. EMA reactivity,
the neoplastic cells revealed a strong immunoreactivity
(DAB, x200). F Carcinoembrionic antigen showed positivity
in tumoral cells (DAB, x200).
B-) Scrotectomy and right lymph node dissection:
Additional to the previously described findings in scrotal skin biopsy a moderately differentiated invasive adenocarcinoma at the dermis, epidermis and sweat glands was observed. Two lymph nodes showed metastatic adenocarcinoma. Immunohistochemical reaction in both specimens (scrotectomy and lymph node) was also similar. The final diagnosis was as extramammary Paget's disease with lymph node metastasis.
DISCUSION
Extramammary Paget's disease is a rare neoplastic condition, in which there is intraepithelial infiltration by neoplastic cells showing glandular differentiation (2). This disease represents approximately 0.2 % of vulvar and penoscrotal malignancies (5) and only some case reports addressed scrotal extramammary Paget's disease (3,4,6). Usually, scrotal EMPD presents as erythematous, pruritic and indurate lesions that may ulcerate and discharge (3,4). Our patient showed symptoms of scrotal EMPD characterized by pruritic erythematous scrotal lesion. These findings are not specific of EMPD and can be mistaken, for example, with micotic infection. A long delay from the onset of symptoms to diagnosis and treatment is frequent (6). Nevertheless, this interval has not been correlated with the progression of the disease, suggesting that scrotal disease is distinctly individual in its presentation, and long-term follow-up is necessary (6).
Unexpected finding in our case of scrotal EMPD was dermal invasion. Even more surprising was adenocarcinoma in the superficial inguinal lymph nodes, implying local metastasis. This unusual finding can be explained by colonization of neoplastics cells within the epidermis and, with time, progress from intraepidermal neoplasia (in situ disease) to dermally invasive adenocarcinoma, these findings are similar to invasive malignant melanoma arising from superficial spreading malignant melanoma (7). Dermal invasion is thought to be present in up to 20% of cases of primary intraepidermal EMPD, although it might not be detected if sampling is not rigorous (8). Primary EMPD has a worse prognosis in the presence of dermal invasion, and it has been suggested that the prognosis depends on the depth of dermal invasion (8).
The differential diagnosis of scrotal EMPD include various pathological condition in which "pagetoid spread" is seen. These pathological conditions comprise superficial spreading malignant melanoma, Bowen's disease and mycosis fungoides (2). Paget's disease can be misdiagnosed as squamous cell carcinoma in situ (Bowen's disease); however, intracellular mucin, signet cells, and glandular structures are useful features to distinguish Paget's disease. In cases where morphological features of glandular differentiation are absent, immunohistochemical staining (Cam 5.2, EMA, CEA positive in Paget's disease) will usually solve the problem (2,9,10). Superficial spreading malignant melanoma shows prominent nesting along the dermoepidermal junction whereas the cells in Paget's disease are usually distributed more diffusely. In difficult cases immunohistochemical markers as S100 and HMB-45 can help to reach an adequate final diagnosis (2,10). Finally, mycosis fungoide have characteristic features with large convoluted, cerebriform, nuclei set in pale cytoplasm and immunohistochemical staining for T cell markers is positive in mycosis fungoides (2).
In conclusion, extramammary Paget's disease of the scrotum is an uncommon intraepithelial adenocarcinoma, which mimic inflammatory and infective skin diseases. This neoplasm can invade the dermal region and lymph node metastasis. The glandular differentiation is indicated by morphological appearances and positive immunohistochemical staining for glandular cytokeratins, EMA and CEA. The histological and immunohistochemical studies provide for support for the view that most cases show an intraepidermal origin, with a small proportion having an epidermotropic origin from an associated in situ or invasive neoplasm in an organ with contiguous epithelium.
BIBLIOGRAFÍA y LECTURAS RECOMENDADAS (*lectura de interés y **lectura fundamental)
*1. CROCKER, H.R.: "Paget's disease affecting the scrotum and penis". Transactions of the Pathological Society of London, 40:187. 1888-1889. [ Links ]
**2. LLOYD, J.; FLANAGAN, A.M.: "Mammary and extramammary Paget's disease". J. Clin. Pathol., 53:742. 2000. [ Links ]
*3. PARK, S.; GROSSFELD, G.D.; MCANINCH, J.W. y cols.: "Extramammary Paget's disease of the penis and scrotum: excision, reconstruction and evaluation of occult malignancy". J. Urol., 166: 2112. 2001. [ Links ]
**4. VAN RANDENBORGH, H.; PAUL, R.; NAHRIG, J. y cols.: "Extramammary Paget's disease of penis and scrotum". J. Urol., 168: 2540. 2002. [ Links ]
5. ROSEN, T.: "Update on genital lesions". JAMA, 209: 1001. 2003. [ Links ]
**6. LAI, Y.L.; YANG, W.G.; TSAY, P.K. y cols.: "Penoscrotal extramammary Paget's disease: A review of 33 cases in a 20-year experience". Plast. Reconstr. Surg., 112: 1017. 2003. [ Links ]
7. EVANS, A.T.; NEVEN, P.: "Invasive adenocarcinoma arising in extramammary Paget's disease of the vulva". Histopathology, 18: 355. 1991. [ Links ]
*8. GOLDBLUM, J.R.; HART, W.R.: "Vulvar Paget's disease: a clinicopathologic and immunohistochemical study of 19 cases". Am. J. Surg. Pathol., 21: 1178. 1997. [ Links ]
9. QUINN, A.M.; SIENKO, A.; BASRAWALA, Z. y cols.: "Extramammary Paget disease of the scrotum with features of bowen disease. A case report and review of the literature". Arch. Pathol. Lab. Med., 128: 84. 2004. [ Links ]
*10. NAKAMURA, G.; SHIKATA, N.; SHOJI, T. y cols.: "Immunohistochemical study of mammary and extramammary Paget's disease". Anticancer. Res., 15: 467. 1995. [ Links ]














